Publication Information
ISSN 2691-8803
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2019
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Typhoid and Paratyphoid Fever in Sub-Saharan Africa: Epidemiological Aspects, Therapeutic Remedies and Practices
H Blaise NGUENDO YONGSI*
Institute for Population Studies (IFORD)/University of Yaoundé II &School of Health Sciences/Catholic University of Central Africa –Cameroone
Received Date: April 27, 2020; Accepted Date: May 04, 2020; Published Date: May 13, 2020
*Corresponding author: H Blaise NGUENDO YONGSI, Institute for Population Studies (IFORD)/University of Yaoundé II &School of Health Sciences/Catholic University of Central Africa–Cameroone. Email: nguendoyongsi@gmail.com
Citation: Nguendo Yongsi HB (2020) Typhoid and Paratyphoid Fever in Sub-Saharan Africa: Epidemiological Aspects, Therapeutic Remedies and Practices. Adv in Pub Health, Com and Trop Med: APCTM-109.
Abstract
Background: Typhoid fever is a contagious toxi-infection due to Salmonella Enterica serotypes Typhi (Bacillus of Eberth) and Paratyphi A, B or C. These serotypes are strictly adapted to humans and make this enterobacterium a classic pathogen associated with danger fecal. Typhoid fever represents a burden on global health, especially in developing countries where health conditions are outdated.
Objectives: This study aims to measure the prevalence, to understand the routes and behaviors of patients in the city of Dschang in the face of typhoid fevers.
Method: This is a cross-sectional epidemiological study focused on individuals aged 5 years and over. This study was used in socio-environmental and medical surveys.
Results: Salmonella typhi and Paratyphi A, B, C were isolated in most of the samples, making it possible to confirm the exposure to typhoid fever. 317 individuals were confirmed, reflecting a prevalence of 18.3%. The 15-44 age group was the most represented, 42.8% overall, with a male / female sex ratio of 0.9 and a median duration of 6 days between the onset of symptoms and the consultation. Examination of the patients revealed that for most of them the onset was abrupt, with plateau fever, headache, and abdominal pain. Faced with the disease, patients resort more to ethnomedicine which offers therapies based on leafy leaves / stems and fruit, for oral administration.
Conclusion: The extent of typhoid and paratyphoid fevers requires individual and collective hygiene measures. Likewise, the scale of self-medication and ethno medicine requires the adoption of a health education action plan, in particular for supervised management of anti-typhoid therapeutic practices in the city.
Keywords: Cameroon; Dschang; Therapeutic Practices; Typhoid and Paratyphoid Fevers; Use of Care
Introduction
Typhoid fever (from the Greek tuphos, torpor) or abdominal typhus is an acute febrile infectious disease with fatal potential, caused by a bacterium of the Enterobacteriaceae family, of the genus Salmonella, and whose responsible species are: Salmonella Enterica-typhi (Bacillus d ‘Elberth) or Salmonella paratyphi A, B, C. It is characterized by fever on a plateau of 40 ° C, shivering, anorexia, lenticular pink spots, dry and red tongue and abdominal pain [1]. Typhoid and paratyphoid fevers are very old systemic bacterial infections [2, 3]. Considered throughout the ages and continents as a reflection of poor living conditions and food hygiene [4,5], the proposed medications have combined preventive measures (fight against fecal peril through the distribution of quality water bacteriologically controlled, wastewater treatment, generalization of sewage, pasteurization of food, disinfection of linens, anti-typhoid vaccination) [6,7], and curative measures (introduction of chloramphenicol in 1948 and treatment with well-dosed and well-developed antibiotics (aminopenicillins) from the early 20th century [8-10]. During the 20th century, progress made in their therapeutic management (introduction of fluoroquinolones and cephalosporins) has made it possible to reduce the complications of the disease (intestinal hemorrhage, intestinal perforation, peritonitis, splenomegaly, hepatomegaly) and to reduce lethality [11-13]. However, due to their size and frequency, they remain a major public health problem. In fact, it is estimated that they are responsible for 21 million cases annually with more than 200,000 deaths worldwide (the fatality rate is 16% without treatment and 1% with appropriate antibiotic therapy), and 9.8 million years lived with a disability (AVI) [14]. The reservoir is strictly human and contamination takes place through the stools of patients or healthy carriers. They are therefore diseases with oro-fecal transmission by ingestion of contaminated water or food. Like all diseases of this kind, they most often occur in areas where hygiene is precarious, and mainly affect developing countries in Asia, Africa or Latin America [15]. In developed countries, they have essentially become a pathology for the traveler returning from endemic areas or people originating from these areas [16]. Until today, this pathology still poses problems related, on the one hand, to the non-eradication of the bacteria and, on the other hand, to the ever-increasing resistance to antibiotics. If morbidity is real in all latitudes, the endemicity of these fevers is observed almost exclusively in developing countries where each individual has a one in two chance of contracting the disease due to the almost daily exposure to the pathogens in question [17]. This is the case in Cameroon where the medical literature reports that typhoid and paratyphoid fevers are after diarrhea and acute respiratory infections, the main reasons for hospital consultation [7, 18]. Although not reportable, national epidemiological data indicate that it went from 876,000 cases in 2013 to 1,401,000 cases in 2017. Despite high and constant morbidity due to co-infection with other infectious pathologies (diarrheal diseases, malaria, etc.), the typhoid endemic remains insufficiently documented in Cameroon, especially in the dimension of its therapeutic management. It is with this in mind that we have undertaken this study, the objective of which is twofold: to present the epidemiological aspects, and to identify the care trajectories and to analyze the behaviors and practices of households in the face of typhoid and paratyphoid fevers.
Materials and Method
Definition of Terms
A person was considered to have typhoid or paratyphoid fever if a fever of at least 38 ° C persisted for three days or more with laboratory confirmation by isolation of Salmonella enterica serovar typhi or paratyphi A, B, or C from clinical samples.
“Seeking care” refers to the channels used by individuals to obtain care. According to Toon and Svalastog [19], individuals make decisions regarding the use of care, developing strategies that put them in contact with various places of treatment (health centers, public markets, private clinics, traditional healers) according to a trajectory that meets the requirements of the individual and that of his social network. By resorting to care, allusion is therefore made to the types of care, better to the behaviors displayed by the populations in their quest for care. As this quest is directed towards different routes, both in the medical and geographic areas, we will speak of therapeutic routes without distinction.
Therapeutic practices, for their part, refer to the therapeutic acts performed, the nature of the care, that is to say the products used and the techniques used to overcome the disease.
Framework of the Study
The scope of this study is the city of Dschang in Cameroon, located between 5 ° 25 ‘and 5 ° 30’ of Latitude North, and between 10 ° 00 ‘and 10 ° 5’ of Longitude East (Figure 1). The city is built on the south-eastern slope of the Bamboutos Mountains and opens to the south-west by the Menoua River which flows towards the plain of Mbo. To the east, it is closed by the Bani massif which rises to more than 1920 m above sea level. Chief town of the Menoua department, Dschang covers an area of 252 km² for an estimated population of 120,207 inhabitants. The five groupings which compose it are: Foto, Foréké-Dschang, Fongo-Ndeng, Fossong-Wentcheng, Fotetsa and Dschang -urban. Dschang is influenced by the equatorial mountain climate, with anthropic vegetation, and sandy clay, ferralitic and hydromorphic soils. Secondary city, Agriculture and animal husbandry remain the favorite activities practiced both in the rural area and in the city center. Dschang does not have enough basic socio-economic infrastructure: sometimes muddy, sometimes dusty roads are dotted with informal trading posts on which fruit, vegetables and other everyday products are placed.
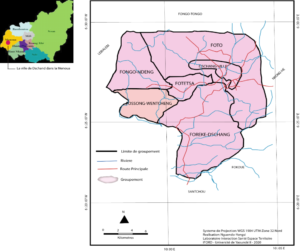
Figure 1: Location of Dschang.
Data and Collection Methods
Study Outline: This is a cross-sectional epidemiological study for descriptive purposes, carried out on the city on the initiative of the Laboratory of Health Space Territory Interactions of the University of Yaoundé II, in collaboration with the Laboratory of Climatology and Environmental Research of the ‘University of Dschang.
Case Definition and Patients: In order to minimize the risk of confusion between fevers, which are symptoms that are generally observed in the case of certain pathologies, a case of typhoid and paratyphoid fever has been defined as meeting the following clinical description: prolonged fever may be as high as 39.8-400 C, headache, abdominal pain, anorexia, constipation, myalgia, relative bradycardia, pink lenticular spots on the abdominal skin. In our study, the term “typhoid fever” was assigned to the clinical form and the serology of which was determined by the Typhidot® test. Since enteric fevers are rare in infants, the target population was any subject aged 5 years and over. So were included in the study.
Sampling and Collection Method: In order to have a real and general picture of typhoid and paratyphoid fevers, our sampling frame was made up of all the five groups that make up the locality of Dschang. However, we carried out a stratified two-stage survey: first, the health areas were selected from each group by simple random selection; then and within these health areas, we selected the households in proportion to the size of each group. A total of 1,734 households were selected. The data were collected by mixed teams (Nurses and socio-demographic interviewers) who visited the households selected to collect the data relating to the study, namely: (i) socio-demographic and environmental data for households and neighborhoods / villages, by means of a specific questionnaire on clinical data and risk factors for contamination: professional occupation, childcare arrangement in the case of a child under 6 years of age, setting and conditions of domestic and home life ( number of people living in the household, type of housing, presence of waste water and household waste, method of supply and storage of drinking water, etc.). (ii) Medical data through blood and stool samples. Initially, blood cultures and / or co-cultures positive for S. typhi and S. paratyphi were carried out. The isolation and identification of pathogens were carried out according to the usual methods (isolation on a selective Hektoen medium, identification using miniaturized identification galleries [API 20E, BioMerieux], agglutination by monovalent serum). The antibiograms were carried out by the method of diffusion in agar medium according to the recommendations of the Cameroonian Society of Microbiology. Then, the confirmation of the cases was made by the bacteriology laboratory of the Center which carried out blood samples for the Typhidot® serodiagnostic test, which is a rapid serological test (takes 3h to perform) and reliable, developed in Malaysia for detection specific IgM and IgG antibodies.
This quantitative and medical approach was supplemented by the qualitative approach, the objective of which was to capture the therapeutic remedies of individuals in the household who tested positive through questions such as: “Have you tried to treat your typhoid fever?” “If yes, who did you consult with?” “How did you manage the treatment?” “If not, why did you not consult or try to treat your typhoid fever?” Etc.
Data analysis: The data were entered on Epi Info version 7, but analyzed under Spss version 18. The Qgis software version 2.18.1 was used to carry out the cartographic distribution of the cases of typhoid fever confirmed by group. The comparisons between the groups were carried out using the Chi-square test when it was a question of qualitative variables, and using the Student’s test when it was a question of quantitative variables. The value of p <0.05 was considered to indicate a significant statistical difference.
Results
Epidemiological aspects
Clinical Features: Among the 1,734 individuals who were the subject of the medical investigation, we noted 317 affected by thyphoid fevers, representing a prevalence of 18.3%. These fevers were caused by four Salmonella serovars, strictly human, antigenically distinct but with similar pathogenic power: S. Typhi, S. Paratyphi A, S. Paratyphi B, S. Paratyphi C, all Salmonella are said to be major due to the severity of the pathology they cause (Graph 1).
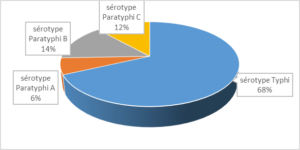
Graph 1: Distribution of Salmonella serovars involved in enteric fevers in Dschang.
Demographic and Behavioral Characteristics: Analysis shows that the 15-44 age group was the most represented, 56.6% overall, with a male / female sex ratio of 1.1 and a median duration of 6 days between the onset of symptoms and the consultation. The consumption of dairy products / ice creams, fruits and vegetables, and local sugary drinks was reported in 21.7%, 28.7% and 43.6%) of patients respectively. Many patients tested positive displayed behaviors at risk of exposure to typhoid fevers (65.9%) (Table 1). 0.83 1 0.36 0.55 (regular hand washing with soap, washing fruit / vegetables under running water, boiling drinking water, depositing household waste in closed containers, discharge of used water into gutters, use of toilets with flushing) 108 34.1 0.62 (irregular hand washing, consumption of well / spring water without boiling, rejection of household waste and waste water in the yard, use of latrines or waterproof pit toilet) 209 65.9 0.47 2 All the patients having presented several signs at the same time, we cannot have a relative frequency equal to 100%
Effective
Percentage
P value
A. Demographic characteristics
Sex
Male
165
52.0
Feminine
152
48.0
Age group (in years)
5-9
15
04.7
10-14
47
14.8
15-24
73
23.1
25-34
68
21.4
35-44
38
12.1
45-54
41
12.9
55 and +
35
11.0
Education level
Primary
83
26.2
Secondary
174
54.9
Superior
60
18.9
B. Behavioral characteristics
Food consumption1
Dairy products / ice creams (kossam, Dakéré)
69
21.7
Local sweet drinks (foléré, Ginger)
138
43.6
Fresh fruits and vegetables
91
28.7
Appropriate health behavior
Health risk behavior
C. Clinical signs observed in patients2
Functional / general signs (Fever, chills, asthenia, anorexia, myalgia and arthralgia, dissociation of pulse / temperature)
309
97.5
Digestive signs (Abdominal pain, nausea and vomiting, constipation, gurgling)
296
93.4
Physical signs (bronchial rales, jaundice, abdominal tenderness, dehydration, hepatomegaly)
81
25.6
Neurological signs (Dizziness, headache, restlessness)
73
23.0
Respiratory signs (Cough, dyspnea, ronchi)
68
21.4
Cardiovascular signs (Low blood pressure, tachycardia)
16
05.1
1 Multi-consumption situations have not been taken into account
Geographic picture of typhoid fevers and paratyphoid, an uneven spatial distribution: The calculated typhoid prevalence of 18.3% is only the average of our six groups surveyed, due to the fact that from one group to another, the prevalence rates vary (Map 2).
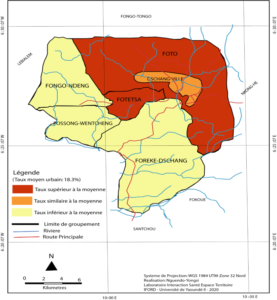
Map 2: Spatial distribution of typhoid and paratyphoid fevers in Dschang.
This map shows the uneven distribution of typhoid and paratyphoid fevers, emphasizes the heterogeneous nature of the district of Dschang on the one hand, and on the other hand the diversity of risk factors for typhoid fevers in the city. Table 2 groups together the nonparametric correlation coefficients which measure the association between the prevalence rate of typhoid fevers and the factors associated with their distribution at the district level. These results show a highly significant positive association between the risk factors and the prevalence of typhoid in the areas surveyed (Table 2). 0.351 * 0.287 * 0.426 ** 0.298 *
Risk factors associated with typhoid fevers
Nonparametric correlation coefficients
Spearman’s Rho
Kendall’s Tau
No running water (water supply dominated by wells and springs)
0.623 *
0.501 **
Wild garbage and disposal in the wild
0.769 **
0.502 **
Wastewater drainage system absent / obsolete (discharge in the yard and alleys)
Unpaved roads (dusty and / or muddy)
0.409
0.317
Domestic breeding and / or peri-domestic
0.198
0.125
Toilet / WC dominated by dry latrines
0.582 *
0.318 *
Open markets with fruit and vegetables arranged on the ground or on open-air stalls / counters
* Significant correlation at the threshold of 0.05 * *Significant correlation at the threshold of 0.01
Remedies and Therapeutic Practices
In the event of an episode of typhoid and paratyphoid fever, the decision to consult or find an antidote to combat it is immediately taken by the caregiver, as it is true that it is from the fifth day that most patients genuinely resolve to do so (Table 3). Time taken
Type of appeal
Self-medication
Modern care
Traditional medicine
Other
[1-2 days]
13 (06.1%)
04 (36.4%)
18 (25.0%)
03 (15.8%)
[3-4 days]
75 (34.9%)
05 (45.5%)
22 (30.5%)
10 (52.6%)
[5days and more]
127 (59.0%)
02 (18.1%)
32 (44.5%)
06 (31.6%)
Total
215 (67.8%)
11 (03.5%)
72 (22.7%)
19 (06.0%)
However, not all patients with enteric fevers in Dschang who have used treatment display the same therapeutic behavior. Indeed, the trajectories followed by these patients are multifaceted (Table 4).
Types of remedies
Frequency
Percentage
Self-medication only
215
67.8
§By chemotherapy
31
14.4
§Traditional
184
85.6
Modern care only
3
0.9
Traditional medicine only
48
15.1
Modern care and Traditional medicine
32
10.2
Other recourse
19
6
Total
317
100
The medications used for therapeutic purposes are different and varied (Table 5).
A-Self-medication (n = 31)
Frequency
Percentage
– Cotrimoxasole (Bactrim)
14
45.20%
– Amoxicillin
11
35.50%
– Metronidazole (Flagyl)
6
19.30%
B- Treatments followed in modern healthcare structures (n = 33)
– Infusion
2
6.10%
-Ciprofloxacin (750mg, 2 times a day for 28 days)
4
12.10%
– Cotrimoxasole (Bactrim – 4 to 6 tablets / 24 hours in adults and 50 to 60 mg / kg / day in children)
10
30.30%
– Amoxicillin (2 to 4g / day) for 14 to 21 days
7
21.20%
– Dexamethasone at a dosage of 3 mg / kg on day 1 then 1 mg / kg / 6 hours for 48 hours
4
12.10%
– Azithromycin 1g on day 1 and 500mg the following 6 days
3
9.10%
– Ofloxacin 200mg × 2 / d for 7 days
3
9.10%
C- Traditional products consumed (n = 232)
– Drinkable potion made from the leaves of Eucalyptus globulus Labill, Musa paradisaca L, and Acanthospermum hispidium. (decoction in equal proportion of the leaves of each of these plants, addition of honey and consumption at will until healing)
42
18.10%
– Drinkable potion based on Allium sativum pod, Phyllantus amarus and Allium cepa bulb (Maceration for 8 minutes of 500 g of minced garlic and two large onions in two liters of unsweetened milk and consume ½ glass three times a day until healing)
52
22.40%
– Drinkable potion based on Petroselinum crisum (Parsley) and cloves (Decoction of 5 to 6 nails and a bunch of parsley in 2 liters of water, then consumption of 1 glass 3 times / day)
26
11.20%
-Drinkable potion made from the leaves of Combretum micranthum (Quiinquéliba) and lemon (Trituration of 500 g of Quiinquéliba leaves and mixture with 3-4 lemon fruits, then drink 1 glass 3 times / day)
19
8.20%
-Drinkable potion made from Carica papaya L leaves, Psidium guajava root and stem, and Citrus lemon fruit (Boil 500 g of young papaya and guava leaves plus 5 lemons in 3 liters; then dissolve 100 g of halite. Drink 1 glass morning and evening until feeling of healing)
93
40.10%
The disease is not an essentially clinical fact in African societies. The perceptions and representations that Dschang’s patients have or have of typhoid and paratyphoid fevers suggest that traditional medicine is the only remedy (Table 6).
Types
Causes
Therapeutic attitudes
Typhoid and acute paratyphoid fevers
Mystical attack of a sorcerer
Can only be healed by healers and patriarchs
Typhoid and chronic paratyphoid fevers
Poisoning by an enemy
Consult a traditional healer to request potions / decoctions to purge the belly
typhoid and paratyphoid fevers of the “bad belly”, that is to say with digestive perforations and hemorrhages
presence of objects (animals) in the belly
Consult a sighted marabout to determine the object and remove it
fevers with vomiting, abdominal pain, and hepatovesicular complications
Caused by wizards or “four-eyed people”
Consult a traditional healer or patriarch
Comments
Epidemiological Aspects
The prevalence of typhoid and paratyphoid fevers in Dschang is slightly higher in boys. This male / female ratio of 1: 1.1 confirms the trend noted by other authors who noted a higher number of subjects in men than in women. Overall, there is a prevalence of 18.3%. Compared to that recorded in other cities such as Tlemcem, 20.7%; Lagos, 26%; Goma, 31% [20-22], this rate may seem moderate, but in the context of Dschang considered as a city, it remains high. We see that the urban advantage did not play for this type of pathology, if not very little. For several decades, cities in sub-Saharan Africa have posed serious epidemiological problems. Pathologies hitherto considered to be characteristic of rural areas, now find in the city conditions favorable to their development. This is because African cities south of the Sahara are in crisis. This crisis is manifested by the human overcrowding and the overcrowding of the habitat, the difficulties of supplying running water, the insufficiency or the defectiveness of the sanitation and household waste disposal equipment: all favorable factors or of the spread of typhoid fevers raging in endemo-epidemic mode in cities. The unequal prevalence of typhoid fevers reveals another dimension of African cities: their extreme heterogeneity. The peri-urban and urban front groups, the most affected by typhoid fevers, reveal the precariousness of living conditions and the still rural character of these areas (widespread use of surface water and wells for the consumption and washing of fruits and vegetables, defecation in the open air or in unprotected latrines, the odors attract flies and winged insects whose role in the contamination of food and in the spread of Salmonella is well known, in that they are the ones who transport germs from human faeces to food). In peri-urban groups and in the city center, the lack of an adequate evacuation system leads housewives to use the streets and the sewers as dumping grounds. And the number of toilets that do not meet the needs of the population, encourages the “windward” system which contributes to water pollution and contamination of fruits and vegetables exposed in the open air. All in all, a lack of general hygiene which combines water and faecal danger.
Therapeutic Remedies
In general, the patients’ therapeutic choices follow a pragmatic logic adapting the care provided to the characteristics of the disease: the nature, intensity, symptomatology, and perception of the disease [23]. However, in the event of a typhoid episode, not all Dschang patients display the same therapeutic behavior. In fact, of the 317 patients questioned, 298 (94.0%) said they used treatment, compared to 19 (06.0%) who said they used no treatment, but who adopted other practices. From the statements of the respondents, there is a feeling of “competence” vis-à-vis typhoid fevers. According to these respondents, it appears that treatment must first be done within the concession, and that recourse to other caregivers will come afterwards.
As a first resort, households choose self-medication (67.8%). Seen as a “profane reference system”, that is to say the personal knowledge and culture that individuals have about health and caregivers, self-medication has become an ordinary therapeutic means which individuals use to treat even serious health problems like typhoid fevers [24]. In Dschang, this type of treatment has taken two forms: self-medication by chemotherapy and traditional self-medication. The first consisted in the use of anti-typhoid drugs either directly obtained from the sellers of street drugs or from unauthorized health workers operating underground, or from the storage of therapeutic residues from previous morbid episodes, deliberately not used if symptoms improve early. The second (traditional) form consisted in the use of different potions and coctions based on vegetable products.
The second remedy consists of modern care obtained from public or private health centers where medical practice is modern medicine from diagnosis to treatment. This means concerned 01% of the patients who did it to fix themselves on the nature of the typhoid (pathogens in question), on the appropriate therapy, but especially with regard to the deterioration of the physical condition of the patient. In the context of a city like Dschang, this rate of use of 01% seems low, thus reflecting the weaknesses of the health system through (i) the insufficient institutional supply of care which poses the problem of accessibility geographic evoked in many works including those of Konèand de Bolduc et al. [25,26]; (ii) the insufficiency of personnel in quantitative and qualitative terms (certain positions such as those relating to consultations, medical analyzes, prescriptions for drugs are held by nursing assistants trained on the job). In addition to this problem of quality of services, there are shortcomings in the area of professional ethics (development of professional unconsciousness, corruption and racketeering of the sick, regular delays and absences, busyness of certain health personnel [27]. In this situation of rejection of medical ethics, the populations have lost all confidence in formal medical action.
The third remedy is traditional medicine considered to be the body of knowledge and practices explicable or not, to diagnose, prevent or eliminate a physical, mental or social imbalance, relying exclusively on lived experience and observation passed on from generation to generation, orally or in writing. More than half of the patients declared going directly to traditional healers (traditional healers) in the event of illness. Among the reasons often mentioned, the economic criteria are sometimes put forward in favor of the advantages of traditional medicine whose treatment costs are considered low. As other determinants, we can think of the gaps identified in modern health structures, beliefs and habits whose preference lies in the symbolic dimension of traditional practices that modern medicine does not integrate [28,29]. A vast field of anthropological and ethnological research has shown that in different traditional societies, the disease does not was not always seen in a rational way but considered as taking source in the world of the invisible [30]. Thus, Clements [31] classified the various causes of the disease commonly invoked in traditional societies into five main types: incorporation of an evil object, loss of a soul, possession by a spirit, violation of a prohibition, aggression against ‘a wizard. In this context of transcendent perception of most diseases, the solutions / responses envisaged to recover health are, most often, through the use of traditional therapists (healers or magicians) [32]. The latter, according to the supposed cause of the disease, proceed by rituals, incantations or administration of antidotes supposed to bring the evil out of the body or the spirit [33].
The fourth therapeutic behavior consisted in associating modern medicine and traditional medicine. This form of mixed remedy reflects the persistence of traditional practices despite the spread of modern medicine and urbanization [34]. The introduction and spread of modern medicine has certainly in many cases met with popular support, due to its relative effectiveness. However, it has not resulted in the total abandonment of traditional therapeutic practices. On the one hand because African populations, both rural and urban, remain for the most part attached to ancestral beliefs associating, implicitly or explicitly as the case may be, disease with supernatural causes [35]. On the other hand, even urbanized, traditional beliefs still remain alive, new urban dwellers importing their therapeutic practices from the countryside into the city [36]. The persistence of these beliefs is reflected today in the subdivision of diseases into two categories, moreover not completely separate: those, benign and / or well known for which the use of modern medicine is the most common solution. But when the disease worsens or when it is a disease with serious complications, the imputation to a transcendent cause takes over and it is then resorted to an initiate (marabout, healers, etc.) whose it is believed that he is the only one capable of obtaining healing [37]. So we can understand in the context of Dschang, the combination of modern medicine and traditional medicine mentioned to “enhance” the effectiveness of modern medicines. This attitude is indicative of the perceptions and representations that people in black Africa have of illness and body health. So, one goes to the hospital just to ask the doctor to alleviate or make disappear the pain caused by the disease, because the evil in itself will be really removed only by the healers and patriarchs, which as far as the cause of the disease is cultural and / or religious [38]. A category of patients declared that they did not use any treatment. But in reality, faced with illness, they engage in symbolic practices based on their perception of the illness [39]. 06% of the patients questioned admit having resorted to prayers and various sacrifices, either as the only therapeutic remedy, or in support of other therapeutic means.
Therapeutic Practices (Nature of Curative means)
The survey methodology and the categories of analysis used made it possible to distinguish three main fields: that using curative means of the biomedical type, that based on so-called traditional knowledge delivered by therapists.
Biomedical curative means include self-medication by chemotherapy and prescriptions obtained in a health facility. In detail, we notedtwo cases of hospitalization in which patients received infusions, in this case intravenous ciprofloxacin. Speaking of anti-typhoid drugs, in most cases it was more or less broad spectrum antibiotics recommended in the case of bacterial infections, and not viral. Their mode of action is essentially bactericidal. Thus, in the two remedies (self-medication and prescription by health personnel), the prescriptions related to ofloxacin or ciprofloxacin which is a first-line antibiotic. This is because its effectiveness has been demonstrated by Booker et al [40] in that its two components act in synergy by simultaneous blocking of two enzymes catalyzing successive reactions in the metabolic chain of folinic acid, essential for the survival of many microorganisms. Regarding etiological or alternative therapy, amoxicillin and Cotrimoxazole were the initial choices in the many cases of typhoid fevers. In fact, in Kinshasa, Kalunda et al. [41] have suggested its use in the treatment of typhoid. It has also been recommended as a first line for the treatment of digestive infections with minor salmonella in fragile areas / subjects [42]. Cotrimoxazole, long considered the benchmark product in the treatment of salmonellosis, retains a significant place. Metronidazole seems to have been acclaimed by the population which lends it the ability to immediately cure the disease, at the cost of confusion between temporary action on symptoms and in-depth treatment of the disease. In general, patients frequently receive several drugs simultaneously.
The second curative means practiced is phytotherapy. Herbal medicine against typhoid fevers in the first line is a living reality in African cities south of the Sahara [43]. It is used by people who have previously practiced this mode of treatment in their environment of origin, in this case their village. It includes a set of plants which, according to their users, have anti-typhoid properties. Very diverse, they come in the form of leaves, roots, bark, and tangy fruit. In this study, it was the leaves of Eucalyptus, globulus Labill, Musa paradisaca L, Acanthospermum hispidium, Phyllantus amarus, and Carica papaya L. which have antibacterial properties against Salmonella spp. These properties have been demonstrated by several researchers. Oluwafemi and Debiri [44] have shown that Salmonella Typhi is sensitive in vitro to aqueous and ethanolic extracts of the leaves of Phyllanthus amarus. At a minimum inhibitory concentration of 12.5 mg / ml, the methanolic extract of the leaves of Carica papaya L inhibits the growth of Salmonella Typhi [45]. Better results have been obtained by Agbankpé et al. [46], who showed that at a minimum inhibitory concentration of 5 mg / ml, the hydro-ethanolic extract of the leaves of Musa paradisaca and Crateva adansonii inhibited the growth of Salmonella Typhi. With regard to the leaves of Psidium guajava and Citrus aurantiifolia, the aqueous and ethanolic extracts have an action inhibiting the growth of Salmonella typhi and paratyphi [47, 48]. The hydro-ethanolic extract and the various fractions of the leaves of Acanthospermum hispidium have an antibacterial activity on Salmonella Typhi with minimum inhibitory concentrations varying from 0.625 to 5 mg / ml [49]. The mode of administration of these decoctions has been almost exclusively oral.
Conclusion
Typhoid fever is a common condition, but evolves in an endemo-epidemic fashion in developing countries. Transmission is oro-fecal, occurs through dirty hands and the ingestion of water and contaminated food. This study made it possible to establish the frequency of typhoid fever in the city of Dschang, and to emphasize its uneven spatial distribution. This is a major public health problem in Dschang, the resolution of which requires multi-sectoral collaboration for water management, the establishment of adequate sanitation systems, and public awareness campaigns on the subject. Personal hygiene (hand washing after using the toilet and before preparing food) are initiated to control fecal peril. This study also showedthat sub-Saharan Africa presents a wide range of therapeutic initiatives, ranging from modern medicine to traditional medicines. In addition, there are popular practices, the main actors of which are drug sellers (itinerant or fixed) who distribute drugs across African cities and villages. The use of these routes to cure typhoid and paratyphoid fevers in Dschang illustrates the existence of the therapeutic pluralism of the rest practiced in many African countries [50-52] and whose success is commensurate with the crisis of the systems of health and, more generally, the crisis in African states. The practices and representations that underlie this recourse to traditional medicine refer to a pragmatic and effective logic. This logic is in some cases more significant than the financial or ideological determinants. She explains that a person uses traditional or other medicines, not because of financial problems, but because they believe in their effectiveness. This is why it is desirable to improve the organization of traditional African medicines, in particular because of their real effectiveness and their complementarity with modern medicine. Another lesson to be learned is that self-medication is a cultural and social reality in our cities [51]. To want to ban it, if that were even possible, would be a mistake. Its spontaneous use by any individual and under its own responsibility is not necessarily open to criticism even if this practice appears to be in contradiction with modern rules of the proper use of the drug, of its traceability, of certain compulsory declarations. This responsible self-medication that we advocate (which consists of treating people with their illnesses using authorized drugs, accessible without a prescription, safe and effective under the conditions of use indicated [44], should be used to treat common symptoms. and mild, or for certain chronic pathologies for which an initial diagnosis has been made by the doctor and the risk of seriousness has been eliminated.
References
- Buther T (1997) Fièvre typhoïde. In : Bennet C, Plum F, eds. Cécil Traité de médecine interne. Paris: Médecine-Sciences Flammarion 1642-1648.
- Gake B, Ngaraoua C, Ebole NM, Gake B, Keugoung DE, et al. (2015) Épidémie de fièvre typhoïde à Gassa extrême-nord Cameroun en 2011. Médecine d’Afrique Noire 62 : 257-264.
- Hassani Y, Subiros M, Ruello M, Leguen A et al. (2017) Situation épidémiologique de la fièvre typhoïde à Mayotte en 2017. Bull Epidémiol Hebd. (24-25): 536-539.
- Colin L (1870) Treatise on intermittent fevers. Paris, École Imperiale d’application de médecine militaire, 236 p
- Crump JA, Luby SP, Mintz ED (2004) The gobal burden of typhoid fever. Bulletin of the WHO 82: 346-353.
- Berche P (2007) Une histoire des microbes, John Libbey Eurotext, 300 p.
- Ndako JA, Olisa J, Ilochi C, et al. (2020) Hematological profile in patients with Enteric Fever : 2 Studies on diagnostic evaluation. Int. J. Environ. Res. Public Health, 17,
- Anderson ES, Smith HR (1972) Chloramphenicol resistance in the typhoid bacillus. Br Med J3: 329-31.
- Gröschel DH, Hornick RB (1981) Who Introduced Typhoid Vaccination: Almroth Wright or Richard Pfeiffer?, Reviews of Infectious Diseases3: 1251-1254.
- Toon P (2015) What is healthcare for?, London J Prim Care 7: 115-117.
- Breuil J, Berger N, Dublanche A (1996) Sensibilité aux antibiotiques de 2800 souches de salmonelles et de shigelles en France en 1994. Méd Mal Inf 26 : 420-425.
- Capoor MR, Rawat D, Nair D, Hasan AS, Deb M, et al. (2007) In vitro activity of azithromycin, newer quinolones and cephalosporins in ciprofloxacin-resistant Salmonella causing enteric fever. J Med Microbiol 56 : 1490-1494.
- Reveyrand O (1983), « Étiologie et perception de la maladie dans les sociétés modernes et traditionnelles », Premier colloque national d’anthropologie médicale (Paris, 28- 30 novembre 1983).
- Guillaume A, Kassi N, Koffi N (1997) Morbidité, comportements thérapeutiques et mortalité à Sassandra. In : Croissance démographique, développement agricole et environnement à Sassandra, ORSTOM, GIMIS-CI, Abidjan 1997: 287-310.
- Raobijaona H, Ranaivo-Harisoa HA (2000) Fièvre typhoïde chez l’enfant à Antananarivo Médecine d’Afrique Noire 47: 245-247.
- Jaffre Y, De Sardan O (2003) Une médecine inhospitalière. Les difficiles relations entre soignants et soignés dans cinq capitales d’Afrique de l’Ouest. Khartala, Paris 462 p.
- Oluwafemi F, Debiri F (2008) Antimicrobial Effect of Phyllanthus amarus and Parquetina nigrescens on Salmonella Typhi, African Journal of Biomedical Research 11: 215-219.
- GBD Typhoid and Paratyphoid Collaborators (2019) The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect Dis 19: 369-381.
- Wain J, Kidgell C (2004) The emergence of multidrug resistance to antimicrobial agents for the treatment of typhoid fever. Trans R Soc Trop Med Hyg 98: 423-430.
- Benbekhti S, Allal I (2016) La situation épidémiologique de la fièvre typhoïde dans la Wilaya de Tlemcen, Algérie, 2002–2014. Revue d’Épidémiologie et de Santé Publique 64: 232-243.
- Kirk MD, Pires SM, Black RE, Caipo M, Crump JA, Devleesschauwer B, et al. (2015) World Health Organization estimates of the global and regional disease burden of 22 foodborne bacterial, protozoal and viral diseases, 2010: a data synthesis. PLoS Med 12: e1001921.
- Oboh PA, Abulu EO (1997) The antimicrobial activities of extracts of Psidium guajava and Citrus aurantiifolia, Nigerian Journal of Biotechnology 8: 25-29.
- Commeyras C, Ndo JR, Merabet O, Kone H, Rakotondrabe FP (2006) Comportement de recours aux soins et aux médicaments au Cameroun, Cahiers Santé 1: 5-12.
- Ayalew MB (2017) Self-medication practice in Ethiopia: a systematic review. Patient preference and adherence, 11: 401-413.
- Bolduc D, Lacroix G, Muller C (1996) The choice of medical providers in rural Benin: A comparison of discrete choice models. Journal of Health Economics 15: 477-498.
- Monteillet N (1999) Aperçu sur un système de soins : Le cas de Mbandjock », Anthropologie de la Santé 17 : 648‑651.
- Kalunda EP, Eloko Eya M, Ngongo O, Bulaïmu AM (2010) Comparaison de l’efficacité de l’Ofloxacine et de l’Amoxycilline dans le traitement de la fièvre typhoïde en RDC. Cas de la ville de Kinshasa. Journal d’Epidémiologie et de Santé Publique 1 : 11-27.
- Benoist J (1996) Soigner au pluriel. Essais sur le pluralisme médical. Paris, Khartala, 520 p.
- Cantrelle P, Locoh T (1990) Facteurs culturels et sociaux de la santé en Afrique de l’Ouest. Paris, CEPED, 36 p.
- Augé M (1986) L’anthropologie de la maladie. L’Homme 26: 81-90.
- Clements FE (1932) Primitive Concepts of Disease. American Archeology and Ethnology 2: 185-252.
- Dozon JP, Sindzingre AN (1986) Pluralisme thérapeutique et médecine traditionnelle, Prévenir 12: 43-52.
- Svalastog, AL, Donev D, Jahren KN, Gajovic S (2017). Concepts and definitions of health and health-related values in the knowledge landscapes of the digital society. Croatian medical journal 58: 431-435.
- Diouf P (2000) Problématique des itinéraires thérapeutiques: approche anthropologique des comportements de recours aux soins en milieu rural sénégalais. DEA de Sociologie, UCAD, 135 p.
- Augé M (1984) Ordre biologique, ordre social. La maladie, forme élémentaire de l’événement ». IN: Le sens du mal, Anthropologie, histoire, sociologie de la maladie, Augé M.(ed.) et Herzlich C. (ed.). Paris, Editions des archives contemporaines p.35-91.
- Nguendo Yongsi HB (2016) Santé urbaine: Géo-épidémiologie des diarrhées infectieuses à Yaoundé. Paris, Connaissances & Savoirs 276 p.
- Forget CP (1841) Traité de l’entérite folliculeuse (Fièvre typhoïde). Paris, Ed J.C. Baillière, 218 p
- Adam P, Herzlich C (1994) Sociologie de la maladie et de la médecine, Paris Nathan, 128p.
- Albrecht J, Asif A (1995) Father’s perception of child health in a squatter settlement, Karachi. Health Transition Review 5: 110-121.
- Booker BM, Smith PF, Forrest A, Bullock J, Kelchlin P, et al. (2005) Application of an in vitro infection model and simulation for reevaluation of fluoroquinolone breakpoints for Salmonella enterica serotype typhi. AntimicrobAgents Chemother 49 : 1775-1781.
- Kone G (2012) L’équité de l’accès aux soins dans un contexte de subvention des médicaments : Une analyse économétrique des déterminants du recours aux soins à Dakar. Thèse d’économie, Université Cheikh A. DIOP, Dakar 269p.
- Roumagnac P, Weill FX, Dolecek C, Baker S, Brisse S, et al (2006) Evolutionary history of SalmonellaScience 314 : 1301-1314.
- Dougnon V, Legba B, Yadouléton A, Agbankpe J, Koudokpon H, et al (2018) Utilisation des plantes du Sud-Bénin dans le traitement de la fièvre typhoïde : rôle des herboristes. Ethnopharmacologia 60 : 19-29.
- OMS (2004) Pharmacovigilance : assurer la sécurité d’emploi des médicaments. Genève, Perspectives Politiques de l’OMS sur les médicaments, numéro 9, 6 pages.
- Ayodeji AA, Anthony AA, Mumuni MA (2011) Evaluation of the antimicrobial activities of crude extract of Cryptolepis sanguinolenta and Crateva adansonii leaves and their interactions, Journal of AppliedPharmaceutical Science 1: 85-89.
- Agbankpé AJ, Dougnon TV, Bankolé HS, Houngbegnon O, Dahnouvlessounon D, et al. (2016) In vitro Antibacterial Effects of Crateva adansonii, Vernonia amygdalina and Sesamum radiatum Used for the Treatment of Infectious Diarrhoeas in Benin, Journal of InfectiousDiseases & Therapy 4: 281.
- Onyeagba RA, Ugbogu OC, Okeke CU, Iroakasi O (2004) Studies on the antimicrobial effects of garlic (Allium sativum Linn), ginger (Zingiber officinale Roscoe) and lime (Citrus aurantiifolia Linn), African Journal of Biotechnology 3: 552-554.
- OMS (2020) Les maladies liées à l’eau. Fièvres typhoïdes et paratyphoïdes. Genève, WHO.
- Kahemulwa LK (2008) Étude épidémiologique sur la fièvre typhoïde: à propos de 57 cas observés à l’Hôpital général de Virunga à Goma en RDC, Université de Goma, 101 p
- Dossou-Yovo, Amalaman k, Carnevale P (2001) Itinéraires et pratiques thérapeutiques antipaludiques chez les citadins de Bouake, Med. Trop 61: 495-499.
- Geissler PW, Nokes K, Prince RJ, Odhiambo RO, Aagaard-Hansen J, et al. (2000) Children and medicines : self-treatment of common illnesses among Luo schoolchildren in western Kenya, Social science & medicine, 50:1771-1783.
- Gbaguidi FA, Houngbèmè AG, Ganfon MY, Medegan S, Yèhouénou B, et al. (2015) Antimicrobial activity of compounds from Acanthospermum hispidum DC and Caesalpinia bonduc (L.) ROXB: Beninese plants used by healers against HIV-associated microbial infections, Journal of Applied Pharmaceutical Science 5: 073-081.
- Drame AM (2010) La prévalence de la fièvre typhoïde à Bamako en 2007. Thèse de Doctorat en Médecine, Faculté de médecine, de Pharmacie et d’Odonto Stomatologie, Université de Bamako, 81 p.
- Faye SL, Lalou R, Adjamagbo A (2004) Soigner les enfants exclusivement à domicile en cas de paludisme en milieu rural sénégalais : un effet de la pauvreté ?, African Population Studies/Étude de la Population Africaine, 2 :221-240.
- Frankel A (2004) Les comportements de recours aux soins en milieu rural au Sénégal :le cas des enfants fébriles à Niakhar. Université paris X, thèse de Doctorat en démographie, 465 p.
- Ghysels G (1964) Les Salmonelloses: 80 ans d’Histoire. In: van Oye E. (eds) The World Problem of Salmonellosis. Monographiae Biologicae, vol 13. Springer, Dordrecht.
- Mogasale V, Maskery B, Ochiai RL, Lee JS, Mogasale VV, et al. (2014) Burden of typhoid fever in low income and middle-income countries: A systematic, literature-based update with risk-factor adjustment. Lancet Glob Health 22: 570-580.
- Parry CM, Ho VA, Phuong le T, Bay PV, Lanh MN, et al. (2007) Randomized controlled comparison of ofloxacin, azithromycin, and an ofloxacin-azithromycin combination for treatment of multidrug-resistant and nalidixic acid-resistant typhoid fever. Antimicrob Agents Chemother 51 : 819-825.