Publication Information
ISSN: 2688-0873
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Archives |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Tibiofibular Fusion by Posterolateral Approach to Treat Tibial Nonunions: A Series Cases
Le Phuc*
Saigon ITO Hospital, add 140C Nguyen Trong Tuyen, Ward 8, District Phu Nhuan, HoChiMinh City, Vietnam
Received Date: April 28, 2020; Accepted Date: May 04, 2020; Published Date: May 13, 2020
*Corresponding author: Le Phuc, Saigon ITO Hospital, add 140C Nguyen Trong Tuyen, Ward 8, District Phu Nhuan, HoChiMinh City, Vietnam. Email: leanhuyen108@gmail.com
Citation: Phuc L (2020) Tibiofibular Fusion by Posterolateral Approach to Treat Tibial Nonunions: A Series Cases. Jr Surg Opetech Anesthesia: JSOPA-110.
Abstract
Nonunion of the tibia is always a challenge in orthopaedic surgery, especially when soft tissue of anterior leg is seriously damaged but the axis of the leg is in the range of acceptability. In these cases, Tibiofibular Fusion by Posterolateral Approach is a presumable treatment of choice.
This surgical technique is proven feasible, not further destructive to the soft tissue envelope of the leg, bone healing achieved and satisfactory recovery of function of the limb. This paper, presents 34 surgeries / 32 patients in which the ancientness of nonunion was 14, 5 months (range 4, 5-35 months) and followed-up average 2, 5 years (range 1, 2-6 years). After the functional scores of Hanson: 20 cases are good, 12 cases are fair, no case is poor, having an encouraging outcome in Lower Limb Reconstructive Surgery.
Keywords: Nonunion of Tibia; Tibiofibular Fusion; Posterolateral Approach; Autograft; Ancientness of Nonunion
Introduction
Nonunion of the tibia is a common complication of complex fracture of the leg. In general, it accounts for 5-20% of tibial fractures depend on severity extent of soft tissue and/or bone injuries caused by initial lesions and / or subsequent surgeries.
Classification of tibial nonunion recognized widely in orthopaedic community is Weber & Cech’s. There are 7: C1: elephant’s foot; C2: horse’s foot; C3: oligotrophic; C4: dystrophic (torsional wedge with butterfly); C5: necrotic (comminuted or avascular fragment) and C6: bone loss. C7: atrophic (end- stage of C6). Congenital pseudarthrosis is excluded in this study. Conventional treatments are nonoperative and operative procedures. No operative treatments are included biomechanical or bioelectrical stimulation or weightbearing methods which obtain bone healing in some selective cases. Operative treatments by several techniques have proven effective for majority of cases. The main steps in surgery include debridement and freshening the fractures; stripping the periosteum from the bone and bone grafting.
In the case of anterior soft tissue of leg is so bad, Tibiofibular Fusion by Posterolateral Approach should be considered the treatment of choice. This surgical technique was applied with success in USA by study of Freeland [1], Hanson [2], Jones [3], and in France and francophone countries, by Evrard [4], Vidal [5], and Moyikoua [6]. Tibial nonunion are exposed as large as posible; debridement is meticulously performed, fractures are well freshened. Cancellous bone harvested from posterior iliac wing are placed and filled in the proximal & distal tibiofibular spaces and the gap between tibial fragments. Postoperative immobilisations (by cast or External Fixation) are maintained for a length of appropriate duration of time.
Tibiofibular fusion by Posterolateral Approach secures to recover good function outcome of tibial nonunions in which anterior soft tissue were so damaged, but tibial and fibular alignment were in the range of acceptability. This paper, 34 surgeries on 32 patients were treated with Tibiofibular Fusion by Posterolateral Approach achieved encouraging final outcome was reported.
Patient and Method
Method: Series cases. Clinical trial, self-control: before and after surgery.
Patient: From 2005 to 2016, 34 surgeries on 32 tibial nonunions of 25 males, 7 females were enrolled in study (Table I).
| Patient No. | Age | Cause of Facture | Classification | Leg Shortening | Second Bone Graft | Postop Immobilisation | Results | |
| Male | Female | |||||||
| 1 | 35 | TA | C5 | C | G | |||
| 2 | 31 | TA | C7 | EF | G | |||
| 3 | 33 | TA | C6 | + | C | G | ||
| 4 | 27 | TA | C4 | EF | F | |||
| 5 | 29 | TA | C6 | C | G | |||
| 6 | 28 | TA | C6 | + | C | F | ||
| 7 | 33 | TA | *C6 | C | G | |||
| 8 | 49 | TA | C6 | C | G | |||
| 9 | 25 | TA | C5 | C | G | |||
| 10 | 50 | TA | C7 | EF | F | |||
| 11 | 27 | TA | C3 | C | G | |||
| 12 | 28 | TA | C6 | C | G | |||
| 13 | 16 | TA | C6 | EF | F | |||
| 14 | 40 | TA | C3 | + | C | F | ||
| 15 | 32 | TA | C6 | EF | G | |||
| 16 | 33 | TA | C1 | C | F | |||
| 17 | 55 | TA | C2 | + | EF | F | ||
| 18 | 18 | TA | C1 | C | F | |||
| 19 | 19 | TA | C5 | EF | G | |||
| 20 | 36 | TA | C4 | + | C | F | ||
| 21 | 43 | TA | C1 | C | G | |||
| 22 | 27 | TA | C4 | EF | F | |||
| 23 | 32 | TA | C4 | C | G | |||
| 24 | 30 | TA | C5 | C | G | |||
| 25 | 35 | TA | C3 | C | G | |||
| 26 | 32 | TA | C4 | C | G | |||
| 27 | 19 | FfH | C5 | C | G | |||
| 28 | 18 | TA | C1 | EF | G | |||
| 29 | 24 | TA | C3 | + | C | G | ||
| 30 | 49 | FfH | C3 | + | C | F | ||
| 31 | 36 | FfH | C4 | C | G | |||
| 32 | 24 | TA | C5 | C | F | |||
| Note: Abbreviation: TA: Traffic Accident; FfH: Fall from Height; EF: External Fixation; C: Casting; G: Good; F: Fair.
*= bone less 10cm. |
||||||||
Operative technique: Tibiofibular Fusion by Posterolateral Approach (Figure 1).
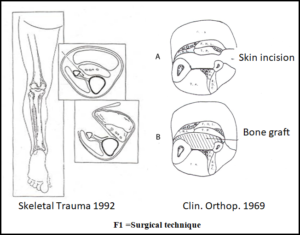
Patient’s position is prone with tourniquet at groin. Skin incision is made longitudinally on the posterolateral aspect of the leg approximately 1-2 cm posterior to the fibula and parallel to it. The length of the incision is determined by the need to expose 4-5 cm of bone above and below the fracture site. After the subcutaneous tissue is divided, the tibia is then exposed for the desired length. The posterior tibial artery and veins are not exposed but rather retracted medially in the muscle mass to expose nonunion and tibiofibular proximal and distal spaces. Small strip of autologous cortical cancellous bone grafts harvested from posterior iliac wing were placed over tibiofibular spaces and between two tibial fragments as well. Postoperative immobilisations were External Fixation or Casting.
Results
Pre-Operation
Twenty-five males, 7 females whose mean age: 31years old (range 16-55 years). Average oldness of tibial nonunion were 14, 5 months (range 4, 5-35 months). Fractures by traffic accident: 29 cases (90%). Nonunion involved middle third of tibia : 12 cases (37%).Tibial angulation ≤150– ≥50: 7 cases ; ≤ 50: 15 cases ; no angulation: 10 cases. 32/32 patients whose tibial anterior soft tissue were so bad due to initial injuries and/or the subsequent surgeries. 8 patients sustained tibial bone loss average 2,8cm (range 1,2-10cm). Average number of past surgeries was 3, 8 times (range 2-11 times). At the time of surgery no infection (at the nonunion) detected. ESR=26 mm (range 12-37mm), CRP=11% (range 8-22%). Postoperative immobilization: 23 casting, 9 external fixations. 34 surgeries / 32 patients were documented with pre op and postop and last clinical / radiographic findings for evaluations.
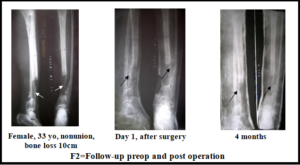

Post-Operation
Thirty patients of 32 patients achieved bone healing after 1 surgery; two patients needed second bone grafting. Knee flexion ≥90o – ≤120o: 6 patients; whose flexion loss 160 (range 5-25o). 26 patients achieved normal knee flexion. Knee extension loss ≤5o: 13 patients. 19 patients got full extension. Ankle ROM ≥40o – ≤60o: 7 patients, whose ROM loss 70 (range 3-20o). Normal ankle ROM is 25 patients.
- Leg shortening 1,8cm (range 0, 5-3 cm): 5 patients. No change in comparison with preoperative.
- Muscular dystrophy 3,2cm (range 1-5cm): 12 patients.
- Peroperative venous lesion: 3 cases were successfully managed.
- Algodystrophia registered in 5 patients and paresthesia in 6 patients which didn’t affect limb function.
- Infection: 2 superficial needed longer hospital stay and then healed.
- After Hanson function scores, there were 20 Good (60%), 12 Fair (40%).
- Average follow-up time: 2, 5 years (range 1, 2 – 6 years.
Discussion
- The orthopaedic surgeon must be able to judge whether a slowly healing tibial fracture will heal eventually (delayed union) or unlikely to heal even with time (nonunion). In 1986, an FDA panel defined nonunion as “established when a minimum of nine months has elapsed since injury and the fracture shows no visible progressive signs of healing for a minimum of three months. Realistically, in most clinical situations a tibial fracture is considered to be ununited if, after six months or more, physical testing shows no progress toward union and there is no radiographic evidence of callus bridging. Indeed, many believe six months is too long to wait. Charnley stated that “the decision to graft can be made three months after tibial fracture, purely on the amount of movement which can be detected clinically”.
- Nonunion of the tibia, if soft tissue of anterior leg is in good status, the treatment is standardized: debridement of fracture; removal of strange materials, dead bone; freshening the bone until bloody; stripping the periosteum from bone to stimulate bone healing, then immobilization (by cast or osteosynthesis) and cancellous bone graft. In case of soft tissue of anterior leg is seriously destructive. It is a special lesion which needs a different management: not routine anterior approaches, not routine site to harvest the bone for grafting.
- For this special situation, the approach accepted by majority of surgeons is posterolateral which avoid the scar, access not so difficultly to the nonunion, expose the tibial fragments, and place the bone grafts. This approach for tibiofibular fusion first time described by Harmon [7] in 1945, since then it’s proven more useful. Tibiofibular fusion is one way to achieve bone healing of the leg in which the fibula healed well or not fractured, rigid enough for the weight bearing. There are some techniques to fuse tibiofibular as Merle D’ Aubigne, or Campanacci or Duparc [8]. In this study, chipbones are used; fill in the gap between two tibial fragments and tibiofibular spaces. No hardware or a big piece of bone graft was utilized to stabilize the fractures.
- In this study, 32 patients whose tibial axis were in the range of acceptability (<150 in sagittal plane, < 50 in frontal plane). 22 fibulae healed in good alignment, 10 fibulae intact. No correction osteotomy surgeries
Conclusion
Tibiofibular fusion by Posterolateral Approach secures to recover good function outcome of tibial nonunions in which anterior soft tissue were so damaged, but tibial and fibular alignment were in the range of acceptability.
Funding: No funding or grant support was received for this work.
Conflict of Interest: No financial disclosures
References
- Freeland AE, Mutz SB (1976) Posterior bone grafting for infected ununited fractures of the tibia. JBJS 58: 653-657.
- Hanson LW, Eppright RH (1966) Posterior bone grafting of the tibia for nonunion: A review of twenty four cases. JBJS 48: 27-43.
- Harmon PH (1945) The simplified surgical approach to the posterior tibia for bone grafting and fibular transference. JBJS 27: 496.
- Evrard J (1992) Place de la greffe inter-tibio-péronière dans le traitement des fractures et pseudarthroses infectées de jambe. Revue de Chirurgie Orthopédique et reparatrice de l’appareil locomoteur, 78: 389-398.
- Vidal J, Buscayret CH, Finzi M, Melka J (1982) Les greffes inter-tibio-peroniere dans le traitement des retards de consolidation jambiers. A propos de 47 cas. Revue de chirurgie orthopedique et reparatrice de l’appareil locomoteur. 68: 12:132.
- Moyikoua A, Pena-Pitra B (1998) Interet de la greffe inter-tibio-peroniere dans les pseudarthroses de jambe a risque septique. A propos de 21 cas. Revue de chirurgie orthopedique et reparatrice de l’appareil locomoteur 84: 358-362.
- Jones KG, Barnett HC (1955) Cancellous bone grafting for nonunion of the tibia through the posterolateral approach. JBJS 37: 1250-1260.
- Rienau G (1983) Manuel de Traumatologie. Masson 245-251.