Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
The Kerlan-Jobe Functional Shoulder Test: Reliability of an upper extremity isometric strength test
Zach McVicker1*, Adam Cady1, Brian Serrano1, Michael Banffy1
1Cedars-Sinai Kerlan-Jobe Institute
Received Date: November 18, 2022; Accepted Date: November 24, 2022; Published Date: November 30, 2022;
*Corresponding author: Zach McVickers. Cedars-Sinai Kerlan-Jobe Institute. Email: zmcvicker@paleyinstitute.org
Citation: McVicker Z, Adam Cady A, Serrano B, Banffy M (2022) The Kerlan-Jobe Functional Shoulder Test: Reliability of an upper extremity isometric strength test. Adv Ortho and Sports Med: AOASM-172.
DOI: 10.37722/AOASM.2022402
Abstract
Background
Upper extremity injuries are common in overhead sports, however objective criteria to support return to sport decisions remains limited. This study seeks to create preliminary data on a novel shoulder test for functional strength, prior to return to play after a shoulder injury.
Purpose
The purpose of this study is to establish reliability and feasibility of a novel functional shoulder strength test.
Study Design
Test-Retest Reliability Study
Methods
22 healthy subjects were recruited for this study. The study was conducted over two non-consecutive days. Each testing session consisted of 4 testing positions which included I, Y, internal rotation (IR), and external rotation (ER). Both upper extremities were tested to ensure accurate data between dominant and non-dominant limbs. Intra-class correlation coefficient (ICC) was performed to establish the reliability of this functional test.
Results
Of each testing position, all were found to have very good reliability (>0.85 ICC) while I, Y and ER for both limbs were found to have excellent reliability (>0.90 ICC).
Conclusion
The Kerlan-Jobe Functional Shoulder Test has data supporting its reliability. This study should be followed by larger scale studies, to further investigate its reliability across diverse populations.
Clinical Relevance
Return to sport criteria after upper extremity injury is limited. This study designed a novel test, providing objective data, to aid in clearance of an athlete for return to overhead sports.
Keywords: Overhead Athlete; Return to Sport; Shoulder; Shoulder Injury
Introduction
Shoulder and elbow injuries are common in overhead sports (Laudner & Sipes, 2009; Wong et al., 2017). Overhead sports are classified as any sport in which athletes must throw an object or perform a hitting motion using the upper extremity (Asker et al., 2018). Overhead sports include but are not limited to baseball, water polo, javelin, and volleyball. In overhead, the shoulder and elbow are at increased risk of injury due to the high forces required to perform sport specific tasks (Cain et al., 2003; Wright et al., 2018).
In the shoulder, the repetitive overhead motion can lead to injuries to the labrum, rotator cuff, and proximal biceps tendon (Abrams & Safran, 2010; Chalmers & Verma, 2016; Economopoulos & Brockmeier, 2012). Post injury, conservative management is typically utilized as first line treatment, which includes manual therapy, addressing mobility deficits, and strengthening peri-scapular musculature (de Mey et al., 2012; Wilk et al., 2002). If conservative management fails, a surgical decision is usually indicated and performed enable the athlete to return to play.
Following conservative or surgical management of the injury, the rehabilitation goal is to restore motion, strength, and function of the upper extremity, which is crucial for overhead performance (Wilk et al., 2015, 2016). While there is a plethora of rehabilitation protocols made for these injuries, they do not provide objective measures strength to aid in decision making for returnto sport.
In contrast to upper extremity injuries, lower extremity injuries have many objective measurements for return to sport criteria (Domb et al., 2014; Harris et al., 2014). For example, after ACL injury it is common for patients to undergo a battery of tests utilized to assess the function of the knee and lower extremity, such as hop and jump tests (W. T. Davies et al., 2020; Gustavsson et al., 2006; Logerstedt et al., 2012). I for athletes suffering from ACL injuries, the best evidence states that they should reach a limb-symmetry index (LSI) of at least 90% for return to sport (Büchler et al., 2016; Nagai et al., 2020; Rohman et al., 2015). The upper extremity should have similar evidence based standards for return to play.
Recently, Ashworth et al. (2018) created a series of functional tests to assess return to tackling in rugby athletes, which consists of three testing positions (Ashworth et al., 2018). Due to the lack of objective data in returning to overhead sports, the authors of the current study decided to perform a study to investigate this novel functional shoulder test. The purpose of this study is to investigate the reliability of a functional shoulder test in assessing return to sport in overhead athletes.
Methods
This is a test-retest study of healthy subjects to assess measures of upper extremity strength on portable force decks (VALD performance, Queensland, AU). Based on a similar study by Ashworth et al. (2018) which used 18 healthy subjects, the authors planned for enrollment of 18 subjects. A total of 22 healthy subjects were enrolled and subsequently tested. (Ashworth et al., 2018). All subjects were employees of the testing institution, recruited with flyers, email, and by word of mouth. All subjects were provided with a written and verbal explanation of the testing procedures, before enrollment, which was approved by the Institutional Review Board. Subjects were excluded if they had sustained an acute injury to the neck or shoulder girdle (<72 hours prior to testing), experienced pain post testing that lasted longer than 20 minutes, or if they were unable to get into any one of the standardized testing positions secondary to inadequate range of motion.
Functional Shoulder Test
The functional shoulder tests consisted of 4 testing positions; 3 in the prone position and 1 in supine. The hand of the corresponding upper extremity performing the test was placed on a portable force plate connected to data analysis software (VALD Performance, Queensland, AU). For the I-test, the shoulder was in full forward flexion, the forearm in pronation, and the palm as the point of contact with the force plate. For the Y-test, the shoulder was placed in 135 degrees of shoulder abduction, forearm in pronation, and the palm as the point of contact with the force plate. For the internal rotation (IR) test, the shoulder was in the 90/90 position (90 degrees of shoulder abduction, 90 degrees of elbow flexion). In the external rotation (ER) test, the subject was supine, and shoulder was in the 90/90 position (90 degrees of shoulder abduction, 90 degrees of elbow flexion). For the I and Y tests, the elbow was fully extended. For the IR and ER tests, the elbow was flexed to 90 degrees. The hand was the only point of contact and the remaining upper extremity was parallel to the force plate and hovering above the floor for all testing positions.
Figure 1 demonstrates the positions of the 4 tests.
I Test

Y-Test

IR Test

ER Test
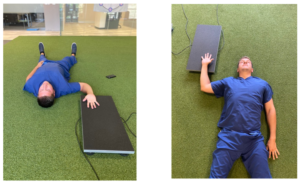
Each subject performed a self-paced warm-up consisting of active shoulder range of motion, to increase blow flow to extremity in preparation for testing. Subjects were provided instructions for each test, verbalized understanding, and allowed to perform two trials of each testing session before data collection.
In the prone testing positions (I, Y, IR), subjects were directed to maintain their scapula in a neutral position relative to the upper extremity being tested (no winging, anterior tilt, or excessive upward rotation). Before data collection in each test position, standardized positioning was visually confirmed. The contralateral arm was placed behind the back to avoid compensatory force production. During each test, the subject was directed to stabilize their core, to limit trunk rotation without using the contralateral arm. If the subject failed to maintain the standardized position at any time point during the testing, the data was discarded, and another trial was performed. The supine test (ER) was performed by having the subject lie flat with the uninvolved arm resting on the ground next to the participant. Tests were consistently performed in the following order: I, Y, IR, ER and conducted on two non-consecutive days with a day of rest (Monday and Wednesday or Tuesday and Thursday). Each testing position was performed three times with the average being used for data analysis. The entire testing protocol took less than 10 minutes per subject, including warm-up and recovery periods. Upon arrival for their second testing session, subjects were asked if they had any questions or concerns, then were reminded of the testing protocol.
The testing protocol consisted of performing all 4 positions, with 3 trials in each position. Each subject was instructed to “press down with maximal effort”, and verbal encouragement was provided at the start of each test. Each attempt consisted of 3 seconds of exertion, alternating with 5 seconds of rest. During the rest period the extremity was removed from the force plate. A 20 second recovery was used between test positions. Testing, supervision, instruction and data collection was performed by the same author for consistency.
Statistical Analysis A power analysis was performed using Interclass Correlation Coefficient (ICC) values proposed by Fleiss using a minimum ICC value of 0.70 (moderate) and Expected ICC value of 0.90 (excellent) with significance level of 0.05 and power of 80% (Kottner et al., 2011). The average of the three tests was used for data analysis and we expected a 10% dropout rate which yielded a 19 subject sample size to achieve statistical significance.
The average Peak Vertical Force (PVF) was collected for each upper extremity test, and used in the analysis. The PVF is defined as the maximum force exerted perpendicular to the surface by the hand on the force plate (Kirby et al., 2011; Ortega et al., 2010). Mean and Standard Deviation (SD) were calculated for maximum and mean PVF in newtons. Parametric tests were used to analyze the data due to its normal distribution determined by the Kruskal-Willis Test. To assess the reliability of each test position over the testing sessions, the authors calculated the intraclass correlation coefficient (ICC). The results were interpreted based on work by Fleiss et al. (2011). Fleiss found that higher values indicate higher reliability (>0.90=excellent; 0.80-0.89=good; 0.70-0.79 moderate; <0.70 low). The bias, root mean square (RMSE), and coefficient of variation (CV) were also calculated to measure the variability between each position and test session.
Results
22 participants were enrolled in the study. No participants were excluded based on the criteria listed previously. Table 1 list the demographics of the subjects.
Demographics
Average
Range
Age
30.4
22-51 years old
Height
68.8
61-77 inches
Weight
171.0
100-235 Ilbs
Gender
7 females, 15 males
Hand Dominance
2 Left, 20 Right
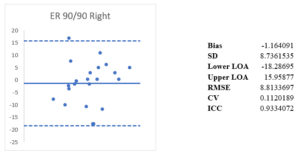
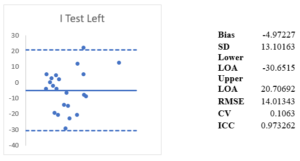
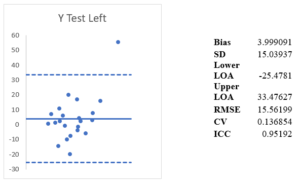
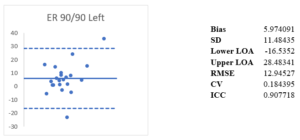
Intraclass correlation coefficient (ICC) was calculated for each testing position and limb. ICC was excellent (>0.90) for all test positions except IR, which was very good at 0.85. ICC for I-right was 0.97, I-left was 0.97, Y-right was 0.95, Y-left was 0.95, IR- right was 0.89, IR- left was 0.86, ER- right was 0.93, and ER-left was 0.91. The coefficient of variation (CV) was found to be in the range of (0.14-0.20) for all tests. The Root Mean Square Error (RMSE) ranges from 8.81-27.04. The Bland-Altman Method is used to quantify agreement between two quantitative measurements by construction limits of agreement. It was used for each of the tests to evaluate for bias between mean differences and to estimate an agreement interval.
Test Position
Day 1
Day 2
ICC
CV (%)
RMSE
Bias
Right Arm
I Test
140.00± 62.23
141.00±62.14
0.96 (0.93 to 0.99)
14.6 (10.03 to 19.1)
15.71 (11.14 to 20.28)
-2.71
Y Test
123.63±52.84
117.89±49.60
0.95 (0.92 to 0.98)
14.0 (9.27 to 18.73)
16.93 (12.2. to 21.66)
5.46
IR Test
132.27 ±52.03
134.55±46.68
0.89 (0.86 to 0.92)
17.6 (10.69 to 24.51)
23.39 (16.48 to 30.3)
-2.28
ER Test
78.09 ± 24.31
79.25±23.16
0.93 (0.90 to 0.96)
11.2 (8.62 to 13.78)
8.81 (6.23 to 11.39)
-1.16
Left Arm
I Test
129.34±56.64
134.31±53.38
0.97 (0.94 to 0.99)
10.6 (6.76 to 14.47)
14.01 (10.14 to 17.88)
-4.97
Y Test
115.71±45.08
111.71±39.96
0.95 (0.92 to 0.98)
13.6 (9.16 to 18.04)
15.56 (11.12 to 20)
3.99
IR Test
130.47±51.92
131.25±48.04
0.85 (0.82 to 0.88)
20.6 (12.62 to 28.58)
27.04 (19.06 to 35.05)
-0.77
ER Test
73.19±26.70
67.21±21.70
0.90 (0.87 to 0.93)
18.4 (13.61 to 23.19)
12.95 (8.16 to 17.91)
5.97



Discussion
In this study, the authors evaluated a series of functional shoulder strength tests, designed to test positional strength that is required of overhead athletes. We used portable force plates to evaluate 4 testing positions (I, Y, IR, ER). The I and Y tests were implemented based on common biomechanics in overhead sports (Weber et al., 2014a, 2014b). Specific to throwing, IR and ER strength is necessary to perform overhead motions, while producing high amounts of force and velocity. (Mascarin et al., 2017; Sirota et al., 1997). Furthermore, lack of strength in the rotator cuff musculature is a risk factor for shoulder injury (van der Hoeven & Kibler, 2006). The ratios of IR/ER have been investigated and found to be a potential risk factor for injury in overhead athletes (Brown et al., 1988; Ellenbecker & Mattalino, 1997).
Although baseball may be the most popular overhead sport, we sought to be more inclusive and give clinicians working with other overhead athletes, an objective measure, to aid in decision making for return to sport. In sports such as volleyball, the ball is hit from varying angles, corresponding primarily to the I and Y positions (Kilic et al., 2017; Stickley et al., 2008). In sports such as football, baseball, and water polo; the I and Y also are a component of each of those sports throwing motion (Escamilla & Andrews, 2009; Hsu et al., 2005). More specifically, the late cocking phase of throwing is when the arm reaches maximal external rotation and abduction followed by an acceleration into internal rotation (Fortenbaugh et al., 2009). Type 2 SLAP tears as classified by Snyder et al. are thought to occur in this late-cocking phase due to forces placed on the superior labrum, secondary to torsion of the long head of the biceps tendon (LHBT) (Knesek et al., 2013; Snyder et al., 1990). Type 3,4 SLAP tears are thought to occur during the traction forces of the LHBT pulling on the labrum (Snyder et al., 1990; Yeh et al., 2005). Injuries to the rotator cuff are also common in throwers secondary to internal impingement or eccentric overload (Heyworth & Williams, 2009; McFarland et al., 1999). For example, with repetitive cocking there is increased contact between the rotator cuff musculature (posterior supraspinatus and anterior infraspinatus) between the posterior humeral head and glenoid rim (Drakos et al., 2009). The large eccentric force placed on the rotator cuff during deceleration phase of throwing has been shown to result in injury as well (Camargo et al., 2014; Niederbracht et al., 2008). By implementing these 4 tests, a clinician will have objective measures of strength that are more specific to demands of overhead athletes, likely leading to more informed decision making regarding return to play.
To our knowledge, this is the first study utilizing a series of functional strength measures, specific to strength necessary for the demands of an overhead athlete. Ashworth et al. (2018) tested the reliability of a series of tests on portable force plates in various positions (I, Y, T) made to mimic motions in rugby and found excellent reliability (ICC 0.94-0.98) (Ashworth et al., 2018). However, these tests were made as a return to tackling test in rugby, which has different demands in comparison to overhead sports.
Holt et al. (2016) investigated inter and intra-reliability of hand-held (HHD) and externally fixed dynamometry for shoulder IR and ER strength and their correlation to isokinetic testing using 20 healthy subjects (Holt et al., 2016a). Subjects were standing and either exerting force onto a clinician holding an HHD or against an isokinetic strength machine. They found that both measures of strength were suitable for clinical practice and research (HD ICC=0.89-0.97; HD EFD ICC=0.88-0.96) (Holt et al., 2016a). Similarly, Cadogan et al. (2010) measured reliability of a new HHD in measuring isometric muscle strength in 40 subjects with unilateral shoulder pain (Cadogan et al., 2011). The authors assessed seated shoulder abduction, seated external rotation in a neutral position and found a high level of reliability (ICC 0.85-0.99; LOA 6-24 degrees and 1.1-7.0 kg) (Cadogan et al., 2011).
Our study follows a similar testing position from Awatani et al. (2016) using an HHD on the ground where subjects were in the prone position (Awatani et al., 2016). Although no picture is present within the manuscript, this seems to follow the I position used by this study and Ashworth et al. (2018). Awatani et al. (2016) test same-session data and between-day data and found moderate to excellent reliability (0.797-0.985) Cools et al. (2014) measured shoulder IR and ER in the supine, sitting, and prone positions with HHD and found good to excellent reliability for each position (Cools et al., 2014b).
Although there is paucity in the literature regarding upper extremity isometric strength on force plates, we were able to compare our methods to those of Ashworth et al. (2018) and McCall et al. (2015). McCall et al. (2015) used portable force plates to examine the reliability and sensitivity of strength tests on posterior limb musculature in soccer players (McCall et al., 2015). They found a high reliability for strength testing of both dominant and non-dominant legs (D: CV=4.3%, ICC=0.95, ES=0.15; ND: CV=5.4%, ICC=0.95, ES=0.14) and concluded that the use isometric strength testing on portable force plates was useful and practical (McCall et al., 2015). Ashworth et al. (2018) similarly found excellent reliability (ICC 0.94-0.98, SEM 4.8-10.18) in their 3 upper extremity testing positions.
In the literature, there is high variability in terms of when to initiate a throwing progression and/or when to clear an athlete to return to sport after upper extremity injuries. In the lower extremity, due to a plethora of literature on knee and hip injuries, more objective criteria to aid in return to sport decision making exists (Casartelli et al., 2015; G. J. Davies et al., 2017; Kaplan & Witvrouw, 2019; Kim et al., 2016). For example, isokinetic testing, force plate testing, and field battery testsusing a Limb-Symmetry Index (LSI) of at least 85-90% is somewhat of a standard used to clear an athlete for return to sport (Ebert et al., 2018; Gaunt & Curd, 2001; Gokeler et al., 2017). These studies provide framework for the utilization of LSI, for clearance of an athlete to an overhead sport, after an upper extremity injury. The Kerlan-Jobe Functional Shoulder test may serve to provide normative values for upper extremity LSI, thus leading to more objective evaluation for return to sport.
Limitations
This study used healthy volunteers to provide preliminary data on a novel functional shoulder strength test, thus it is too early to extrapolate the results to the targeted population of overhead athletes. The testing sessions were spread between days (ex: Monday, Wednesday) which may not have been the ideal setting for testing reliability as other studies have used same day and consecutive day sessions. The prone and supine positions may not be truly functional as the sports we seek to imitate occur while standing and varying positions of the lower extremities, and trunk rotation. However, since shoulder and elbow injuries are common in overhead athletes, the prone and supine positions attempt to isolate the shoulder musculature. We decided to use an exertion: rest ratio of 3 seconds to 5 seconds, and a rest period of 20 seconds between trials which differ from other testing protocols (Cools et al., 2014; Holt et al., 2016). Normative strength data comparing dominant and non-dominant upper extremities, and objective criteria relating to a level of LSI that would be acceptable for clearance to return to sport is lacking in the literature. Thus the Kerlan-Jobe Functional Shoulder test needs to be validated across diverse overhead sport populations, and therefore should not be used as the only criteria for returning an athlete to an overhead sport at this time.
Conclusion
The Kerlan-Jobe Functional Shoulder Test performed with very good to excellent reliability in all positions. Our cohort of 22 subjects consisted of healthy subjects from both genders along with a varied age range (22-51). The high reliability shows a positive trend that the 4 testing positions may have clinical utility when making a return to sport decision with overhead athletes. Larger scale studies should be explored in athletes returning to various overhead sports. As no test should be used alone, the authors suggest using this testing series in conjunction with other strength tests, assessments, and biopsychosocial measures to aid in return to sport decision making.
References
- Abrams, G. D., & Safran, M. R. (2010). Diagnosis and management of superior labrum anterior posterior lesions in overhead athletes. British Journal of Sports Medicine, 44:311-318.
- Ashworth, B., Hogben, P., Singh, N., Tulloch, L., & Cohen, D. D. (2018). The Athletic Shoulder (ASH) test: Reliability of a novel upper body isometric strength test in elite rugby players. BMJ Open Sport and Exercise Medicine, 4(1), 365.
- Asker, M., Brooke, H. L., Waldén, M., Tranaeus, U., Johansson, F., Skillgate, E., & Holm, L. W. (2018). Risk factors for, and prevention of, shoulder injuries in overhead sports: A systematic review with best-evidence synthesis. In British Journal of Sports Medicine (52:1312-1319). BMJ Publishing Group.
- Awatani, T., Mori, S., Shinohara, J., Koshiba, H., Nariai, M., Tatsumi, Y., Nagata, A., & Morikita, I. (2016). Same-session and between-day intra-rater reliability of hand-held dynamometer measurements of isometric shoulder extensor strength. Journal of Physical Therapy Science, 28: 936-939.
- Brown, L. P., Niehues, S. L., Harrah, A., Yavorsky, P., & Hirshman, H. P. (1988). Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. The American Journal of Sports Medicine, 16:577-585.
- Büchler, L., Regli, D., Evangelopoulos, D. S., Bieri, K., Ahmad, S. S., Krismer, A., Muller, T., & Kohl, S. (2016). Functional recovery following primary ACL repair with dynamic intraligamentary stabilization. Knee, 23:549-553.
- Cadogan, A., Laslett, M., Hing, W., McNair, P., & Williams, M. (2011). Reliability of a new hand-held dynamometer in measuring shoulder range of motion and strength. Manual Therapy, 16:97-101.
- Cain, E. L., Dugas, J. R., Wolf, R. S., & Andrews, J. R. (2003). Elbow injuries in throwing athletes: A current concepts review. In American Journal of Sports Medicine (Vol. 31, Issue 4, pp. 621-635). American Orthopaedic Society for Sports Medicine.
- Camargo, P. R., Alburquerque-Sendín, F., & Salvini, T. F. (2014). Eccentric training as a new approach for rotator cufftendinopathy: Review and perspectives. World Journal of Orthopaedics, 5:634-644.
- Casartelli, N. C., Leunig, M., Maffiuletti, N. A., & Bizzini, M. (2015). Return to sport after hip surgery for femoroacetabular impingement: A systematic review. In British Journal of Sports Medicine (Vol. 49:819-824). BMJ Publishing Group.
- Chalmers, P. N., & Verma, N. N. (2016). Proximal Biceps in Overhead Athletes. In Clinics in Sports Medicine (Vol. 35:163-179). W.B. Saunders.
- Cools, A. M., de Wilde, L., van Tongel, A., Ceyssens, C., Ryckewaert, R., & Cambier, D. C. (2014a). Measuring shoulder external and internal rotation strength and range of motion: Comprehensive intra-rater and inter-rater reliability study of several testing protocols. Journal of Shoulder and Elbow Surgery, 23:1454-1461.
- Cools, A. M., de Wilde, L., van Tongel, A., Ceyssens, C., Ryckewaert, R., & Cambier, D. C. (2014b). Measuring shoulder external and internal rotation strength and range of motion: Comprehensive intra-rater and inter-rater reliability study of several testing protocols. Journal of Shoulder and Elbow Surgery, 23:1454-1461.
- Davies, G. J., McCarty, E., Provencher, M., & Manske, R. C. (2017). ACL Return to Sport Guidelines and Criteria. In Current Reviews in Musculoskeletal Medicine (Vol. 10:307-314). Humana Press Inc.
- Davies, W. T., Myer, G. D., & Read, P. J. (2020). Is It Time We Better Understood the Tests We are Using for Return to Sport Decision Making Following ACL Reconstruction? A Critical Review of the Hop Tests. In Sports Medicine (Vol. 50:485-495). Springer.
- de Mey, K., Danneels, L., Cagnie, B., & Cools, A. M. (2012). Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: Effect of a 6-week training program on muscle recruitment and functional outcome. American Journal of Sports Medicine, 40:1906-1915.
- Dodson, C. C., Slenker, N., Cohen, S. B., Ciccotti, M. G., & DeLuca, P. (2010). Ulnar collateral ligament injuries of the elbow in professional football quarterbacks. Journal of Shoulder and Elbow Surgery, 19:1276-1280.
- Domb, B. G., Stake, C. E., Finch, N. A., & Cramer, T. L. (2014). Return to sport after hip arthroscopy: Aggregate recommendations from high-volume hip arthroscopy centers. Orthopedics, 37: e902-e905.
- Drakos, M. C., Rudzki, J. R., Allen, A. A., Potter, H. G., & Altchek, D. W. (2009). Internal Impingement of the Shoulder in the Overhead Athlete. The Journal of Bone & Joint Surgery, 91:2719-2728.
- Ebert, J. R., Edwards, P., Yi, L., Joss, B., Ackland, T., Carey-Smith, R., Buelow, J. U., & Hewitt, B. (2018). Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 26:2353-2361.
- Economopoulos, K. J., & Brockmeier, S. F. (2012). Rotator Cuff Tears in Overhead Athletes. In Clinics in Sports Medicine (Vol. 31:675-692). Elsevier.
- Ellenbecker, T. S., & Mattalino, A. J. (1997). Concentric isokinetic shoulder internal and external rotation strength in professional baseball pitchers. Journal of Orthopaedic and Sports Physical Therapy, 25:323-328.
- Escamilla, R. F., & Andrews, J. R. (2009). Shoulder muscle recruitment patterns and related biomechanics during upper extremity sports. In Sports Medicine (Vol. 39:569-590). Springer.
- Fortenbaugh, D., Fleisig, G. S., & Andrews, J. R. (2009). Baseball pitching biomechanics in relation to injury risk and performance. Sports Health, 1:314-320.
- Gaunt, B. W., & Curd, D. T. (2001). Anthropometric and demographic factors affecting distance hopped and limb symmetry index for the crossover hop-for-distance test in high school athletes. Journal of Orthopaedic and Sports Physical Therapy, 31:145-151.
- Gokeler, A., Welling, W., Benjaminse, A., Lemmink, K., Seil, R., & Zaffagnini, S. (2017). A critical analysis of limb symmetry indices of hop tests in athletes after anterior cruciate ligament reconstruction: A case control study. Orthopaedics and Traumatology: Surgery and Research, 103:947-951.
- Gustavsson, A., Neeter, C., Thomee´karin, P., Gra¨vare, T., Silbernagel, G, et al. (2006). A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction SPORTS MEDICINE. Knee Surg Sports Traumatol Arthrosc, 14:778-788.
- Harris, J. D., Abrams, G. D., Bach, B. R., Williams, D., Heidloff, D., Bush-Joseph, C. A., Verma, N. N., Forsythe, B., & Cole, B. J. (2014). Return to sport after ACL reconstruction. Orthopedics, 37(2), e103-e108.
- Heyworth, B. E., & Williams, R. J. (2009). Internal impingement of the shoulder. American Journal of Sports Medicine, 37(5), 1024-1037.
- Holt, K. L., Raper, D. P., Boettcher, C. E., Waddington, G. S., & Drew, M. K. (2016a). Hand-held dynamometry strength measures for internal and external rotation demonstrate superior reliability, lower minimal detectable change and higher correlation to isokinetic dynamometry than externally-fixed dynamometry of the shoulder. Physical Therapy in Sport, 21, 75-81.
- Holt, K. L., Raper, D. P., Boettcher, C. E., Waddington, G. S., & Drew, M. K. (2016b). Hand-held dynamometry strength measures for internal and external rotation demonstrate superior reliability, lower minimal detectable change and higher correlation to isokinetic dynamometry than externally-fixed dynamometry of the shoulder. Physical Therapy in Sport, 21, 75-81.
- Hsu, C.-Y., Un, P.-C., & Un, H.-M. (2005). BIOMECHANICS ANALYSIS OF WATER POLO THROWING. In ISBS - Conference Proceedings Archive.
- Kaplan, Y., & Witvrouw, E. (2019). When Is It Safe to Return to Sport After ACL Reconstruction? Reviewing the Criteria. In Sports Health (Vol. 11:301-305). SAGE Publications Inc.
- Kilic, O., Maas, M., Verhagen, E., Zwerver, J., & Gouttebarge, V. (2017). Incidence, aetiology and prevention of musculoskeletal injuries in volleyball: A systematic review of the literature. In European Journal of Sport Science (Vol. 17, Issue 6, pp. 765-793). Taylor and Francis Ltd.
- Kim, C., Chasse, P. M., & Taylor, D. C. (2016). Return to Play After Medial Collateral Ligament Injury. In Clinics in Sports Medicine (Vol. 35, Issue 4, pp. 679-696). W.B. Saunders.
- Kirby, T. J., McBride, J. M., Haines, T. L., & Dayne, A. M. (2011). Relative net vertical impulse determines jumping performance. Journal of Applied Biomechanics, 27(3), 207-214.
- Knesek, M., Skendzel, J. G., Dines, J. S., Altchek, D. W., Allen, A. A., & Bedi, A. (2013). Diagnosis and management of superior labral anterior posterior tears in throwing athletes. The American Journal of Sports Medicine, 41(2), 444-460.
- Kottner, J., Audige, L., Brorson, S., Donner, A., Gajewski, B. J., Hróbjartsson, A., Roberts, C., Shoukri, M., & Streiner, D. L. (2011). Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. International Journal of Nursing Studies, 48(6), 661-671.
- Laudner, K., & Sipes, R. (2009). The Incidence of Shoulder Injury among Collegiate Overhead Athletes. Journal of Intercollegiate Sport, 2(2), 260-268.
- Logerstedt, D., Grindem, H., Lynch, A., Eitzen, I., Engebretsen, L., Risberg, M. A., Axe, M. J., & Snyder-Mackler, L. (2012). Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. The American Journal of Sports Medicine, 40(10), 2348-2356.
- Mascarin, N. C., de Lira, C. A. B., Vancini, R. L., Pochini, A. de C., da Silva, A. C., & Andrade, M. dos S. (2017). Strength training using elastic bands: Improvement of muscle power and throwing performance in young female handball players. Journal of Sport Rehabilitation, 26(3), 245-252.
- McCall, A., Nedelec, M., Carling, C., le Gall, F., Berthoin, S., & Dupont, G. (2015). Reliability and sensitivity of a simple isometric posterior lower limb muscle test in professional football players. Journal of Sports Sciences, 33(12), 1298-1304.
- McFarland, E. G., Hsu, C. Y., Neira, C., & O’Neil, O. (1999). Internal impingement of the shoulder: A clinical and arthroscopic analysis. Journal of Shoulder and Elbow Surgery, 8(5), 458-460.
- Nagai, T., Schilaty, N. D., Laskowski, E. R., & Hewett, T. E. (2020). Hop tests can result in higher limb symmetry index values than isokinetic strength and leg press tests in patients following ACL reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 28(3), 816-822.
- Niederbracht, Y., Shim, A. L., Sloniger, M. A., Paternostro-Bayles, M., & Short, T. H. (2008). Effects of a Shoulder Injury Prevention Strength Training Program on Eccentric External Rotator Muscle Strength and Glenohumeral Joint Imbalance in Female Overhead Activity Athletes. Journal of Strength and Conditioning Research, 22(1), 140-145.
- Ortega, D. R., Rodríguez Bíes, E. C., & Berral de la Rosa, F. J. (2010). Analysis of the vertical ground reaction forces and temporal factors in the landing phase of a countermovement jump. Journal of Sports Science and Medicine, 9(2), 282-287.
- Rohman, E., Steubs, J. T., & Tompkins, M. (2015). Changes in Involved and Uninvolved Limb Function During Rehabilitation After Anterior Cruciate Ligament Reconstruction: Implications for Limb Symmetry Index Measures. American Journal of Sports Medicine, 43(6), 1391-1398.
- Sirota, S. C., Malanga, G. A., Eischen, J. J., & Laskowski, E. R. (1997). An eccentric- and concentric-strength profile of shoulder external and internal rotator muscles in professional baseball pitchers. The American Journal of Sports Medicine, 25:59-64.
- Snyder, S. J., Karzel, R. P., Pizzo, W. del, Ferkel, R. D., & Friedman, M. J. (1990). SLAP lesions of the shoulder. Arthroscopy: The Journal of Arthroscopic and Related Surgery, 6:274-279.
- Stickley, C. D., Hetzler, R. K., Freemyer, B. G., & Kimura, I. F. (2008). Isokinetic peak torque ratios and shoulder injury history in adolescent female volleyball athletes. Journal of Athletic Training, 43(6), 571-577.
- van der Hoeven, H., & Kibler, W. B. (2006). Shoulder injuries in tennis players. In British Journal of Sports Medicine (Vol. 40:435-440). British Association of Sport and Excercise Medicine.
- Weber, A. E., Kontaxis, A., O’Brien, S. J., Bedi, A. (2014a). The biomechanics of throwing: Simplified and cogent. In Sports Medicine and Arthroscopy Review (Vol. 22:72-79). Lippincott Williams and Wilkins.
- Weber, A. E., Kontaxis, A., O’Brien, S. J., & Bedi, A. (2014b). The Biomechanics of Throwing. Sports Medicine and Arthroscopy Review, 22:72-79.
- Wilk, K. E., Arrigo, C. A., Hooks, T. R., & Andrews, J. R. (2016). Rehabilitation of the Overhead Throwing Athlete: There Is More to It Than Just External Rotation/Internal Rotation Strengthening. PM&R, 8(3S), S78-S90.
- Wilk, K. E., Ellenbecker, T. S., & Macrina, L. C. (2015). Rehabilitation of the Overhead Athlete’s Elbow. In Elbow Ulnar Collateral Ligament Injury (pp. 227-259). Springer US.
- Wilk, K. E., Meister, K., & Andrews, J. R. (2002). Current concepts in the rehabilitation of the overhead throwing athlete. The American Journal of Sports Medicine, 30(1), 136-151.
- Wong, T. T., Lin, D. J., Ayyala, R. S., & Kazam, J. K. (2017). Elbow Injuries in Adult Overhead Athletes. American Journal of Roentgenology, 208: W110-W120.
- Wright, A. A., Hegedus, E. J., Tarara, D. T., Ray, S. C., & Dischiavi, S. L. (2018). Exercise prescription for overhead athletes with shoulder pathology: A systematic review with best evidence synthesis. In British Journal of Sports Medicine (Vol. 52:231-237). BMJ Publishing Group.
- Yeh, M.-L., Lintner, D., & Luo, Z.-P. (2005). Stress distribution in the superior labrum during throwing motion. The American Journal of Sports Medicine, 33:395-401.