Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
The Influence of Kyphosis on Kinematics and Kinetics during Turning in the Elderly
Wataru Yamazaki1, 2*, Yasuhiko Hatanaka1
1Graduate School of Health Science, Suzuka University of Medical Science, 1001-1 Kishioka-cho, Suzuka-shi, Mie, Japan
2Department of Physical Therapy, Faculty of Health Sciences, Kansai University of Health Sciences, 2-11-1, Wakaba, Kumatori-cho, Osaka, Japan
Received Date: January 11, 2021; Accepted Date: February 05, 2021; Published Date: March 01, 2021
*Corresponding author: Wataru Yamazaki, Graduate School of Health Science, Suzuka University of Medical Science, 1001-1 Kishioka-cho, Suzuka-shi, Mie, Japan. / Department of Physical Therapy, Faculty of Health Sciences, Kansai University of Health Sciences, 2 -11-1, Wakaba, Kumatori-cho, Osaka, Japan. Tel: +81593839208; Fax: +81593839666; Email: w.yamazaki@kansai.ac.jp
Citation: Yamazaki W, Hatanaka Y (2021) The Influence of Kyphosis on Kinematics and Kinetics during Turning in the Elderly. Adv Ortho and Sprts Med: AOASM-135.
Abstract
Elderly people with kyphosis are at increased risk of falling when walking. In particular, there is a tendency to fall when turning. Knowledge of strategies which the elderly with kyphosis could use to turn without falling would be helpful for preventing falls. Therefore, the purpose of this study was to describe strategies of turning in elderly individuals with kyphosis based on investigation of kinematics and kinetics by motion analysis. Forty elderly participants (20 with kyphosis, 20 controls) aged 65 years and over were recruited for this study. The participants were able to walk independently and were attending outpatient rehabilitation or community day-care centers. We measured ground reaction force and joint coordination using force plates and a motion capture system during participants’ turns. We found that hip extension, adduction, and first metatarsophalangeal extension angle were significantly smaller in the kyphosis group, moreover, walking velocity before turning was also lower. Thus, turning in the elderly with kyphosis changed into a short-arc and slow-velocity pattern. Meanwhile, propulsive impulse and ankle plantar flexion moment were significantly larger in the kyphosis group, which was necessary to accelerate body movement again after turning. We considered that short-arc and slow-velocity turning enabled the elderly with kyphosis to turn stably by reducing centrifugal force. Accelerating body movement again after performing a slow turn was also necessary to maintain stability in the turn. In this study, we clarified the strategies of turning used by elderly people with kyphosis to prevent falling, based on kinematics and kinetics. The results of this study could be effectively utilized to prevent falls when turning in patients who have difficulty in improving their kyphosis.
Keywords: Biomechanics; Elderly; Kinematics; Kinetics; Kyphosis; Turning
Introduction
It is important for elderly people to be able to perform turns without risk of falling. Approximately 30% of community-dwelling elderly people suffer falls at least once a year [1] and falling results in hospitalization or outpatient rehabilitation which reduces the daily activities of the elderly [2, 3]. In particular, kyphosis, which is a characteristic posture of the elderly, increases the risk of falls. Aging increases the rate of kyphosis in the population [4] and it has been reported that the estimated proportion of community-dwelling elderly with kyphosis is 20% to 40% [5]. Kyphosis brings the center of mass (COM) close to the limit of stability and reduces balance and walking ability [6, 7]. Conditions that are related to kyphosis in the elderly include reduced walking velocity, stride length, range of motion limitations in the hip and the knee, and decreased muscle strength in the hip and the knee [7-11]. As a result, elderly people with kyphosis are more likely to suffer falls during walking [11, 12]. When walking, turning often causes falls in the elderly because of the greater requirement for dynamic balance ability compared to straight walking [13-15]. Turning has been divided into step turns and spin turns by Hase [16]. The step turn involves a change in direction opposite to the stance limb, while the spin turn involves a change in direction toward the same side as the stance limb. A spin turn is potentially destabilizing because the COM will be outside the base of support [17, 18] and requires more exertion of the lower extremity muscle strength compared to a step turn [19, 20]. Therefore, the spin turn is a motion with a particularly high risk of falls when turning.
However, the type of movement change which occurs in the spin turn as a result of kyphosis has not been clarified. Consequently, it is necessary to analyze the influence of kyphosis during spin turns in the elderly based on kinematics and kinetics. The rotation of the pelvis in the stance phase is an important movement for turning the body [7, 12], and body movement needs to be decelerated in the stance phase during spin turns [16, 21, 22]. We infer from the characteristics of kyphosis that the posterior shift of the COM causes changes in movement of the lower extremity and in the joint moment as well as deceleration and acceleration of body movements. Therefore, the purpose of this study was to clarify, from the analysis of kinematics and kinetics, what kind of strategy was adopted by the elderly with kyphosis to enable them to perform a spin turn without falling. The results of this study are expected to contribute to fall prevention in elderly patients with kyphosis.
Methods
Participants
Twenty elderly volunteers with kyphosis, and 20 age-matched control subjects participated in this study. All participants were aged 65 years or over, were able to walk with no assistance and were attending outpatient rehabilitation or community day-care centers (Table 1). All participants could perform a Timed up & Go test within 13.5 seconds, and we confirmed using the method of Milne [23] that the elderly participants with kyphosis had an index of kyphosis of 13 and over. Exclusion criteria were; 1) severe pain during movement, 2) prominent deformation of the lower extremity, 3) history of neurological disease, 4) cognitive disorder, or 5) a history of orthopedic disease other than spinal column disease within the previous 6 months. This study was conducted with the approval of the Suzuka University of Medical Science and Kansai University of Health Sciences ethics committee (Authorization number: 405, 19-06), written informed consent was obtained from all patients and the rights of the participants were protected.
Control (n=20) Mean ± SD
Kyphosis (n=20) Mean ± SD
Age (years)
74.21±4.89
76.30±7.78
Gender (n (%))
Male
12(60)
7(35)
Female
8(40)
13(65)
Height (cm)
156.61±7.50
154.22±7.21
Mass (kg)
56.28±7.11
53.54±8.24
Index of kyphosis
7.12±2.55
16.44±2.33
Instrumentation
Three force plates (BP400600, 400 × 600 mm, AMTI, Inc., Watertown, MA, USA) installed in the walkway were used to measure ground reaction force, and a ten-camera motion capture system (Vicon Motion Systems Ltd., Oxford, UK) was used to measure joint coordination during spin turns. At the start of the measurement operation, the forward/backward direction was Y+/Y-, the right/left direction was X+/X-, and the upward/downward direction was Z+/Z-. The sampling frequency was set at 100 Hz. Joint coordination was measured by tracing infrared reflective markers with a diameter of 15 mm attached to the subject using 10 charge-coupled device (CCD) cameras. Reflective markers were placed according to plug-in gait model marker placement, as well as at the bilateral medial malleolus, first metatarsal head, and midpoint of the proximal phalange (Figure 1).
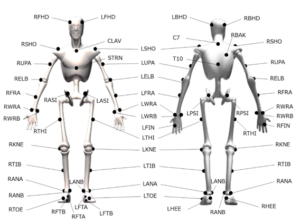
Figure 1: Marker placement.
RFHD : right forehead.
LFHD : left forehead.
RBHD : right back of head.
LBHD : left back of head.
C7 : 7th cervical vertebra.
T10 : 10th thoracic vertebra.
CLAV : clavicle.
STRN : sternum.
RBAK : right back of scapula.
RSHO : right shoulder.
LSHO : left shoulder.
RUPA : right midpoint of upper arm.
LUPA : left midpoint of upper arm.
RELB : right elbow.
LELB : left elbow.
RFRA : right midpoint of forearm.
LFRA : left midpoint of forearm.
RWRA : right styloid process of radius.
LWRA : left styloid process of radius.
RWRB : right styloid process of ulna.
LWRB : left styloid process of ulna.
RFIN : right 2ndmetacarpal head.
LFIN : left 2nd metacarpal head.
RASI : right superior anterior iliac spine.
LASI : left superior anterior iliac spine.
RPSI : right superior posterior iliac spine.
LPSI : left superior posterior iliac spine.
RTHI : right thigh.
LTHI : left thigh.
RKNE : right lateral epicondyle of the femur.
LKNE : left lateral epicondyle of the femur.
RTIB : right midpoint of shank.
LTIB : left midpoint of shank.
RANA : right lateral malleolus.
LANA : left lateral malleolus.
RANB : right medial malleolus.
LANB : left medial malleolus.
RHEE : right calcaneus ridge.
LHEE : left calcaneus ridge.
RTOE : right 2nd metatarsal head.
LTOE : left 2nd metatarsal head.
RFTA : right 1st metatarsal head.
LFTA : left 1st metatarsal head.
RFTB : right midpoint of proximal phalange.
LFTB : left midpoint of proximal phalange.
Measurement Protocol
All participants walked on a 4 m walkway at a self-selected speed, then stepped on force plates in the center of the walkway in the order of right, left, and right. The stance phase during which the foot contacted the force plates was defined as Rt1 (first right stance phase), Lt1 (left stance phase), and Rt2 (second right stance phase), then the participants were asked to perform a spin turn clockwise during Rt2 (Figure 2). The participants practiced several times before the measurement and the spin turn was measured three times for each participant (Figure 3)
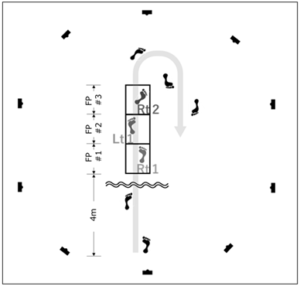
Figure 2: Measurement layout.
- The participants walked on a 4 m walkway at a self-selected speed from installed center of walkway force plates.
- A spin turn was performed with the right foot in contact with FP#3, then the participant was asked to return to the start position.

Figure 3: Spin turn task.
- The spin turn task is shown in stick pictures.
- The right lower extremity is shown in black and the left lower extremity is shown in gray.
- The period during which the foot contacted the force plates was divided into phases as follows; Rt1 is the phase in which the right foot is in contact with FP#1, Lt1 is the phase in which the left foot is in contact with FP#2, and Rt2 is the phase in which the right foot contacted FP#3.
- The period between second heel contact and third heel contact is represented as 100% of the gait cycle.
Data Processing
The trajectory distance of the COM, walking velocity, centrifugal force, ground reaction forces, joint angles, and joint moments were analyzed.
Trajectory Distance of COM
The trajectory distance of the COM was calculated from the placement of reflective markers on each part of the body during each stance phase using the analysis software Nexus2 ver.2.8.1 (Vicon Motion Systems Ltd.). Moreover, the difference in trajectory distance of the COM between Rt1 and Rt2 were compared between the two groups.
Walking Velocity
The walking velocity was the value of the trajectory distance of the COM divided by the time of displacement during each stance phase. Moreover, the difference in walking velocity between Rt1 and Rt2, and Lt1 and Rt2 were compared between the two groups.
Centrifugal Force
The magnitude of the centrifugal force F was defined as:
![]()
m: mass of object,
v: walking velocity,
r: the distance between COM and center of pressure (COP)
The centrifugal force in Rt2 was compared between the two groups.
Ground Reaction Force
The braking impulse generated on deceleration of the body was calculated from the posterior component of the ground reaction force (Fy-) and its action time. The propulsive impulse generated on acceleration of the body was calculated from the anterior component of the ground reaction force (Fy+) and its action time. The braking impulse and propulsive impulse were normalized to each subject’s body mass, and these values were compared between the two groups in the same way as variation of walking velocity.
Joint Angle
The joint angles of the right lower extremity in Rt2 were compared between the two groups; hip extension/flexion, adduction/abduction, internal/external rotation, knee flexion/extension, internal/external rotation, ankle plantar flexion/dorsiflexion, eversion/inversion, first metatarsophalangeal extension, and inside rotation of the pelvis. Moreover, the posterior tilt angle of the pelvis in a standing posture was compared between the two groups. We defined the pelvis, bilateral femurs, shanks, and feet segments from the reflective markers placed on each part of the body using the analysis software Nexus2 ver.2.8.1 (Figure 4). The origin of the pelvis segment was taken as the midpoint of the two anterior superior iliac spine (ASIS) markers. The X axis was the direction from the right ASIS marker to the left ASIS marker. The Y axis was taken as the direction from the midpoint of the two posterior superior iliac spine (PSIS) markers to the midpoint of the two ASIS markers. The Z axis was vertical, perpendicular to the plane which consisted of two ASIS and two PSIS markers (Figure 4 a). The origin of the femur segment was taken as the knee center. The Z axis was taken from the knee center to the hip center. The X axis was taken parallel to the line from the knee center to the knee markers. The Y axis was taken as an axis orthogonal to the Z and X axes (Figure 4 a). The origin of the shank segment was taken as the ankle center. The Z axis was taken from the ankle center to the knee center. The X axis was taken from the ankle center to the shank marker. The Y axis was taken as an axis orthogonal to the Z and X axes (Figure 4 b). The origin of the foot segment was taken as the ankle center. The Y axis was taken from the heel marker to the second metatarsal head marker. The X axis was taken from the ankle center to the lateral malleolus marker. The Z axis was taken as an axis orthogonal to the X and Y axes (Figure 4 c).
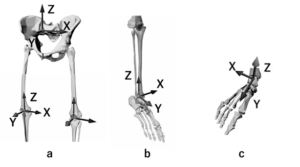
Figure 4: The segment definitions for pelvis, bilateral femurs, shank, and foot are shown. (a) pelvis and femur, (b) shank, (c) foot.
Next, the hip center, knee center and ankle center were calculated according to Bell’s technique [12, 24, 25]. The relative angle between these adjacent segments was calculated by using the Cardan angle in which the rotation order is the Y-X-Z. Then, rotation around the Y axis was defined as adduction/abduction (foot undergoes eversion/inversion), rotation around the X-axis was defined as flexion/extension (plantar flexion/dorsiflexion of the ankle) and rotation around the Z axis was defined as internal/external rotation in each adjacent segment. The rotation of the pelvis was determined between the Y axis of the pelvic segment and the Y axis in the global coordinate system. Similarly, the tilting of the pelvis posteriorly was determined by the angle formed by each Z axis. The first metatarsophalangeal extension and flexion angles were calculated using the arithmetic processing software Vicon Body Builder ver3.6 (Vicon Motion Systems Ltd.). These joint angles were calculated as a relative angle between the following two axes: first, the axis connecting the calcaneal ridge and the first metatarsal head through the midpoint of the line connecting the medial malleolus and the lateral malleolus. Second, the axis connecting the first metatarsal head and the midpoint of the first phalange.
Joint Moment
The maximal values of the following joint moments of the right lower extremity in Rt2 were compared in the two groups: hip extension/flexion, adduction/abduction, internal/external rotation, knee flexion/extension, internal/external rotation, ankle plantar flexion/dorsiflexion, eversion/inversion. The joint moments of the hip, knee, and ankle were calculated by inverse dynamic analysis in which the moment of inertia, mass, and location of the COM were substituted into the joint coordinates and ground reaction force [26-30] using the analysis software Nexus2 ver.2.8.1 (Vicon Motion Systems Ltd.) based on the technique of Winter [24]. The joint moments were normalized to each subject’s body mass.
Statistical Analysis
The variation in trajectory distance of the COM, walking velocity, and braking and propulsive impulse in each phase was compared between the two groups, as well as centrifugal force and the maximal joint angles and joint moments during Rt2. The variation of rotation of the pelvis inside angle from heel contact to toe off during Rt2 was compared between the two groups because of the gradual increase in internal rotation of the pelvis during Rt2. These data used the mean value of three trials in each subject. Non-paired t-tests were used for comparison between the two groups after confirming that the data were normally distributed with equal variance. IBM SPSS Statistical ver.24 statistical analysis software (SPSS, IBM Corp., Armonk, NY, USA) was used for statistical analysis, and the significance level was set at P < 0.05.
Results
Trajectory Distance of the COM
The variation in the difference between Rt1 and Rt2 forward and inside was shorter in the kyphosis group than the control group (P < 0.05) (Table 2). Trajectory distances of the COM in forward and inside directions are shown, which was from the right heel contact to the right toe off during the spin turn (Figure 5).
Control (n=20) Mean ± SD
Kyphosis (n=20) Mean ± SD
Trajectory Distance of COM (mm)
Forward Displacement (Variation from Rt1 to Rt2)
-287.17±91.26
-374.30±74.91*
Inside Displacement (Variation from Rt1 to Rt2)
367.13±78.92
264.67±67.30*
Upward Displacement (Variation from Rt1 to Rt2)
3.27±1.65
4.8±2.98
Walking Velocity (m /sec)
Variation from Rt1 to Rt2
-0.51±0.15
-0.34±0.12*
Variation from Rt1 to Lt1
-0.29±0.10
-0.55±0.12*
Centrifugal Force (N)
824.81±219.17
858.12±294.33
Impulse (N.s /kg)
Braking impulse (variation from Rt1 to Lt1)
-0.23±0.14
-0.29±0.19
Braking impulse (variation from Rt1 to Rt2)
2.23±0.62
0.99±0.27*
Propulsive impulse (variation from Rt1 to Lt1)
-1.13±0.31
-1.96±0.41*
Propulsive impulse (variation from Rt1 to Rt2)
-1.43±0.57
-0.94±0.28*
Joint Angle (degree)
Hip joint
Extension
11.10±4.83
6.10±2.21*
Flexion
26.21±5.82
27.18±4.21
Adduction
12.41±3.91
5.21±2.69*
Abduction
2.52±1.41
5.85±3.01
External rotation
16.23±7.54
19.87±12.06
Internal rotation
6.04±2.32
5.66±3.48
Knee Joint
Flexion
14.63±6.59
22.61±8.75*
External rotation
16.73±7.43
25.39±8.56*
Internal rotation
8.06±2.48
7.63±2.76
Ankle Joint
Plantar flexion
19.51±3.27
14.76±6.27
Dorsiflexion
12.93±4.71
18.62±6.21*
Eversion
3.84±2.91
4.22±1.37
Inversion
4.74±3.41
2.99±2.61
Pelvis
Posterior tilting
7.32±3.22
13.82±6.78*
Internal rotation
57.26±15.90
47.05±12.42*
First metatarsophalangeal Joint
Extension
38.51±6.42
22.11±8.23*
Joint Moment (Nm /kg)
Hip Joint
Extension
0.59±0.25
0.32±0.18*
Flexion
0.48±0.28
0.45±0.31
Adduction
0.82±0.28
0.80±0.37
External rotation
0.14±0.09
0.11±0.05
Internal rotation
0.15±0.10
0.13±0.08
Knee Joint
Extension
0.44±0.21
0.54±0.29*
Flexion
0.56±0.24
0.42±0.22
External rotation
0.22±0.19
0.13±0.11
Internal rotation
0.21±0.15
0.17±0.12
Ankle Joint
Plantar flexion
0.98±0.27
1.18±0.31*
Dorsiflexion
0.15±0.08
0.10±0.09
Eversion
0.16±0.10
0.22±0.11*
Inversion
0.19±0.11
0.18±0.09
- *P <05; non-paired t-test. The variation between Rt1-Lt1 and between Rt1-Rt2 are shown regarding the trajectory distance of the COM, walking velocity, braking impulse, and propulsive impulse.
- Internal rotation of the pelvis is also shown depicting the angle from heel contact to toe off during Rt2 as the variation.
- All joint angles and joint moments are shown as the maximal value.
 Figure 5: Trajectories of the COM in the forward and inside direction from right heel contact to right toe off during a spin turn.
Figure 5: Trajectories of the COM in the forward and inside direction from right heel contact to right toe off during a spin turn.
- Trajectories of the COM in forward and inside directions, from the right heel contact to the left heel contact during a spin turn.
- For a representative subject of each group, the coordinates during right heel contact are shown as the origin.
- The values for the kyphosis group are presented as a solid line, and for the control group as a dotted line.
Walking Velocity
The variation in the difference between Rt1 and Rt2 was smaller in the kyphosis group than in the control group (P < 0.05). Meanwhile, the variation in the difference between Rt1 and Lt1 was higher in the kyphosis group than in the control group (P < 0.05) (Table 2).
Centrifugal Force
There was no difference between the groups in centrifugal force in Rt2 (Table 2).
Ground Reaction Force
The variation in the difference in braking impulse between Rt1 and Rt2 and in propulsive impulse between Rt1 and Rt2 were smaller in the kyphosis group than in the control group (P < 0.05). Meanwhile, the variation in the difference in propulsive impulse between Rt1 and Lt1 was larger in the kyphosis group than in the control group (P < 0.05) (Table 2).
Joint Angle
The maximal hip extension angle, adduction angle, first metatarsophalangeal extension angle, and rotation of the pelvis inside angle were all lower in the kyphosis group than in the control group (P < 0.05). The maximal knee flexion angle, external rotation angle, and ankle dorsiflexion angle were larger in the kyphosis group than in the control group (P < 0.05) (Figure 6). The tilting of the pelvis posteriorly in a standing position was also larger in the kyphosis group than in the control group (P < 0.05) (Table 2).
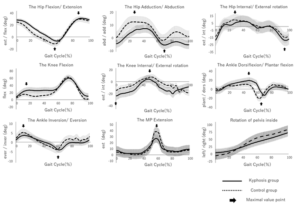
Figure 6: The joint angles in the kyphosis group and the control group during a spin turn.
- Mean and SD of joint angles in the right extremity during a spin turn.
- The values for the kyphosis group are presented as a solid line, and for the control group as a dotted line.
- The positions from which the maximal value was extracted are indicated by arrows ( ).
- The maximal value of the knee external rotation was extracted at heel contact.
- The value of rotation of pelvis inside was extracted as a variation from heel contact (0%) to heel contact (100%).
Joint Moment
The maximal hip extension moment was smaller in the kyphosis group than in the control group (P < 0.05). The maximal knee extension moment, ankle plantar flexion moment, and eversion moment were larger in the kyphosis group than in the control group (P < 0.05) (Figure 7) (Table 2).
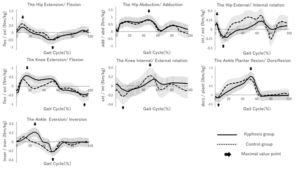
Figure 7: The joint moments in the kyphosis group and control group during a spin turn.
- Mean and SD are shown in joint moments in the right extremity during a spin turn.
- The values for the kyphosis group are presented as a solid line, and for the control group as a dotted line.
- The positions at which maximal value was extracted are indicated by arrows ( ).
Discussion
Kyphosis caused a change in the pattern of a spin turn into a short-arc and slow-velocity movement. The COM moved away from the COP because of the shifting COM anteromedially at mid stance or later in the pivot foot of the spin turn. The shortening of the distance of the anterior shift of the COM in the elderly with kyphosis indicated that a spin turn was performed in a short arc. Moreover, the velocity of the COM had already decelerated before the spin turn started in the elderly with kyphosis. A short-arc and slow-velocity spin turn reduced the centrifugal force acting on the COM at mid stance or later. The centrifugal force could cause the COM to move anterolaterally during a spin turn. Kyphosis caused the COM to move posteriorly and increased the radius of rotation of the COM around the COP; meanwhile, the centrifugal force did not significantly differ between the two groups. Therefore, we considered that elderly subjects with kyphosis performed a spin turn with a short arc and slow velocity, which reduced the centrifugal force to the same magnitude as the control group.
Performing a spin turn with a short arc and slow velocity influenced the movement of the pelvis and lower extremities. Decreasing the maximal angle of hip extension, adduction, and first metatarsophalangeal extension restricted the anterolateral shift of the COM and changed the movement to a short-arc spin turn in the elderly with kyphosis. In addition, internal rotation of the pelvis decreased during the stance phase of the pivot foot in the elderly subjects with kyphosis. The internal rotation of the pelvis in stance phase of the pivot foot was driven by rotation of the foot on the floor with the ball of the foot as the axis as well as by hip internal rotation and knee internal rotation [31]. The first metatarsophalangeal extension at mid stance or later in the pivot foot involved lifting the heel off the ground due to rotation of the foot on the floor with the ball of the foot as the axis. However, tilting of the pelvis posteriorly, which occurs in kyphosis, restricted extension of the hip and the first metatarsophalangeal joint [31, 32]. Therefore, we considered that internal rotation of the pelvis was restricted by the limitation of heel lifting, and then, tilting of the pelvis posteriorly, caused by kyphosis, restricted the ability to take the heel off the ground. On the other hand, internal rotation of the pelvis in the elderly with kyphosis was compensated for by knee internal rotation at heel contact or later in the pivot foot. The differences in the maximal angle of the knee during external rotation and internal rotation in the two groups indicated that the knee internal rotation occurred significantly at heel contact or later of the pivot foot in elderly subjects with kyphosis. The knee internal rotation meant rotation of the tibia internally against the femur or rotation of the femur externally against the tibia. The knee internal rotation in the pivot foot of the spin turn was rotation of the femur externally against the tibia and rotation of the pelvis on the same side with external rotation of the femur. The knee internal rotation compensated for the decrease of internal rotation of the pelvis in the pivot foot and then elderly subjects with kyphosis were able to perform a short-arc spin turn.
The mechanism of deceleration in the pivot foot of the spin turn changed the movement to a slow-velocity spin turn in the elderly with kyphosis. The elderly with kyphosis had already entered the loading response of the pivot foot with deceleration by reducing the kicking off from the ground on the exterior foot at terminal stance or later. It was necessary to decelerate body movement in the stance phase of the pivot foot to perform a short-arc spin turn and reduce the centrifugal force in the spin turn. Comparing the propulsive impulse on the exterior foot between the two groups, we found that it decreased in the elderly with kyphosis. Hase et al. reported that it was necessary to decelerate due to the posterior shift of the COM in the pivot foot of the spin turn [16], however, the hip extension moment was not been affected because the body movement had already decelerated at the exterior foot in the elderly with kyphosis. From the above, it can be seen that the elderly with kyphosis decelerated body movement during the terminal stance or later of the exterior foot before heel contact of the pivot foot more than the control group. Moreover, the ankle inversion moment and the knee extension moment both increased in the elderly with kyphosis because decreasing the shifting COM anteromedially on the pivot foot caused the ground reaction force vector on the pivot foot to pass inside the ball of the foot and posterior to the knee. Increasing the knee flexion and ankle dorsiflexion angles needed to compensate for shifting the COM posteriorly, a characteristic posture of the elderly with kyphosis. Meanwhile, the elderly with kyphosis showed accelerated body movement compared to the control group at the terminal stance or later in the pivot foot because of increased walking velocity, propulsive impulse, and ankle plantar flexion moment. Acceleration in the terminal stance or later during a spin turn restored decelerated body movement steadily and was necessary to perform the spin turn. Therefore, we considered the elderly with kyphosis who decelerated their body movement until mid-stance of the pivot foot needed to accelerate their body movement again more at terminal stance or later. The elderly with kyphosis reached the pre-swing stage of the with an increased foot angle after reaching heel contact. Increasing the foot angle at pre swing of the pivot foot provided a greater ankle plantar flexion moment for kicking the ground. We considered that increasing the foot angle at heel contact of the pivot foot was a factor related to promotion of foot plantar flexion moment.
The purpose of this study was to clarify, based on analysis of the kinematics and kinetics, what kind of strategy was adopted by the elderly with kyphosis in order to perform spin turns without falling. Kyphosis causes falling due to poor balance as a result of the posterior shift in the COM. However, the elderly with kyphosis in this study were able to perform spin turns without falling, using three strategies as follows. The first strategy was to reach heel contact of the pivot foot once they had already decelerated by decreasing kicking from the ground at terminal stance or later. The muscle activity of the hip extensor at loading response of the pivot foot decreased in the elderly with kyphosis, which restricted deceleration of body movement. The elderly with kyphosis reached loading response of the pivot foot with already decelerating body movement by reducing kicking from the ground by the exterior foot. The second strategy was to rotate the knee internally at pivot foot to compensate for insufficient internal rotation of the pelvis. The pelvis rotated internally at pivot foot as an axis, which was necessary to shift the COM anteromedially. Increasing the internal rotation of the knee exerted further internal rotation of the pelvis and compensated for the anteromedial shift of the COM. These strategies reduced centrifugal force at mid stance or later in the pivot foot by reducing walking velocity and shifting the COM anteromedially. We considered that reducing centrifugal force prevented anterolateral shift of the COM and was performed by the elderly with kyphosis to enable them to make spin turns without falling. The third strategy was to kick the ground at the pivot foot by exerting the ankle plantar flexion moment to accelerate body movement at terminal stance or later. The body movement which decelerated until the loading response of the pivot foot later accelerated again at terminal stance or later and it participated in keeping the body balance steady [7]. We estimated that it was necessary to accelerate body movement again before the spin turn so as to prevent falling as well as to decelerate body movement later in the spin turn.
Overall, we concluded that the three strategies revealed by this study were strategies enabling the elderly with kyphosis to perform spin turns without falling. The kyphosis was caused by irreversible changes to the spinal column, which made it difficult to radically improve the posture. However, muscle strength in the knee and the ankle tended to be conserved in the elderly with kyphosis [19]. Based on the findings in this study, we considered that maintaining the range of motion and muscle strength of the knee and the ankle could be effective in preventing falling during spin turns in patients who had difficulty in improving their kyphosis.
Conclusion
In this study we analyzed strategies to enable the elderly with kyphosis to perform spin turns without falling based on analysis of kinematics and kinetics. In the elderly with kyphosis, the distance that the COM shifted anteromedially in the pivot foot was shortened and walking velocity was already decelerated before the spin turn started. These results showed that the spin turn changed into a short-arc and slow-velocity pattern. We considered that a short-arc and slow-velocity spin turn reduced the centrifugal force causing the COM to move laterally, and thus enabled the spin turn to be performed steadily in the elderly with kyphosis. A short-arc and slow-velocity spin turn was made possible by three strategies: reduced kicking off the ground by the exterior foot, increased internal rotation of the knee in the pivot foot, and increased kicking off the ground in the pivot foot. Knowledge of these three strategies based on kinematics and kinetics will be helpful in considering what motor function is required to prevent falling in the elderly.
Conflict of interest
We declare that there are no competing interests associated with the research reported within this manuscript. No source of funding was used in the undertaking of this study or the preparation of this manuscript.
Author Contributions
Wataru Yamazaki: Conceptualization, Data Curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Visualization, Writing – Original Draft, Writing – Review & Editing.
Yasuhiko Hatanaka: Conceptualization, Data Curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – Original Draft, Writing – Review & Editing.
References
- Sattin RW (1992) Falls among older persons: a public health perspective. Annu Rev Public Health 13: 489-508.
- Tinetti ME, Williams CS (1997) Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl 337: 1279-1284.
- Stevens JA, Corso PS, Finkelstein EA, Miller TR (2005) The costs of fatal and non-fatal falls among older adults. InjPrev 12: 290-295.
- Sinaki M, Brey RH, Hughes CA, Larson DA, Kaufman KR (2005) Balance disorder and increased risk of falls in osteoporosis and kyphosis. Osteoporos Int 16: 1004-1010.
- Kado DM, Prenovost K, Crandall C (2007) Narrative review: hyperkyphosis in older persons. Ann Intern Med 147: 330-338.
- Lynn SG, Sinaki M, Westerlind KC (1992) Balance characteristics of persons with osteoporosis. Arch Phys Med Rehabil 78: 273-277.
- Overstall PW, Exton-Smith AN, Johnson AL (1977) Falls in the elderly related to postural imbalance. Br Med J 1: 261-264.
- Kim SB, Kim WJ, Kang JW, Kang SI, Park KY (2010) Change of pelvic tilt before and after gait in patients with lumbar degenerative kyphosis. Journal of Korean Society of Spine Surgery 16: 95-103.
- Demarteau J, Jansen B, Keymolen BY, Mets T, Bautmans I (2019) Trunk inclination and hip extension mobility, but not thoracic kyphosis angle, are related to 3D-accelerometry based gait alterations and increased fall-risk in older persons. Gait posture 72: 89-95.
- Kado DM, Huang MH, Connor EB, Greendale GA (2005) Hyperkyphotic posture and poor physical functional ability in older community-dwelling men and women: The rancho bernardo study. J GerontolA Biol Sci Med Sci 60: 633-637.
- Kado DM, Prenovost K, Crandall C (2007) Narrative review: Hyperkyphosis in older persons. Ann Intern Med 147: 330-338.
- Davis RB, Ounpuu S, Tyburski D, Gage JR (1991) A gait analysis data collection and reduction technique. Human Movement Science 10: 575-587.
- Tinetti ME, Speechley M, Ginter SF (1998) Risk factors for falls among elderly persons living in the community. N Engl J Med 319:1701-1707.
- Cumming RG, Klineberg RJ (1994) Fall frequency and characteristics and the risk of hip fractures. J Am Geriatr Soc 42: 774-778.
- Wright RL, Peters DM, Robinson PD, Sitch AJ, Watt TN, et al. (2012) Differences in axial segment reorientation during standing turns predict multiple falls in older adults. Gait Posture 36: 541-545.
- Hase K, Stein RB (1999) Turning strategies during human walking. J Neurophysiol 81: 2914-2922.
- Akram SB, Frank JS, Chenouri S (2010) Turning behavior in healthy older adults: is there a preference for step versus spin turns? Gait Posture 31: 23-26.
- England SE, Verghese J, Mahoney JR, Trantzas C, Holtzer R (2010) Three-level rating of turns while walking. Gait Posture 41: 300-303.
- Kasukawa Y (2017) Age-related changes in muscle strength and spinal kyphosis angles in an elderly Japanese population. Clinical interventions in aging 12: 413-420.
- Yamada M, Higuchi T, Mori S, Uemura K, Nagai K, et al. (2012) Maladaptive turning and gaze behavior induces impaired stepping on multiple footfall targets during gait in older individuals who are at high risk of falling. Arch Gerontol Geriatr 54: 102-108.
- Glaister BC, Orendurff MS, Schoen JA, Bernatz GC, Klute GK (2008) Ground reaction forces and impulses during a transient turning maneuver. J Biomech 41: 3090-3093.
- Orendurff MS, Bernatz GC, Schoen JA, Klute GK (2008) Kinetic mechanisms to alter walking speed. Gait Posture 27: 603-610.
- Milne JS, Lauder IJ (1974) Age effects in kyphosis and lordosis in adult. Ann Hum Biol 1: 327-337.
- Winter DA, Patla AE, Prince F, Ishac M, Gielo-Perczak K (1998) Stiffness control of balance in quiet standing. J Neurophysiol 80: 1211-1221.
- Bell AL, Pedersen DR, Brand RA (1990) A comparison of the accuracy of several hip center location prediction methods. J Biomech 23: 617-621.
- Kadaba MP, Ramakrishnan HK, Wootten ME (1987) Lower extremity joint moments and ground reaction torque in adult gait. Biomechanics of normal and prosthetic gait 4: 87-92.
- Kadaba MP, Ramakrishnan HK, Wootten ME, Gainey J, Gorton G, et al. (1989) Repeatability of kinematic, kinetics and electromyographic data in normal adult gait. Journal of Orthopaedic Research 7: 849-860.
- Kadaba, MP, Ramakrishnan HK, Wooten ME (1990) Lower extremity kinematics during level walking. Journal of Orthopaedic Research 8: 383-392.
- Ramakrishnan HK, Masiello G, Kadaba MP (1991) On the estimation of the three dimensional joint moments in gait. Biomechanics Symposium, ASME 120: 333-339.
- Winter DA (2002) Biomechanics and motor control of human movement. John Wiley & Sons. Print ISBN:9780470398180 |Online ISBN:9780470549148
- Thigpen MT, Light KE, Creel GL, Flynn SM (2000) Turning difficulty characteristics of adults aged 65 years or older. Phys Ther 80: 1174-1187.
- Maki BE and McIlroy WE (2006) Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age and ageing 35: 12-18.