Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Screw Penetration in the Operative Management of Distal Radial Fractures, the Pitfalls of Peri-Operative Imaging and the Effect on Rehabilitation and Sporting Function
Erden Ali1*, John Hambidge2
1Magdalene College, Magdalene Street, Cambridge, CB3 0AG. University of Cambridge, United Kingdom
2Queens Hospital, Romford, Essex, United Kingdom
Received Date: June 26, 2020; Accepted Date: July 02, 2020; Published Date: July 10, 2020
*Corresponding author: Erden Ali, Magdalene College, University of Cambridge, Magdalene Street, Cambridge CB3 0AG, United Kingdom. Tel: +4401223332100; Email: erden@doctors.org.uk
Citation: Ali E, Hambidge J (2020) Screw Penetration in the Operative Management of Distal Radial Fractures, the Pitfalls of Peri-Operative Imaging and the Effect on Rehabilitation and Sporting Function. Adv Ortho and Sprts Med: AOASM-125.
Abstract
An ever demanding patient population and introduction of newer techniques and technologies, brings with it new challenges. Distal radial fractures are a common condition encountered amongst trauma and orthopedic surgeons and those who sustain this injury desire early mobilisation, quick return to work and adequate function. Whilst it has been proven to be a successful treatment modality, it is associated with potential side effects most notable articular screw penetration and tendinopathy from suboptimal screw placement. The literature is permeated with articles demonstrating the use of specific intra-operative imaging to assess intra-articular screw penetration in surgical fixation of the distal radius fracture however these studies have largely used cadaveric models. We present an interesting study of the pitfalls of intra-operative imaging on a saw bones model. Ominously, we were able to hide screw penetration with standard intra-operative views which are taken in order to ensure screw penetration is not achieved. The effect of this on a patient’s ability to rehabilitate accordingly cannot be underestimated.
Introduction
Fractures of the distal radius represent one of the most common orthopedic injuries encountered making up some 15-20% of all fractures [1], with 50% of this displaying intra-articular extension [1]. As with all the majority of trauma injuries, a bimodal distribution exists with regards incidence as young patients sustain these injuries via high energy transfer and elderly patients with lower impacts such as a fall from standing. Treatment modalities vary from conservative measures such as closed manipulation and casting, to surgical intervention such as closed manipulation and fixation with Kirschner wires or open reduction and internal fixation (O.R.I.F.) using plates and screws.
Whilst a definitive treatment plan is lacking in an elderly population [2, 3] it is widely accepted that these injuries can be inherently unstable with casting alone proving insufficient to maintain fracture reduction [4]. An injury more commonly seen in the elderly population, treatment goals vary in this age category. Those who lead a less active lifestyle are able to tolerate a reduction of function, with attainment of pain relief being the mainstay of treatment. Younger active patients who demand a more active lifestyle warrant a more aggressive approach requiring O.R.I.F. and anatomical reduction of the articular surface being the objective of treatment. It is this patient cohort that this document is focused on.
Screw length and penetration of the articular surface is a concern when performing distal radial ORIF [5, 6]. Patients who undergo wrist ORIF are often of a younger and more active persuasion who take part in sporting recreation. Much has been done in the literature to suggest optimal imaging for detection of screw penetration [7-9]. With inadequate screw position in distal radial fractures, it is not only destruction of the joint surface and obstruction to movement that poses a potential greater threat to long term outcome but further surgeries in order to remove malpositioned metalwork leads to greater surgical destruction and scar tissue formation.
Anatomy
The distal radius possesses three separate articular surfaces; these are the scaphoid and lunate facets and the sigmoid notch. The latter forms the distal radioulnar joint (D.R.U.J.) with its articulation with the ulna and is located on the radius’ ulna aspect proximal to the lunate facet. The scaphoid and lunate facets articulate with the corresponding carpal bones respectively. The triangular fibro cartilage complex (T.F.C.C.) articulates with the lunate and triquetrum providing support at the ulna aspect of the wrist.
A complicated pivot joint responsible for pronation and supination, 80% of axial load is supported by the radius with the remaining 20% by the ulna. Variation in radial alignment can lead to an increase in the load transferred to the ulna. Radial deformity alters wrist kinematics, especially shortening, which in turn alters load transfer.
With fractures of the distal radius, ligamentous attachments remain intact which permits ligament taxis fracture reduction. Brachioradialis acts as a deforming force and is a solitary muscle attaching to the distal radius, its release is often warranted in order to achieve fracture reduction.
Methods of Fixation and Volar Locking Plates
Fracture pattern, level of function, age and bone quality will dictate which method of fixation is adopted. Those that are available include closed reduction and percutaneous pinning, external fixation, dorsal plating and volar fixed-angle plating. Low profile, fixed-angle devices provide an excellent option for treatment of distal radial fractures and are seen as a major improvement in orthopedic surgery. This document is aimed at volar locking plates.
This method of surgical fixation has gained popularity due to satisfactory surgical outcomes. Locked distal screws provide support and stabilisation to the distal comminuted fragments whilst proximal fixation of the plate permits a stable three-dimensional construct. These devices provide inherent stability based on the metal-bone construct and can therefore also be utilised with less comminuted fractures that exhibit instability. Specific advantages when utilising this method of fixation include direct fracture reduction allied with stable fixed-angle support thereby permitting early active wrist rehabilitation. Biomechanical data suggests that when these devices are loaded to failure, volar fixed-angle plates demonstrate significantly increased strength when compared to dorsal plating [10]. This method of fixation has proved advantageous in elderly osteopaenic patients, for high-energy comminuted fractures and patients who have developed fracture mal-union warranting osteotomy..
Whilst they have proven very successful in the treatment of distal radial fractures, complications such as flexor pollicis tendon rupture [11] do exist due to inadequate screw penetration. It is the role of intra-operative fluoroscopy allied with surgical technique that is used to ensure this complication does not occur. However, despite standard intra-operative imaging, screw penetration can be missed.
Objective
To demonstrate standard intra-operative imaging used in the detection of articular screw penetration, when performing fixation of distal radial fractures, can miss breaches of the articular surface due to metalwork.
Materials and Methods
We performed a prospective study in conjunction with the local radiology department. Ethical approval was not required as patients were not used directly in this investigation. Data was gathered prospectively and images were taken in conjunction with local radiology policy. In order to objectify the study, a different surgeon elected to select the saw bones model which was going to represent a distal radius demonstrating articular screw penetration.
Using saw bones, a volar locking plate was applied using 4 distal locking screws and 1 proximal screw to a distal radius and ulna model. By the same surgeon who had selected the model. The distal locking screws were inserted in such a manner that each penetrated the corresponding cortical bone or the articular surface (Figure 1).
4 surfaces of the distal radius were perforated with screws manually under the guidance of the image intensifier; these were the radio-ulna joint, radial articular surface, ulna radial border and the dorsal radial surface. (Figure 1) demonstrates the sites of the screw penetration and the model that was used to assess screw position. Using this saw bones model and the image intensifier a different surgeon used fluoroscopic images in order to assess if screw penetration was visible using this standard intra-operative technique. Standard views were taken and those that would not usually be possible as the saw bones model allowed a greater degree of freedom than is usually tolerable when operating on patients. This was done to accurately assess if screw penetration could have been masked.
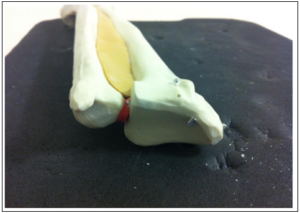
Figure 1: Saw bones model demonstrating screw penetration of the distal radius. The articular surface has clearly been breached.
Results
Under image intensification, images demonstrated that screw penetration had not occurred. As exampled by (figure 1), the degree of screw penetration witnessed on the imaging was significantly underestimated.
(Figure 2) is an oblique image taken of the distal radius, a radial to medial Kirshner wire has been placed for positional orientation. The image demonstrates all screws to be adequately positioned within bone.
(Figure 3) is an anteroposterior view taken of the corresponding saw bones model. When correlated with figure 1, the degree of screw penetration is again masked.
(Figure 4) represents a true lateral view. The degree of metalwork within the joint remains hidden.

Figure 2: Oblique view demonstrating underestimation of screw penetration with screws appearing within bone.
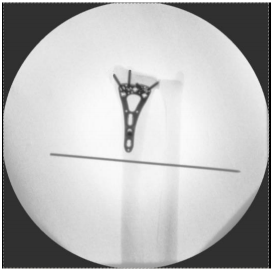
Figure 3: Antero-posterior view demonstrates screw penetration is masked.

Figure 4: A true lateral view of the saw bones model with an equivalent volar locking plate applied.
Conclusion
The authors have demonstrated that screw penetration was masked when using standard intra-operative views for assessment of the articular surface during ORIF of the distal radius. The model that was used permitted even greater freedom of movement and despite this, screw penetration was missed. This is particularly important as even less movement is afforded when operating on patients which bring even greater risk of missing malpositioned metalwork.
Whilst much data has been produced on how best to visualise screw penetration with the advocation of specific views and comparisons being made of existing ones available [12], it still proves difficult to produce a valid and robust technique to permit exclusion of intra-operative screw penetration. Our study is a novel examination in assessment of volar locking plate fixation with previous studies utilising cadaveric tissue that has highlighted the difficulties placed with this common place surgical procedure. Surgeons must remain vigilant as patients who require a higher level of wrist movement and function for example in those taking part in racket sports are at greater risk of long term sequelae with inadequate metalwork position.
Discussion
As commented in this document and throughout the literature, use of volar locking plates is increasing in the treatment of distal radial fractures. This increase in its utilisation has brought with it a greater awareness of the complications. Earlier work has highlighted the need for further intra-operative images in addition to standard postero-anterior (PA) and lateral radiographs with anatomically tilted images demonstrating vital supplementary views when assessing screw penetration [13]. Specific supplementary views have been evaluated with the use of computerised Tomography [14] with others advocating specific screw lengths [15].The need for supplemental images in addition to standard AP and lateral images was supported further by an interesting recent study by Patel et al. (2013) [16]. The authors in this study set out to examine the effect of additional lateral tilt images when assessing screw penetration in distal volar locking plate fixation. Their data concluded that supplementary views improved the ability of those evaluating screw lengths, regardless of training level.
Reports of prominent screw tips beyond the dorsal cortex are increasing. An interesting study by Park and Goldie, (2012) [17] commented on the difficulty in assessing screw length on fluoroscopy owing to the size of the valley depth in the intermediate column located between Lister’s tubercle and the sigmoid notch of the distal radius. Using computed tomography (CT) or magnetic resonance imaging (MRI) they discovered that in their assessment of 33 wrists using either treatment modality, 99% of patients possessed a valley depth of at least 2mm. They concluded that when using fluoroscopy peri-operatively, standard lateral views or oblique views were not adequate when assessing screw length.
Maschke et al. (2007) [18] in their cadaveric study have published their results when assessing dorsal screw penetration radiographically. Fixed angle, distal volar locking plates were applied to the upper extremities of eight fresh frozen human cadavers. Lateral, supinated and pronated views were taken fluoroscopically, proceeded by dissections of the wrist and comparisons of screw depth made. They advocated the use of oblique pronosupination views in order to assess screw length with standard postero-anterior and lateral intraoperative radiographs. They demonstrated that for example screws used for the most radial distal locking screw were on average 6.5 mm prominent before radiographic detection for lateral views and 2 mm for supinated views. Pronated views did not detect prominent screws.
Some authors have advocated the implementation of more specific radiographic views when assessing screw penetration [19]. The authors of this particular study commented on an articular wrist series with an antero-posterior (AP) image taken at 11 degrees elevation with a supplementary lateral of 23 degrees elevation. These additional two radiographs permitted a parallel image of the radiocarpal joint to be visualised.
Much work on this important surgical consideration has been documented in the literature. An earlier cadaveric study by Soong et al. (2009) [20] examined screw penetration using a standard PA, tilt PA with 11 degrees elevation, standard lateral and 3 tilt lateral views with 15, 23 and 30 degrees of elevation respectively. They suggested first placing ulnar screws with their position confirmed using lower angle tilt radiographs varying from 15 to 23 degrees. They suggested placement of the radial styloid screw to be performed finally and its evaluation conducted using PA and tilt PA views.
Much work has been performed in order to optimise the surgeon’s ability to assess screw penetration with volar locking late fixation. Some authors have gone on to conclude 15˚ of inclination is optimal for assessment [21], with others stating 20˚ in the horizontal plane and 5˚ in the sagittal plane combined with a radial groove view is best [22]. There are those who have recommended the use of rotational fluoroscopy whilst maintaining that no combination of imaging permits accurate assessment of screw penetration [23]. There is evidence in the literature that three dimensional fluoroscopic imaging may be superior to tangenital views when assessing screw penetration [24] however this modality is not readily available and the authors from the same paper did admit dorsal tangential views are adequate when used accurately and diligently.
Inadequate metalwork position is not acceptable in any patient population but the authors stress the importance in distal radial fracture fixation in this article due to the impact on a younger and more active case mix.
Funding Statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author Contributions: Ali was responsible for substantial contributions to the research design and data acquisition, analysis and interpretation. E. Ali and J. Hambidge were responsible for manuscript drafting and for final version approval.
References
- Black WS, Becker JA (2009) Common forearm fractures in adults. Am Fam Physician 80: 1096-1102.
- Handoll HH, Madhok R (2002) Conservative interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev 2:CD000314.
- Handoll HH, Madhok R (2003) Surgical interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev 3:CD003209.
- Simic PM, Weiland AJ (2003) Fractures of the distal aspect of the radius: changes in treatment over the past two decades. Instr Course Lect 52: 185-195.
- Yuen G, Yee DKH, Fang C, Lau TW, Leung F (2015) Screw Length in Volar Locking Plate Fixation for Distal Radial Fractures. J OrthopSurg (Hong Kong) 23: 164-167.
- Bergsma M, Doornberg JN, Duit R, Saarig A, Worsley D, et al. (2018) Volar plating in distal radius fractures: A prospective clinical study on efficacy of dorsal tangential views to avoid screw penetration. Injury 49: 1810-1815.
- Cha SM, Shin HD (2017) Detections of Screw Penetration during Volar Plating for Distal Radius Fractures. J Wrist Surg 6: 340-348.
- Özbek EA, Ayanoğlu T, Armangil M (2019) How effective is skyline view for avoiding dorsal cortex penetration in volar plate fixation of intra-articular and dorsal cortex comminuted distal radius fractures. Injury 50: 1684-1688.
- Sumner K, Grandizio LC, Schultz S, Klena JC (2019) The 70° Supinated Oblique View: A Cadaveric Analysis to Determine Ideal Radial Styloid Screw Position in Locked Volar Plating of Distal Radius Fractures. Hand (N Y) 1558944719836210 doi:10.1177/1558944719836210
- Smith DW, Henry MHHenry MH (2005) Volar fixed-angle plating of the distal radius. J Am AcadOrthop Surg 13: 28-36.
- Limthongthang R, Bachoura A, Jacoby SM, Osterman AL (2014) Distal radius volar locking plate design and associated vulnerability of the flexor pollicis longus. J Hand Surg Am 39: 852-60.
- Ozer K, Wolf JM, Watkins B, Hak DJ (2012) Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg Am 37: 963-967.
- Boyer MI, Korcek KJ, Gelberman RH, Gilula LA, Ditsios K, et al. (2004) Anatomic tilt x-rays of the distal radius: an ex vivo analysis of surgical fixation. J Hand Surg Am 29: 116-122.
- Diong TW, Haflah NHM, Kassim AYM, Habshi SMIA, Shukur MH (2018) Use of Computed Tomography in Determining the Occurrence of Dorsal and Intra-articular Screw Penetration in Volar Locking Plate Osteosynthesis of Distal Radius Fracture. J Hand Surg Asian Pac 23: 26-32.
- Kilian M, Simkovic P, Zamborsky R, Skoda A, Labas P (2019) What are the ideal screw lengths in volar locking plate fixation for distal radius fractures?. BratislLekListy 120: 505-509.
- Patel A, Culbertson MD, Lahey P, Semenovski M, Choueka J (2013) Improving accuracy and confidence in distal radius volar plate screw placement through supplemental radiography: examining specialty, education, and experience levels. Hand (N Y) 8: 308-314.
- Park DH, Goldie BS (2012) Volar plating for distal radius fractures--do not trust the image intensifier when judging distalsubchondral screw length. Tech Hand Up Extrem Surg 16: 169-172.
- Maschke SD, Evans PJ, Schub D, Drake R, Lawton JN (2007) Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand (N Y 2: 144-150.
- Pace A, Cresswell T (210) Use of articular wrist views to assess intra-articular screw penetration in surgical fixation of distal radius fractures. J Hand Surg Am 35: 1015-1018.
- Soong M, Got C, Katarincic J, Akelman E (2008) Fluoroscopic evaluation of intra-articular screw placement during locked volar plating of the distal radius: a cadaveric study. J Hand Surg Am 33: 1720-1723.
- Haug LC, Glodny B, Deml C, Lutz M, Attal R (2013) A new radiological method to detect dorsally penetrating screws when using volar locking plates in distal radial fractures. The dorsal horizon view. Bone Joint J 95: 1101-1105.
- Lee SK, Bae KW, Choy WS (2013) Use of the radial groove view intra-operatively to prevent damage to the extensor pollicis longus tendon by protruding screws during volar plating of a distal radial fracture.Bone Joint J 95: 1372-1376.
- Tweet ML, Calfee RP, Stern PJ (2010) Rotational fluoroscopy assists in detection of intra-articular screw penetration during volar plating of the distal radius. J Hand Surg Am Apr 35: 619-627.
- Langerhuizen DWG, Bergsma M, Selles CA (2020) Diagnosis of dorsal screw penetration after volar plating of a distal radial fracture. Bone Joint J 102: 874-880.