Publication Information
ISSN: 2641-693X
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Reactivation of Endocarditis with Commitment of the Fibrosis Skeleton
Rios William1, Rios Giovanny2*
1Cirujano Cardiovascular Pontificia Universidad Javeriana, Hospital de San José, Colombia
2Cirujano Cardiovascular Hospital San Ignacio- Hospital San José, Profesor Asistente Pontificia Universidad Javeriana, Colombia
Received Date: October 05, 2019; Accepted Date: November 04, 2019; Published Date: November 13, 2019
*Corresponding author: Rios Giovanny, Cirujano Cardiovascular Hospital San Ignacio- Hospital San José, Profesor Asistente Pontificia Universidad Javeriana, Colombia. Email: edgar.rios@javeriana.edu.co
Citation: William R, Giovanny R (2019) Reactivation of Endocarditis with Commitment of the Fibrosis Skeleton. Int Jr Cardiac Sci and Res: IJCSAR-113.
Summary
Introduction: the fibrous skeleton endocarditis is a frequent complication of infective endocarditis. Its incidence varies depending on the series between 25 and 39% and doubles in prosthetic valve endocarditis. It is considered that mortality is 30% with conventional surgical management and recurrence of infection of 9.5%. Case: patient 40 years old who was admitted because of Table 3 months of occasional fever, night sweats, chest pain and weight loss; valuation is performed and positive cultures for gram positive cocci evidence. With echocardiogram report vegetated anterior leaflet of the mitral valve and aortic valve vegetation and severe mitral regurgitation. Antibiotic therapy is initiated with posterior mitral valve replacement and aortic mechanical. On the first postoperative month presents vegetation accompanied by severe mitral regurgitation again. Antibiotic therapy is initiated, and progression of failure, mitral valve eviction takes new mechanical mitral valve replacement and reconstruction of the ring. Postoperative control of the second valve replacement is asymptomatic. Conclusion: This is an important event for the revival of the fibrous skeleton endocarditis in the first month after surgery, which required a second change, more reconstruction of the mitral ring, adequate evolution.
Keywords: Cardiovascular Surgery; Endocarditis, Fibrous Skeleton, Valvular Heart Disease
Introduction
Endocarditis of the fibrous skeleton is a frequent complication in infective endocarditis. Infective endocarditis is an inflammatory pathology of the parietal and / or valvular endocardium secondary to infectious phenomena, which can have serious consequences for the individual. It is characterized by the presence of vegetations composed of platelets, fibrin, microorganisms and inflammatory cells. Its incidence varies according to the series between 25 and 39% and is doubled in endocarditis on prostheses. It is considered that mortality is 30% with conventional surgical management and with a recurrence of infection of 9.5%. [1, 3, 5].
We present the following case report of endocarditis of the fibrous skeleton in a native valve, and later in a prosthetic valve of the same patient. Case Report this is a 40-year-old patient who consulted the cardiology department of Hospital San Ignacio in February 2014 for presenting a 3-month history of occasional fever, nocturnal diaphoresis, non-angina chest pain and weight loss. He studied with a focus on dental caries. Denies some important antecedent. On admission physical examination, the patient presented systolic aortic murmur and mitral systolic murmur.
Hemogram with leukocytosis and neutrophilia, report of positive blood cultures for streptococcus viridans. A transesophageal echocardiogram is taken where vegetation of 2cm x 0.8 cm is evident in the anterior leaflet of the mitral valve; with perforation of the anterior leaflet and possible abscess. It presents severe insufficiency of the same one. Bivalve aortic valve with 0.4 cm vegetations in one of the valves with severe aortic insufficiency. LVEF: 50%. Without other alterations (Figure 1).
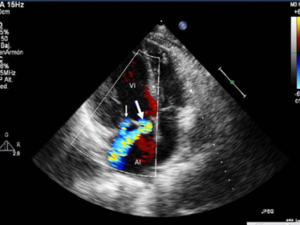
Figure 1: Mitral valve vegetation associated with severe insufficiency is evidenced.
In view of the different findings, aortic and mitral valvular changes were carried out 15 days after the start of the antibiotic scheme. After this the patient presents adequate evolution and output. Consult again the emergency cardiology service for presenting respiratory distress, fever associated with retrosternal pain. The antibiotic scheme is started and paraclinics are taken, in which there is marked evidence of leukocytosis and neutrophilia; Transesophageal echocardiogram report showing vegetation in the ring and severe mechanical mitral valve insufficiency. It is again brought to mechanical mitral valvular exchange, where it is necessary to manage the adhesions and recent inflammatory process (Figure 2).
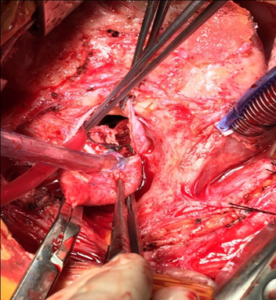
Figure 2: Inflammation and thrombus findings in valves.
In cavity, a completely dislodged mitral valve was found, with adhesion to the ring only in the posterior part. The anterior part shows vegetation, abscess of the ring. (Figure 3 and 4) Resection, drainage, debridement and reconstruction of the ring with a pericardial patch sutured in two planes is made, and this neoanillo is made fixation of new prosthesis. It is left packed by coagulopathy and subsequent closure.
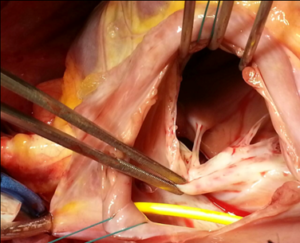
Figure3: Resection of the mitral valve.
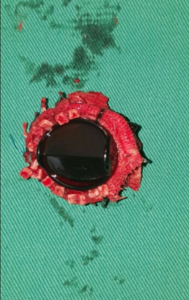
Figure 4: Detachment of the mechanical prosthesis.
It models the inflammatory response, tolerates weaning of supports and is discharged with oral anticoagulation. The patient is assessed at the postoperative month with a transesophageal echocardiogram report, which adequately performs valvular prostheses and LVEF: 50%. Pathology report evidence presence of vegetations with abundant inflammatory infiltrate (Figure 5).
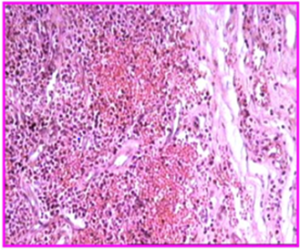
Figure 5: Histopathological study with a large increase in polymorphonuclear cells and fibroblasts.
Discussion
Infective endocarditis presents vegetations composed of platelets, fibrin, microorganisms and inflammatory cells, in other cases there is a thrombotic endocarditis [1, 3, 5]; this type of pathology occurs more in the male sex compared to the opposite sex, with some variations with respect to age being previously a pathology of adult patients now more cases occur in young patients [2, 4, 6]. Some of the predisposing factors (prosthetic valves, degenerative sclerosis of a valve, intravenous drug abuse) and invasive procedures with risk of bacteremia. The left heart valves have a greater incidence of said pathology due to the higher pressure that these valves must support [1, 2].
In our case, it was a patient with infectious endocarditis on the native valve, with no clear initial cause of the pathology, apparently with only focus on dental caries, with an initial echocardiogram report showing a mitral valve vegetation associated with severe insufficiency; Severe mitral regurgitation occurs more frequently in men older than 50 years. The patient-related microbiology in the initial blood cultures was positive for S. viridans, it is frequent in patients with underlying valve disease (in 62-90% of the patients a pre-existing cardiovascular disorder is described) [1-4]. One of the major complications is septic embolism, which did not occur in our case and this only occurs in a third of patients. The echocardiogram reported these detectable vegetations in 64% of the cases [1]. Current antibiotic recommendations include penicillin G, ceftriaxone or vancomycin for six weeks, combined with an aminglocoside for at least the first two weeks.
The antibiotic prophylaxis of endocarditis is not indicated in all cases; only prophylaxis in patients with prosthetic valves or some congenital heart disease [1, 4, 5]. Initial antibiotic treatment and subsequent surgical management were given. Surgical treatment during the active phase of endocarditis presents a higher risk of complications such as damage to the cardiac structure, so it is decided to perform after antibiotic management depending on the case and the surveillance of it. Infective endocarditis is ideal surgical treatment after the end of antibiotic management; looking for that the valvular tissue and bordering to it is free of the infection in its majority, this occurs for the native valves and in the cases of valvular prosthesis it is ideal to take the patient to surgery in the smaller possible time [1-4]. There is a higher mortality in the studies carried out; in patients who are taken to surgical management in the active phase of the disease, in comparison with those that are worn when the infection is controlled [2]. In our case, there were no embolisms, which are frequent and is one of the indications for surgical management. This type of embolism occurs in 20 to 25% of cases and more frequently to the brain and spleen [3, 4].
Urgent surgical management should be done as prevention of embolisms or vegetations with high potential to cause embolisms; such as vegetations greater than 10 mm or that have presented one or more embolic episodes despite strict antibiotic use for said pathology, cases in which the evolution of the pathology causes (heart failure, persistent infection, abscess), or because they had Very large isolated vegetations (> 15 mm) [1, 3, 5]. In the prosthetic valves we can find a classification given by time; in early (within 2 months of surgery) and late after two months after surgery. There are other series that show a lapse of up to 12 months. One must have a high suspicion of persistence of the disease given by embolic events in its majority to organs such as brain; in which the patient is following the surgical procedure with cerebrovascular events. One of the most important cases is splenic embolism, which was suspected in our case and a scan was taken with marked leukocytes, which was negative. The persistence of splenic plantings is mostly seen; associated with the reactivation of endocarditis and especially endocarditis of the fibrous skeleton [1, 2, 5, 6].
It is a serious disease, with high mortality which can be between 20 and 30% in expert hands and with a complex hospital infrastructure. Its prognosis depends on several factors, among which we have the valvular type are the left valves in comparison with the right valves, if it is one or multiple. The type of germ and virulence (S. aureus, Gram negative, fungi); nosocomial infections have a higher mortality. conclusion It is a complex pathology with an important incidence in our environment; that presents an increase given by the multiple diseases and the consumption of intravenous substances. Which is an important challenge for the surgeon and his interdisciplinary team, both medical and surgical management. In our case, it is a reactivation of the same with a proper and timely medical and surgical management. The high mortality must be taken into account both in a first surgical intervention and with greater reason and elevation of it in a second intervention; with the favorable results that were had in said patient.
References
- Arnettn EN, Roberts WC (1976) Valve ring abscess in active infective endocarditis. Frequency, location and clues to clinical diagnosis from the study of 95 necropsy patients. Circulation 54: 140-145.
- Casabe J. Oracio (2008) Infectious endocarditis, a changing disease, cardiology and cardiovascular surgery institute, favaloro foundation, buenos aires 68: 164-174.
- David TE, Kuo J, Armstrong S (1997) Aortic and mitral valve replacement with reconstruction of the intervalvular fibrous body. J Thorac Cardiovasc Surg 114: 766-771; discussion 771-772.
- De Oliveira NC, David TE, Amstrong S, Ivanov J (2005) Aortic and mitral valve replacement with reconstruction of the intervalvular fibrous body: an analysis of clinical outcomes. J Thorac Cardiovasc Surg 129: 286 -290.
- Moreillon P, Que Y-A (2004) Infective endocarditis. Lancet 363: 139-149.
- Mylonakis E, Calderwood SB (2001) Infective endocarditis in adults, N Engl J Med 345: 1318-1330.