Publication Information
ISSN 2691-8803
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2019
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Preliminary Outcomes of Multimodal Conservative Therapy in Lipedema
Lorenzo Ricolfi1* and Laura Patton2
1Department of Medical Biotechnology – University of Siena, Italy
2Medical clinic of endocrinology – Trento, Italy
Received Date: June 22, 2023; Accepted Date: June 28, 2023; Published Date: July 07, 2023;
*Corresponding author: Lorenzo Ricolfi, Department of Medical Biotechnology, University of Siena, Italy. Email: lorenzoricolfi@hotmail.it
Citation: Ricolfi1 L, Patton L. (2023) Preliminary Outcomes of Multimodal Conservative Therapy in Lipedema. . Adv Pub Health Com Trop Med: APCTM-181.
DOI: 10.37722/APHCTM.2023204
The term “lipedema” identifies a pathology defined for the first time by Allen and Hines in 1940 and characterized by an increase in subcutaneous adipose tissue associated with transient edema aggravated by prolonged standing, especially in the summer season [1]. Lipedema is a chronic pathology that is little known and difficult to diagnose, typically affects the female sex, can potentially be in any part of the body, but more frequently involves the lower limbs; often confused with lymphoedema, lipodystrophy, or obesity [2]. The true prevalence of lipedema is not known, although it is thought to be a common disease. Prevalence estimates range from 6.5% in children in the United States, 6%–8% in women in Germany, 15%–19% in vascular disease clinics. If these numbers hold true, applied to the US population, millions of women in the US would be affected [3]. It is an inflammatory and fibrotic disease of the loose connective tissue (of which adipose tissue is a part) that generally spares the trunk and does not affect the hands and feet. From this preferential anatomical distribution derives a typical disproportion between the extremities and the trunk, due to a localized and symmetrical increase in the subcutaneous adipose tissue at the level of the lower and/or upper limbs [4].
The treatment must be customized to the specific clinical needs of the patient and must be set after a careful clinical lymphological and endocrine-metabolic evaluation and in selected cases after a vascular and surgical evaluation. Conservative treatment is based on a multidisciplinary approach that includes multimodal decongestive therapy and the use of compression garments, in association with specific nutritional and physical activity regimes. In selected cases, especially in cases not responsive to adequate conservative treatment, a surgical approach is required.
There is still no complete agreement on the diagnostic criteria useful for the purposes of diagnosis proposed by the various guidelines and international consensus documents. The confusion is even more evident for therapeutic proposals, as there are currently no defined and differentiated protocols not only based on staging but also based on the phenotypic expression of the disease in the individual patient.
Decongestive treatment, despite being defined as the key treatment of the disease, does not yet have a clear indication in the therapeutic path in the absence of clinical signs of manifest edema. However, we have reason to think that the usefulness of this treatment goes far beyond the simple reduction of edema and or tissue congestion in the areas of the body affected by lipedema and that its usefulness needs to be redefined by structuring therapeutic protocols that take into consideration the timing of the therapy, the intervals and the number of treatment needed and the combination with the other therapeutic approaches, such as specifically, nutrition and physical activity. All these aspects must be taken into consideration, in our opinion, if we want to act effectively on the characteristic signs and symptoms of the disease, but in particular on pain and discomfort.
In our case series, which includes a population of women with lower limb lipedema of over 200 patients, in 95.4% of cases, at least one of the specific symptoms of lipedema were reported by the patients such as spontaneous pain (77% of cases), sensation of heaviness, swelling and fatigue in the absence of pain in the remaining cases. In most cases, these symptoms worsen during the day, following physical activity, especially if of high intensity but also in situations of prolonged time in a sitting position or prolonged time in standing position, during the luteal phase of the menstrual cycle and, in general, with the warm season. Only in 10% of cases, the symptoms are not affected by the factors just described, while a part of the patients instead reports an improvement in symptoms with physical activity. Bruising due to minimal trauma or spontaneously was reported in over 80 % of cases and the prevalence of the symptom increases with the clinical stage.
The most frequent clinical sign in our population was pain on pinching the skin of the affected limbs that is present in 99% of cases:
Among other clinical signs found with greater frequency we have subcutaneous nodules (98%), supra-patellar fat pads (95%) and the presence of the dimple in the medial retromalleolar region (89%) (Figure 1.).
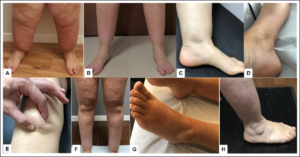
Figure 1: Clinical signs in lipedema. The figure shows some of the characteristic clinical signs of lipedema: ankle cuff. (A and B), malleolar dimple (C and D), supra-patellar fat pad (E and F), malleolar fat pad (H and I).
The prevalence of the presence of pain on pinching the skin in the lower extremities did not differ between stages.
In our opinion, this clinical sign is fundamental, not only for the diagnosis and definition of the clinical severity, but also because, if measurable, it could be used in the follow-up of the patient over time and as indicators of the various treatments and in addition to the indices anthropometrics, volumetrics and ultrasound evaluation of tissues.
In our group, the presence of pain on pinching the skin is performed in a systematic and methodical manner at the moment of the diagnosis and at each follow-up visit. The presence of pain on pinching the skin is evaluated in different points of the lower limb, upper limb, abdominal and back and we use the Verbal Rating Scale (VRS) for evaluating the intensity of pain.
We report the preliminary outcomes of multimodal conservative therapy in Lipedema using this sign as a parameter of efficacy of the therapy. During the study we also evaluated the modification of other parameters, such as subjective symptoms, the volume of the limbs, the thickness of the subcutaneous tissue measured by ultrasound, which will be published later. The variation of all these parameters considered to evaluate the response to the different treatments is specific and not always harmonious or comparable, suggesting a different therapeutic mechanism of action, which could be usefully used according to the phenotype, the clinical stage, the specific needs and the goals of each individual patient.
Below we report the specific data relating to the variation of pain intensity when pinching the skin in 7 points of the lower limbs evaluated with the VRS scale individually and as a total score (sum of the scores in the individual points) in 39 patients to various conservative treatments:
- only diet
- only bandages
- physical activity with compression stocking (not daily) and diet
- bandages and diet (intensive sessions and half sessions)
- daily physical exercise with compression stocking
The most effective treatment in terms of reducing of pain was the association of DAILY specific compression stocking with physical activity and the association of bandages with diet (intensive session), which resulted in a reduction in the pain score of 80% and 70% , respectively. A 65% reduction was also obtained in the group treated with the combination of NOT DAILY physical exercise with stocking compression and diet.
Significantly lower results were instead found in the groups of patients who were treated selectively with the bandage and selectively with diet alone or in patients evaluated after half of the intensive bandaging cycle in association with diet (Figure 2).
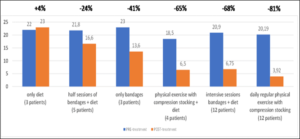
Figure 2: Effect of different treatments on pain. The figure shows the reduction of the total pain score evaluated with VRS in 7 points (total score 0-28) of the lower limb in relation to the different treatments. Total score before and after treatment and % change in score are shown.
The reduction of the lipoalgia score obtained with the bandage alone was approximately 20%, while it was not obtained with diet alone, although the subjective symptoms and anthropometric parameters improved in both groups.
In conclusion, the conservative treatment of the patient affected by lipedema still plays a fundamental role and is effective in terms of reduction of subjective symptoms and pain caused by pinching the skin fold, parameters of no small importance if considered in the patient’s daily life.
The pathophysiological mechanism underlying the pain remains to be clarified, although the study of the response to the different treatments could be helpful and very interesting for this purpose. However, from these data, it became clear the need for a multidisciplinary approach, fundamental for effective treatment, which otherwise could lead to little or no benefit and be incorrectly considered ineffective.
Furthermore, in our opinion, this is a sufficient reason to try to define different therapeutic pathways which must consider not only the presence or absence of clinical signs of edema, but also the presence of other specific symptoms as or clinical signs such as this, the presence of other comorbidities such as vascular and endocrine-metabolic which can aggravate the disease.
This type of approach is essential for studying the patient in toto to obtain a better definition of the clinical picture as complete as possible and then formalize a suitable therapeutic-assistance path inherent in the patient’s global “status” of health, thus not swelling only or the loco-regional aspect of the pathology.
References
- Allen EV, Hines EA (1940) Lipoedema of the legs: A syndrome characterized by fat legs and orthostatic oedema. Staff Meetings of the Mayo Clinic 15:184-187.
- Alcolea JM, Alonso AB, Arroyo BA, et al. Consensus document on lipedema 2018. Includes current status of Lipedema 2019. April 2018 / Update september 2019. Barcelona: LITOGAMA SL.
- Herbst KL, Kahn LA, Iker E, et al. (2021) Standard of care for lipedema in the United States. Phlebology. 36:779-796.
- Reich- Schupke S, Schmeller W, Brauer WJ, et al. (2017) S1 guidelines: Lipoedema. J Dtsch Dermatol Ges 15:758-767.