Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Persistent Symptomatic and Functional Improvement of Hands Osteoarthritis Post-Autologous Expanded Mesenchymal Stem Therapy: Case Report
Hassan Mubark*
Rheumatologist, Institution: Auckland Regenerative Clinic, Ormiston Specialist Centre, 125 Ormiston Road Flat Bush, Auckland 2019, New Zealand
Received Date: October 29, 2021; Accepted Date: October 31, 2021; Published Date: November 03, 2021
*Corresponding author: Hassan Mubark, Rheumatologist, Institution: Auckland Regenerative Clinic, Ormiston Specialist Centre, 125 Ormiston Road, Flat Bush, Auckland 2019, New Zealand. Tel: +64 9 2713305/+64 21843513; Fax: +64 9 2770769; Email: drhassanmubark@gmail.com
Citation: Mubark H (2021) Persistent Symptomatic and Functional Improvement of Hands Osteoarthritis Post-Autologous Expanded Mesenchymal Stem Therapy: Case Report. Adv Ortho and Sprts Med: AOASM-154.
DOI: 10.37722/AOASM.2021502
Abstract
Osteoarthritis of the hands is a challenging condition and difficult to treat. Current management included analgesic and anti-inflammatory medicines with hand exercises. In severe cases, joint replacement of the proximal interphalangeal joints and joint fusion surgery for distal phalangeal joints. We report a case of a sixty-six-year-old female who was bothered by symptomatic hand osteoarthritis for six years that affected her activities of daily living and work, her job as an aromatherapist. She responded well to fat-derived autologous expanded mesenchymal stem cell therapy, which we performed under ultrasound guidance after trans-thecal digital nerve block for bilateral second through fifth distal interphalangeal joints. The improvement started one month following the stem cell implants, with maximum benefit occurring ten months after the therapy, which endured afterward. A follow-up x-ray fourteen months post-treatment revealed no radiological progression of the treated joints compared to the baseline x-ray. Despite the persistent response, she elected a booster dose of stem cell therapy to maintain her function and prevent osteoarthritis progression. This case represents pleasant symptomatic and functional outcomes with no further deterioration of x-rays following expanded mesenchymal treatment for bilateral interphalangeal hands osteoarthritis.
Keywords: Hand Osteoarthritis, Mesenchymal Stem Cell, Radiologic Progression, Ultrasound-Guided
Introduction
The hand is one of the places highly commonly involved by osteoarthritis (OA), described by pain, stiffness, reduced hand strength, and skeletal deformities of hand joints, namely trapeziometacarpal joint, proximal interphalangeal (PIP), and distal phalangeal (DIP) joints [1,2]. As OA progresses, it affects routine daily activities, work, and quality of life [3]. Dissimilar to the general belief that it is a disorder of older individuals, hand OA can occur reasonably early in life, especially in middle-aged people, and impair individuals' work capacity [4]. The standard practice in managing hand OA is a combination of non-medical and medical interventions but those measures with limited and short-lived benefit. Medical therapy includes local and systemic non-steroidal anti-inflammatory drugs (NSAIDs). The latter could carry the risk of gastrointestinal irritation, bleeding, and renal damage, particularly if the patient has comorbidities like diabetes, hypertension, or taking medications that interact with NSAIDs. Other medical therapies have been tried, including acetaminophen, glucosamine and chondroitin, intra-articular steroid, and hyaluronic acid injections with limited successes [5, 6, 7, 8]. The surgical option is considered a last resort with arthroplasties for PIP joints and arthrodesis in DIP joints [9].
Our case demonstrates a persistent dramatic response to the implantation of autologous expanded mesenchymal stem cells into bilateral multiple DIP joints; her post-treatment x-ray showed stability with no progression of the treated DIP joints.
Case Report
A sixty-six-year-old aromatherapist, she is usually fit and healthy who works around thirty hours a week. She presented with six years of symptoms of increasing bilateral pain in her second-fifth DIP joints, particularly in cold weather. She had significant stiffness with impairment in activities of daily living, notably gardening, cutting things, and opening jars. She struggled to do her job in aromatherapy. In January 2020, she had an x-ray of her hands which revealed severe osteoarthritis right third DIP joint with narrowing and osteophyte formation. Moderate osteoarthritis at the bilateral fourth and fifth DIPs, as in (Figure1). She elected experimental mesenchymal stem cell (MSC) therapy; in June 2020, she had the abdominal fat harvesting then was sent to a specialized lab for cell expansion. In August 2020, she underwent MSC implantations. We did the procedures using multiple bilateral trans-thecal digital nerve blocks, as in (Figure2). We implanted 10 million MSCs in each of the eight DIP joints using a 0.4MLS solution under ultrasound guidance using a hockey stick probe with a sonosite ultrasound transverse approach, as in (Figure3). One-month post-MSC injections, she felt some improvement in pain and stiffness that peaked after ten months of the therapy. That positive effect has continued; she reported good social and work functional abilities. A repeat x-ray in October 2021 revealed no progression of OA, as in, as in (Figure4). We compare the current x-ray to her baseline x-ray, twenty-one months prior. In October 2021, she decided on booster MSC injections to further protect her joints, and we adapted the same protocol as the first one.

Figure1: pre-treatment X-ray hands demonstrating established osteoarthritis in multiple joints.

Figure2: Long axis ultrasound-guided needle for trans-thecal digital nerve block.
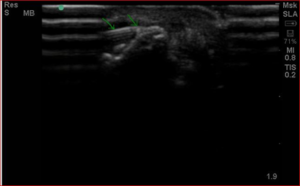
Figure3: Short axis ultrasound-guided needle in distal interphalangeal joint.

Figure4: post-treatment X-ray hands demonstrating No progression of osteoarthritis.
Discussion
There is no proven therapy for hand OA, particularly for DIP joints, with arthrodesis the only option while PIP joints can be replaced [9]. In comparison, various non-pharmacologic and pharmacologic therapy do not seem to alter the outcome of the hand's function in addition to the gastrointestinal and renal complications of the long-term use of NSAIDs. Fusion of DIP joints means a significant limitation of fine finger movements, which leads to impairment of daily living activities. It could also lead to job loss, like our patient, who could continue her loved work following MSC therapy.
MSC therapy is a promising science and rapidly progressing. However, it does not cure finger osteoarthritis or reverse the severely damaged cartilage. Still, we believe it is the best available experimental option and counted as a safe option, shown in clinical trials [10].
Our therapy, in this case, suggests a possible good potential and safe alternative medicine in patients who elect to try it.
Conclusion
We hypothesize that autologous expanded MSC therapy has significantly improved daily functional activities and returned to work with no further radiologic progression. We believe booster doses can be implemented safely and would help maintain the hand's function. However, we need to confirm those findings are consistent in comprehensive randomized controlled trials.
References
- Zhang W, Doherty M, Leeb BF, Alekseeva L, Arden NK, et al. (2009) EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Ann Rheum Dis. 68:8-17.
- Zhang Y, Niu J, Kelly-Hayes M, Chaisson CE, Aliabadi P, et al. (2002) Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly: The Framingham Study. Am J Epidemiol. 156:1021-7.
- Michon M, Maheu E, Berenbaum F (2011) Assessing health-related quality of life in hand osteoarthritis: a literature review. Ann Rheum Dis. 70:921-8.
- Kloppenburg M, Stamm T, Watt I, Kainberger F, Cawston TE, et al. (2007) Research in hand osteoarthritis: time for reappraisal and demand for new strategies. An opinion paper. Ann Rheum Dis. 66:1157-61.
- Bannuru RR, Schmid CH, Kent DM, Vaysbrot EE, Wong JB, et al. (2015) Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 162:46-54.
- Gabay C, Medinger-Sadowski C, Gascon D, Kolo F, Finckh A (2011) Symptomatic effects of chondroitin 4 and chondroitin 6 sulfate on hand osteoarthritis: a randomized, double-blind, placebo-controlled clinical trial at a single center. Arthritis Rheum. 63:3383-91.
- Bannuru RR, McAlindon TE, Sullivan MC, Wong JB, Kent DM, et al. (2015) Effectiveness and Implications of Alternative Placebo Treatments: A Systematic Review and Network Meta-analysis of Osteoarthritis Trials. Ann Intern Med. 163:365-72.
- Kroon FP, Rubio R, Schoones JW, Kloppenburg M (2016) Intra-Articular Therapies in the Treatment of Hand Osteoarthritis: A Systematic Literature Review. Drugs Aging. 33:119-33.
- Rongières M (2013) Surgical treatment of degenerative osteoarthritis of the fingers. Chir Main. 32:193-8.
- Centeno CJ, Al-Sayegh H, Freeman MD, et al. (2016) A multi-center analysis of adverse events among two thousand, three hundred and seventy-two adult patients undergoing adult autologous stem cell therapy for orthopaedic conditions. Int Orthop 40:1755-1765.