Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Periosteal Sleeve and Cartilage “Clew” Injury Secondary to SCFE Related CAM Type Deformity
Jaime Hinzpeter*, Alvaro Zamorano, Cristian Barrientos, Maximiliano Barahona, Guillermo Robles
Orthopedic Department at Hospital Clinico Universidad de Chile, 999 Santos Dumont Street, Independencia, Santiago 8380456, Chile
Received Date: January 24, 2020; Accepted Date: February 04, 2020; Published Date: February 12, 2020
*Corresponding author: Jaime Hinzpeter, Orthopedic Department at Hospital Clinico Universidad de Chile, 999 Santos Dumont Street, Independencia, Santiago 8380456, Chile. Email: jhinzpeter@hcuch.cl
Citation: Hinzpeter J, Zamorano A, Barrientos C, Barahona M, Robles G (2020) Periosteal Sleeve and Cartilage “Clew” Injury Secondary to SCFE Related CAM Type Deformity. Arthroscopic Finding and Pathogenesis Approximation. Adv Ortho and Sprts Med: AOASM-118.
Abstract
This case attempts to propose the pathophysiological mechanism in the relationship between SCFE (slipped capital femoralepiphilosolysis) and FAI (femoroacetabular impingement), and also establish a pathophysiological way between the slipped capital femoral epiphysiolysis and the femoroacetabular impingement, at the beginning of the series of events that lead to joint damage.
The authors present the case of a female patient (16 years old), who has a femoroacetabular impingement, in the context of a slipped capital femoral epiphysiolysis.
We have observed an atypical behavior of the chondral lesion, with the formation of a kind of cartilaginous clew, which causes an alteration of contact (friction) with the consequent chondral damage, so we postulate that it is relevance the relationship between SCFE (slipped capital femoral epiphysiolysis) and FAI (femoroacetabular impingement) is known, in terms of the formation of a CAM-like defect. This series of events leads to osteoarthritis in young patients. We uphold a possible origin in this chain of events; for example, we describe an initial lesion, a cartilaginous clew, with its consequent development and possible cause of joint damage, finally, in conclusion, we confirm that the formation of this kind of clew can be the pathophysiological beginning of the relationship between the SCFE (slipped capital femoral epiphysiolysis) and the FAI (femoroacetabular impingement), which aims to make an early and timely diagnosis.
Keywords: Clew; FAI (Femoroacetabular impingement); SCFE (Slipped Capital femoral Epiphilosolysis)
Introduction
There is a relationship between slipped capital femoral epiphilosolysis, (SCFE) and femoroacetabular impingement syndrome (FAI) [7, 3, 17]. The sequela of slipped capital femoral epiphysiolysis is a deformity at the level of the femoral neck-head union, which is prominent, especially in the lateral region of the femur. Over time, this will produce a CAM type of damage on the acetabular joint surface; that is to say, rupture at the level of the chondrolabral junction will eventually trigger a degenerative process producing early osteoarthritis [4, 5, 12, 20].
SCFE (slipped capital femoral epiphysiolysis) is a pathology of the adolescent's hip, with an incidence of 11 out of every 100,000 adolescents [13]. It corresponds to sliding of the hypertrophic layer of the articular cartilage line, which causes a displacement of the femur in relation to the head, towards anterior and superior. Consequently, in about 90% of cases there is a decrease in external rotation [9]. And the cervicodiaphyseal angle (varusdeviation). The pathophysiology is not yet clear; however, mechanical factors such as vertical articular cartilage line and obesity are associated since they increase the increase the shears forces on the articular cartilage line, and hormonal factors, such as alterations in the secretion of growth hormone and sex hormones. There are 2 large presentations, stable, corresponding to the patient with epiphysiolysis that can bear load at the time of consultation, and unstable when a patient cannot walk. However, there is a considerable percentage, approximately 3 - 10% of patients, with silent or asymptomatic SCFE (slipped capital femoral epiphysiolysis), who seek consultation years later due to the deformity that consequently remains13. The bump type SCFE (slipped capital femoral epiphysiolysis) deformity has been found in 17 to 24% of the male population and in 4% in the female [6, 21].
Here is a particular case of a female adolescent with slipped capital femoral epiphilosolysissequel, who presents femoroacetabular impingement. In addition to the acetabularchondral damage, an atypical injury in the articular cartilage of the femoral head is observed, which we call a ball injury due to its macroscopic characteristics.
Clinical Case
A 16-year-old female patient who consulted due to bilateral coxalgia, more significant on the right hand side, with approximately one year of evolution, associated with limited joint range and no claudication.
Physical examination presents pain in the right inguinal area ++. Right internal rotation of 0º, external rotation of 25º and abduction of 0º is observed during active and passive mobilization see (Table 1).
Study with Images
AP pelvis X-ray + axial hip: bilateral sequela of epiphysiolysis with an extensive bilateral bump in the anterolateral region is observed, with positive “pistol grip” sign associated, a decrease in joint space can be seen concordant with Tonnis 211. The AP X-rays of both hips are shown in (Figures 1 and 2).
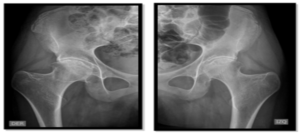 (1) & (2)
(1) & (2)
Figure 1: Anterior antero X-ray of right hip.
Figure 2: Anterior antero X-ray of left hip.
Nuclear Magnetic Resonance (NMR): presents coxo femoral arthrosis and joint effusion. Severe thinning of the cartilage is observed predominantly in the upper portion of the joint, with areas of subchondral bone exposure.
Extensive rupture of the superior and anterior disinsertion labrum, evidencing foci of in the superior anterior labrum. Bony prominence in the anterior area of the femoral neck and head union, secondary to degenerative bone proliferation (Figure 3) 93º alpha angle (Figure 4).
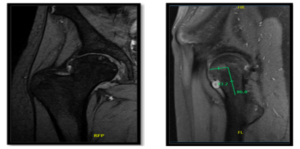
Figure 3 and 4: Coronal section of the right hip in T2. Deformity of the femoral head is observed.
Sagittal section of the right hip. Alpha angle measurement is seen.
Due to the aforementioned, an arthroscopy of the right hip was performed since the joint was causing significant pain for the patient. In the diagnostic arthroscopy, acetabular cartilage with a Type 3 [11]. ALAD injury in the anterolateral area is observed. The labrum is uninserted between 11:00 and 12:00. In the load zone of the femur, an extensive Grade 4 chondral injury is observed in the anterolateral region, and of the chondrolabral union, the cartilaginous tissue is folded in on itself, emulating a ball. It is impressive to observe how a full-thickness cartilaginous injury, completely detached from the subchondral bone, gradually coiled due to the movement of the hip until it reached such a volume that it blocked the joint (Figure 5).
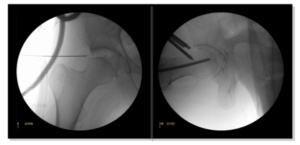
Figure 5: Arthroscopy of the right hip. A ball injury of the articular cartilage is observed.
A capsulotomy in "T" was performed, Acetabuloplasty between 10:00 and 1:00, according to time classification for hip. Reinsertion of labrum with two 2.3 bioraptor anchors (Smith & Nephew®).Resection of femoral ball injury. Femoral neck-head fixation with cephalomedullary screw of 6.5mm x 100mm to avoid risk of fracture and then extensive femoral osteochondroplasty from medial to lateral prior visualization of lateral retinaculum (Figure 6). At the end of the surgery, impingement tests were performed, which were negative. A capsulorrhaphy was not performed due to the degree of osteoarthritis found.
At control, 12 months after the surgical procedure on her right hip, the patient reported that in general she had not presented any pain, unlike in her contralateral hip.

Figure 6: Intraoperative fluoroscopy. A. Deformity of the femoral head is observed. B. Posterior femoral head to osteosynthesis of epiphysis fixation and posterior form to osteoplasty.
However, no significant improvement in joint range is observed. Harris Hip function test, 1 year post surgery, scores 89 points. It emphasizes the presence of pain during maximum degrees of flexion, which means there is discomfort when performing daily activities such as putting on socks. The patient states that most discomfort is caused by pain in the contralateral hip (Table 1).
Right hip before surgery
Right hip 1 year after surgery
Left hip
External Rotation
30°
30º
30º
Internal Rotation
0°
0º
0º
Flexion
90°
90º
90º
Extension
30°
30º
30º
Abduction
0°
10º
20º
Aduction
45°
45º
45º
Discussion
The acetabulofemoral impingement affects a significant number of people, causing symptoms as frequent as: inguinal pain, claudication and decreased activity. The diagnosis is based on the clinic and the test results (radiology and NMR (nuclear magnetic resonance).
There is a clear relationship between SCFE (slipped capital femoral epiphysiolysis) and FAI (femoroacetabular impingement), as supported in the literature. It is established that the sequelae produced by epiphysiolysis determine chondral damage with the physiological characteristics described in the CAM type FAI.
This association should increase the pediatric traumatologists´ alarms so that they achieve an early diagnosis and an adequate reduction of the SCFE (slipped capital femoral epiphilosolysis). Greater survival of the hip joint surface can be offered to our patients and thus, better quality of life while decreasing the likelihood of an arthroplasty at an early age.
On the other hand, even when the diagnosis is made early on and the respective surgery is indicated, some displacements of the femoral head are not reducible, therefore, its fixation is done in situ, which subsequently develops a deformity type bump and its sequelae.
Concomitantly, the increase in obesity and the early onset of adolescence have probably increased the incidence of SCFE (slipped capital femoral epiphysiolysis), and therefore, the incidence of sequelae in the hips in the adolescent population [18]. In addition to the aforementioned, there is a percentage of patients that present bilateral SCFE (slipped capital femoral epiphysiolysis), as is the case of patients [9, 2, 8, 14]. Bilateral SCFE (slipped capital femoral epiphysiolysis) is presented in a synchronous or an asynchronous manner. The latter is a challenge for the traumatologist since in situ fixation is indicated in at-risk populations. The prevalence of bilateral slipped capital femoral epiphysiolysis varies from 7% to 25%19. However, CAM-type deformities in patients with SCFE (slipped capital femoral epiphysiolysis) followed up until adulthood have been reported in 41% to 80% [9, 1, 19, 16]. This background information should change how a supposed unilateral epiphysiolysis is approached.
Although the relationship between slipped capital femoral epiphilosolysis and femoroacetabular impingement is known, the particularity of the case is the early finding of an extensive injury at the femoral cartilage level. This injury is characterized by a total thickness detachment of an extensive area of articular cartilage of the femoral head, which has the appearance of a large flap of cartilage that folded in on itself, generating a "ball" of cartilage. Our hypothesis is that the sequel of SCFE (slipped capital femoral epiphilosolysis) was of such magnitude that the movements of abduction / flexion and internal rotation not only detached the articular cartilage of the acetabulum, but also initially produced a fracture at the level of the femoral cartilage. The perpetuation of the mechanical problem caused a detachment of the articular cartilage forming this flap that began to fold [15]. This is unusual for CAM-type impingements in that the chondral damage at the femoral level is degenerative and not mechanical. The extensive chondral damage, both acetabular and femoral, in a 16-year-old patient, should reopen the discussion of epiphysiolysis management and its prevention in such a way as to not only treat the disease itself, but also its consequences in order to perform effective joint preservation surgeries in a timely manner.
Conclusion
Slipped capital femoral epiphilosolysis is a pathology whose incidence is increasing, therefore the sequelae of this pathology is also expected to increase. Its usual presentation is CAM-type femoroacetabular impingement syndrome and osteoarthritis. The severity of the sequelae is of high impact, as is established in the case described in which the patient has advanced coxarthrosis in both hips. Better diagnosis and management of the pathology is required to avoid the need for arthroplasty at an early age.
Conflicts of Interest
- The corresponding author declare no conflicts of interest.
- We declare that we haven't finance source.
Author Contributions
- Robles, A. Zamorano, J. Hinzpeter: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work.
- Barahona and C. Barrientos, J. Hinzpeter: Drafting the work or revising it critically for important intellectual content.
- M Barahona, J. Hinzpeter: Final approval of the version to be published.
References
- Kent DM, Ruthazer R, Weimar C, Mas JL, Serena J, et al. (2013) An index to identify stroke-related vs
incidental patent foramen ovale in cryptogenic stroke. Neurology 81: 619-625. - Aronsson D, Loder R, Breur G, Weinstein S (2006) epiphysis: current concepts Slipped capital femoral. J Am AcadOrthopSurg 14: 666-679.
- Carney B, Weinstein S, Noble J (1991) Long-term follow-up of slipped capital femoral epiphysis. J Bone Joint Surg Am 73: 667-674.
- Fraitzl C, Käfer W, Nelitz M, Reichel H (2007) Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: a mean follow-up of 14.4 years after pinning in situ. J Bone Joint Surg (Br) 89: 1592–1596.
- Ganz R, Leunig M, Leunig-Ganz K, Harris W (2008) The etiology of osteoarthritis of the hip: an integrated mechanical concept. ClinOrthopRelat Res 466: 264-272.
- Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, eta al. (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. ClinOrthopRelat Res. 417: 112-120.
- Gosvig K, Jacobsen S,Palm H, Sonne-Holm S,Magnusson E (2007) A new radiological index for assessing asphericity of the femoral head in CAM impingement. J Bone Joint Surg 89: 1309-1316.
- Hosalkar H, Pandya N, Bomar J, Wenger D (2012) Hip impingement in slipped capital femoral epiphysis: a changing perspective. J Child Orthop 6: 161-172.
- Jensen H, Steinke M, Mikkelsen S, Thomsen P (1990) Hip physiolysis. Bilaterality in 62 cases followed for 20 years. ActaOrthopScand 61: 419-420.
- Jerre R, Billing L, Hansson G, KarlssonJ,Wallin J (1996) Bilaterality in slipped capital femoral epiphysis: importance of a reliable radiographic method. J PediatrOrthop B 5: 80-84.
- Koczewski P (2013) Valgus slipped capital femoral epiphysis: subcapital growth plate orientation analysis. J PediatrOrthop B 22: 548-552.
- Konan S, Rayan F, Meermans G, Witt J, Haddad FS (2011) Validation of the classification system for acetabularchondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br 93: 332-336.
- Lavigne M, Parvizi J, Beck M, Siebenrock K, Ganz R, et al. (2004) Anterior femoroacetabular impingement: Part I. Techniques of joint preserving surgery. ClinOrthopRelat Res 418: 61-66.
- Lehmann C, Arons R, Loder R, Vitale M (2006) The epidemiology os Slipped capital femoral epiphysis: An update. J PediatrOrthop 26: 286-290.
- Loder R, Aronson D, Greenfield M (1993) The epidemiology of bilateral slipped capital femoral epiphysis. A study of children in Michigan. J Bone Joint Surg Am 75: 1141-1147.
- Loder R, Richards B, Shapiro P, Reznick L, Aronson D (1993) Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am 75: 1134 -1140.
- Macía C, Sanchez I, Medina J (2016) Slipped capital femoral epiphysis in adults: case report and review of literature. Reumatismo 68: 40-47.
- Rab G (1999) The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J PediatrOrthop 19: 419-424.
- Siebenrock KA, Ferner F, Noble PC, Santore RF, Werlen S, et al. (2011) The CAM-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. ClinOrthop 469: 3229-3240.
- Schultz W, Weinstein J, Weinstein S, Smith B (2002) Prophylactic pinning of the contralateral hip in slipped capital femoral epiphysis: evaluation of long-term outcome for the contralateral hip with use of decision analysis. J Bone JointSurg Am 84: 1305-1314.
- Tannast M, Goricki D, Beck M, Murphy S, Siebenrock K (2008) Hip damage occurs at the zone of femoroacetabular impingement. ClinOrthopRelat Res 466: 273-280.
- Valera M, Ibañez N, Sancho R, Tey M (2016). Reliability of Tönnis classification in early hip arthritis: a useless reference for hip-preserving surgery. Archives of orthopaedic and trauma surgery 136: 27-33.