Publication Information
ISSN 2691-8803
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2019
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Nepal COVID-19 Disease Response Intervention Effectiveness on Wave 1 and Wave 2 based on Nepal’s Ministry of Health and Population Daily Situation Reports
King Daveric Lomotos, MPH1*, Sujan Babu Marahatta, MsC, PhD2, Faith Boucher, PhD3
1Department of Public Health Sciences, University of California, Davis, Davis, California
2Professor, Manmohan Memorial Institute Sciences, Kathmandu, Nepal
3Department of Public Health Sciences, University of California, Davis, Davis, California
Received Date: October 14, 2022; Accepted Date: October 21, 2022; Published Date: October 27, 2022;
*Corresponding author: King Daveric Lomotos. Department of Public Health Sciences, University of California, Davis, Davis, California. Email: kdlomotos@ucdavis.edu
Citation: Lomotos K D, Marahatta S B, Boucher F (2022) Nepal COVID-19 Disease Response Intervention Effectiveness on Wave 1 and Wave 2 based on Nepal’s Ministry of Health and Population daily situation reports. Adv Pub Health Com Trop Med: APCTM-167.
DOI: 10.37722/APHCTM.2022503
Abstract
Background
This study is to assess the effectiveness of Nepal’s COVID-19 disease response in the first wave and second wave (01/28/2020-06/28/21) by inspecting the trajectory of morbidity (cases) and mortality (deaths) peaks after the implementation of key COVID-19 interventions shown through constructing graphs utilizing Nepal’s COVID-19 daily situation reports.
Objectives
This study aims to highlight the notable mistakes of Nepal’s COVID-19 interventions and policies to provide possible recommendations through Covid-19 Nepal Preparedness and Response Plan in April 2021 to improve their disease response policies and interventions, preparing the country against future pandemics.
Methods
A retrospective analysis was conducted to investigate contextual information using scholarly and grey literature in Google Scholar to help understand what occurred in Nepal within and before the peaks.
Result
Although, Nepal’s disease response was effective and swift in the beginning months shown from the daily cases and mortalities were as high as 24 and 0 per day, respectively. However, that soon changed a year later when problems from existing policies and interventions arose as the pandemic continued with cases reaching as high as 8,173 per day and 5,410 mortalities per day.
Conclusion
The paper addresses the potential problems with existing policies and interventions by concluding with possible improvements to Nepal’s current COVID-19 2021 Disease Response Plan to mitigate mortality and morbidity in future endemics or pandemics Nepal may endure.
Keywords: First Wave; Interventions; Nepal Ministry of Health & Population of Nepal Daily Situation Reports; Second Wave
Background
During the beginning of the Pandemic, the first interventions were implemented at “Tribhuvan International Airport” screening for incoming passengers displaying COVID-19 symptoms. [1] Those suspected of COVID-19 were transported to “Sukraraj Infectious and Tropical Disease hospital in Kathmandu,” and quarantined until tested negative for COVID-19 using RT-PCR tests [2] conducted at the National Public Health Laboratory (NPHL) on January 27th, 2020. [1] However, the National Public Health Laboratory staff needed to be trained hands-on by WHO (World Health Organization) international experts. Thus, an expert from WHO developed 20 standard operating procedures for COVID-19 Testing in the country. As cases increased in March 2020, the testing capacity needed to increase but due to the limitations of laboratories, Polymerase Chain Reaction (PCR) technology could not be utilized, thus relying on Rapid Diagnostic Testing (RDT) kits. Furthermore, the Nepalese government created the “High-Level Multi Sectorial Coordination Committee for COVID-19” to organize a federal response for its citizens against COVID-19 and issued a lockdown to slow down the spread of the cases along with the utilization of the Information Education and Communication (IEC) to help spread information and awareness to mitigate the disease. [3] However, despite these early interventions, mortalities and cases still rose, thus this paper addresses the effectiveness of interventions.
Objectives
This study aims to highlight the notable mistakes reported from grey and scholarly articles on Nepal’s COVID-19 interventions and policies to provide possible recommendations in the Covid-19 Nepal Preparedness and Response Plan in April 2021 for further improving their disease response efforts and assisting the country against future pandemics.
Methodology
The paper conducted a retrospective analysis highlighting the important peaks of mortality(deaths) and morbidity(cases) for Wave 1 and Wave 2 in Nepal. Then, observing the within and before the time period of the peaks, interventions were noted by inspecting Nepal’s Daily Situation Reports. After, contextual information was obtained from grey and scholarly literature to help understand what occurred before and within the time period of the peaks to locate problems of the interventions. A time lag of 20 days is accounted for after the implementation of interventions and policies for effects to occur. Additionally, a time lag of 20 days is used for deaths to occur from cases. [4] Finally, Nepal’s current COVID-19 2021 Disease Response Plan was utilized for any recommendations or changes to improve or implement any intervention.
All data illustrations were formulated through R-Studio coding
Results
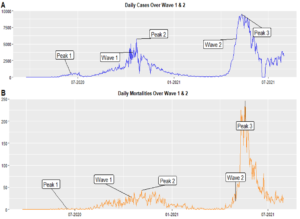
Figure 1: Highlighting Peaks of Daily Cases and Mortalities over Wave 1 and Wave 2.
Figure 2: Highlighting Intervention and Policies with Peaks (P1, P2, P3) of Total Cases and Mortalities over Wave 1 and Wave 2. RDTK(X) (6/6/20) Stopped Rapid Diagnostic Testing LK(X) (09/10/20) LK2 (04/29/21) Lockdown in Kathmandu ended 2nd Lockdown in Kathmandu VP2 (02/14/21) Vaccination Phase 2
Abbreviation (Date)
Intervention
What is it?
NL (3/24/2020)
National Lockdown
Stricter measurements in place restricting movements of citizens and told to stay home. [1]
ELC (3/29/20)
Expansion of Laboratory Capacity
COVID-19 PCR laboratory capacity was expanded from only the National Public Health Laboratory to 19 institutions in each province on May 11th, 2020, then 83 COVID-19 PCR laboratories a year later. [3]
RDTK (04/10/20-06/06/20)
Rapid Diagnostic Testing
RDT usage occurred which are rapid diagnostic testing kits instead of PCR for testing. There were many kits involved in finding positive cases and two main ones were used such as Rapid Diagnostic Testing and PCR technology [3]
LK (08/19/20)
Lockdown in Kathmandu
Lockdown in the capital of Kathmandu. [4]
VP1 (01/27/21)
Vaccination Phase 1
Vaccination phase 1 occurred where 1 million doses of AstraZeneca donated from India were utilized to vaccinate essential workers such as ambulance drivers, frontline personnel, and sanitation workers for. The second phase included government employees, banks, and journalists.5 After the vaccination phase, 2.62% of Nepalese were vaccinated. [6]
Abbreviation (Date)
Policies
What is it?
C-19R (3/25/20)
COVID-19 Relief Fund
COVID-19 Relief Fund provides monetary and food aid to lower-income families. [7]
SOP (3/25/20)
Standard of Procedure
Standard Operating Procedures were training manuals that were updated to provide training. For example, how to conduct COVID-19 testing effectively and safely on individuals as a Nepalese Health worker. [7]
QP (3/25/20)
Quarantine Protocols
Quarantine protocols were brochures provided to those that were exposed or positive cases on how to quarantine safely and successfully. [7]
C-19MCSP (4/1/20)
COVID-19 Management Centre & Social Policies
The COVID-19 Management Centre was responsible for the logistics of the movement of personal protective equipment, ventilators, and infected individuals to hospitals. Social Policies included Public Health Works where unemployed individuals were offered sufficient wages to help construct public projects that were funded by the Nepalese government. [4]
SCI (4/7/20)
Supreme Court Interim
The Supreme Court’s Interim occurred on April 7, 2020, which required all Nepalese migrant workers in different countries specifically in India to return to Nepal. [8]
HEP (6/20/20)
Health Sector Emergency Plan
The Health Sector plan was passed on June 20, 2020, where it prepared and strengthen the healthcare system in Nepal to combat COVID-19 surges. [7]

Figure 3: Highlighting Policies and Interventions before and within each peak.

Figure 4: Gender and Age Bracket Differences in Cases from April to September 2020.
Notable Peaks
Throughout Wave 1 and Wave 2, the daily cases for Peak 1 occurred before Wave 1 on June 17, 2020, with 586 daily cases per day, then Peak 2 occurred on October 21, 2020, after Wave 1 with 5,743 daily cases per day, and then after Wave 2, Peak 3 occurred on May 11th, 2020, with 9,483 daily cases per day (Figure 1A). As for daily mortalities, Peak 1 occurred on June 17, 2020, before Wave 1 with 1 death per day and Peak 2 occurred on November 4th with 43 deaths per day after Wave 1, and Peak 3 on May 19, 2021, with 246 deaths per day after Wave 2 (Figure 1B). Each Peak for daily mortalities and daily cases is near in terms of time.
Interventions and Policies in Wave 1 and Wave 2
Before Peak 1 (P1), 7 policy categories were recorded compared to none in Peak 1 and Peak 2 (P2 and P3). As of interventions reported, 6 were before Peak 1 compared to 2 before Peak 2, and 2 before Peak 3 (Figure 2).
First Peak
The daily cases start to increase on May 26, 2020, with 90 cases per day slowly rising into the next month peaking at 671 cases per day throughout June 2020. Then, continues to increase in July 2020 peaking at 743 cases at end of the month, and begins to decline (Figure 3A). As for the daily mortalities, the trend begins to increase with 1 death per day in May 2020 then peaks at 4 deaths per day on July 9, 2020, and slowly decreases. (Figure 3D). There are notable events around this time period, such as the inhibition of RDT testing on June 6, 2020, and the lifting of the national lockdown on July 1, 2020, occurring. [3]
Second Peak
The daily cases begin to increase in August 2020 with 1016 cases per day peaking at 5743 cases per day two months later and slowly decreasing in the upcoming two months (Figure 3B). As for the daily mortalities, it begins to increase with 11 deaths per day in August to where it continues to increase peaking at 43 deaths per day in November and decreasing towards the middle of November. However, starts to rise to a peak of 42 deaths per day in late November and decreases throughout December 2020 (Figure 3E). Notable events include the first Lockdown in Kathmandu on August 19, 2020, and then, the ending of the lockdown in Kathmandu a month after on September 10, 2020.
Third Peak
The daily cases begin to increase in April 2021 with 843 cases per day peaking a month after with 9,483 cases per day and slowly decreasing two months after (Figure 3C). As for the daily mortalities, starts increasing with 53 deaths per day in May 2021 to the peaking of 246 deaths per day in mid-May (Figure 3F). One important key trend is in August 2021, daily mortalities are following a decreasing trend whereas, daily cases are increasing. Three notable events were that Delta Variant was reported by the Nepal Ministry of Health on July 27, 2021 [9] and a small second lockdown period in Kathmandu occurred on April 29, 2021, and ended on May 13, 2021 [10]. Finally, Nepal accomplishes 2.62% vaccination of its citizens. [6]
Gender and Age Bracket Differences
As shown in the dark green and light green illustrates the majority of those who test positive for cases are ages 20-40 years old (Figure 3A). Furthermore, there is a gender difference between males and females illustrated with the majority of blue (males) comprising the total cases each month. However, the red (females) start to increase months after except June (Figure 3B).
Discussion
Peak 1
The increase in a spike of cases and mortality for the first peak can be best explained by the usage of the current testing kits and their lack of variety. Although RDT’s time period was before Peak 1, there is a possibility that this is responsible for the increase in daily cases. As the RDT kits were used from April 10, 2020, to July 6, 2020 (Covid-19 Status of Nepal), it was unable to catch most positive cases. Furthermore, the confirmatory testing strategy was only 10% for those who test negative to be tested for PCR due to the lack of expansion of laboratories for PCR testing [3]. As a result, this may explain the sudden rise in COVID-19 daily cases as more positive cases can be “captured,” (Figure 2A). Additionally, the daily mortality increases by a small amount during the earlier months of the pandemic to 0 deaths per day, and this could be responsible for the various interventions and policies implemented before Peak 1 (Figure 2). However, one month after the inhibition of RDT kits usage, daily cases, and mortality rate increased (Figure 3 A& D) To address this issue, the expansion of laboratories’ capacity for PCR testing began on March 29,2020. [3] where 18 laboratories were expanded to undergo PCR tests to the “6T principle of travel restriction, testing, tracing, tracking, treatment, and togetherness” to combat COVID-19 [11]. Weeks after, the COVID-19 PCR lab tests were at 19 institutions with one laboratory in each province. A year later, a total of 83 COVID-19 laboratories were formed. Most of those laboratories were from the private sector located in Kathmandu.3 However, there were problems as Nepal had a lack of infrastructure to follow the PCR testing recommended by the World Health Organization (WHO) to identify COVID-19. Additionally, a lack of trained personnel in using PCR in laboratories and interpreting the results was present. Furthermore, Nepal had laboratories that were not approved for biosafety in WHO standards and reports of exposure to health care workers. [3] Finally, there are improvements needed to be addressed in Nepal’s disease response to COVID-19.
Peak 2
The increasing daily cases and mortality in August 2020 could be best explained by the long history of young Nepalese migrating to India to work for economic opportunities due to an open border. [12] Strategies are needed to trace positive patients and have them isolated in addition to having those around them quarantined to limit disease spread. However, there were obstacles that Nepal health officials and the government faced. [11] For example, on April 7th, 2020, Nepal’s Supreme Court’s interim order stated to bring all Nepali migrant workers from the Indian Border [8]. Hence, the response was developing 20 ground crossing points from June 3 to August 10 for Nepal migrants to enter back to the country [3]. As thousands of Nepalese migrant workers were stuck at India and the Nepal border, the large borders made it difficult to maintain surveillance of border movement. As a result, contact tracing became difficult to continue and implement effectively when cases rosed up. [13] Working ages from 21-40 (light and dark green) constitute the majority of the positive cases among all age groups each month from Supreme Court’s interim order in April (Figure 4B). As a result, this could explain the disproportionate of male to female COVID cases as the majority of Nepali migrant workers are male. [12] Men comprise the majority of positive cases when compared to women among all positive cases each month after the Supreme Court Interim order from April (Figure 4A).
As India eased their border movement in April, more and more migrants stranded on the border increased. [8] The construction of quarantine centers and mandatory testing could not be followed by Nepal due to resource constraints. Most testing sites from “Quarantine centers” that hold returnees reported that most positive cases were difficult to locate the source of origin. [13] As the Quarantine Centers became full, the Nepal Government instructed individuals to self-isolate however, without follow-up, many individuals did not follow instructions. [13] Overcrowded and lack of medical staff, individuals escaped or left through the Mahakali River Tribhuvan [8], of which some had COVID-19 from the quarantine centers. Furthermore, contact tracing was not adequate due to stigmatization and discrimination against those who had COVID-19 for healthcare workers and patients. [14] Moreover, many lacked transportation to reach the ground crossing points from India and thus, died by walking. [8]
Peak 3
The rise of daily cases and mortalities on May 10, 2021, could be explained by the continued open border with India in March 2021 and the highly transmissible delta variant in India [15] following the increasing daily cases in August, a month after the Delta variant was reported in Nepal on July (Figure 3C). The removal of lockdown to mitigate mobility allowed individuals to spread the disease quicker. Furthermore, Nepalese migrants began to go home from India, which at that time had a rise in COVID-19 Delta cases. [16] Lack of interventions implemented on the Nepal-India border is possible a reason that could explain higher daily cases and mortality than the second wave. [16] By June 28, 2021, only 2.62% of Nepal’s total population were vaccinated making it vulnerable resulting in the second wave. [6] So far, 1 million doses of AstraZeneca donated from India were used to vaccinate essential workers such as ambulance drivers, frontline personnel, and sanitation workers on January 27, 2021, for the first phase. The Second phase included February 14, 2021, including government employees, banks, and journalists. The government had an expected plan for “72%” of the total 28.16 million individuals in the country however, only 3% were reached. The distribution of vaccines was distributed efficiently however there was a lack of donated vaccines.
Recommendations
In the Covid-19 Nepal Preparedness and Response Plan in April 2021, there should be a bullet point underneath 4.3 National Laboratories of Priority Preparedness Activities: “Develop a list of capable laboratories of handling PCR testing and ensure that there is enough present relative to each province’s population.” This is to mitigate disproportionately distributed laboratories concentrated on one area or district neglecting other areas that may need testing. Furthermore, to limit the time from shipping to the National Public Health Laboratory, there should be a secondary capable laboratory in each province that can immediately handle PCR testing in the future for faster results. Another intervention regarding this section is to increase the variety of testing methods. For example, “Utilizing colometric loop-mediated isothermal amplification (LAMP),” as an alternative to testing since it’s cheaper and successful at detecting COVID-19. [17] Hence, there should be underneath the 4.3 National Laboratories, “Increasing variety of appropriate testing methods that is cheaper and cost-effective in case of lack of testing supplies.” As a result, it’s better to have some sort of testing that has a low specificity and sensitivity rather than no tests at all. Additionally, there are scenarios where swift results are needed which is beneficial instead of waiting for delayed test results from the full capacity of laboratories [18] to prevent a situation where an individual is made aware they are positive, but due to the delayed results, they have infected many individuals making it hard for contact tracing to be effective. Training and workshops on how to use PCR testing are valuable however, it needs to be in a virtual format instead of a WHO official visiting to limit physical contact emphasizing protecting health care workers. Thus, Training modules from World Health Organization to prevent contact should be requested. Although 4.3 National Laboratories says, “weekly engagement in virtual interactive sessions…” there is no specific scenario for foreign training thus, it could be “weekly engagement in virtual engagement in virtual interactive sessions from foreign officials and within health officials in Nepal on addressing challenges.”
As for 2. Protection, there is the utilization of ambulances regarding refugees with “Continued ambulance and hospital transfer service to address the needs of refugees and vulnerable members of the host community…” However, this is within Nepal and does not include the Nepalese working migrants in India. As previously mentioned, many Nepal migrant workers passed away walking from India to reach the crossing points. [8] Hence, another bullet point could be added, “Extra ambulances or Army vehicles reserved to help transport stranded Nepali migrant workers in other countries.” Furthermore, there is a lack of policies regarding sanitation and crowd-control pertaining specifically to the India-Nepal Border quarantine centers along with timely data collection and managing efficiently for contact tracing. Additionally, a monitoring system movement is needed in the border control of India through the points of entry. Although underneath CCCM/Shelter Cluster it states, “construct or improve critical infrastructure at PoEs… improve isolation and quarantine centers,” it is not specific enough to the India-Nepal Border. Focusing on this key open border since most of the Nepali migrants’ work can be beneficial if reserved resources are placed. Hence, a change could be “improving infrastructure at POEs and quarantine centers with an emphasis on the India-Nepal Border.”
Conclusion
Overall, at the beginning of the Pandemic, Nepal did a great job setting up interventions and policies, however, could not keep its consistency in mitigating disease spread and preventing mortality. Most of the explanations and recommendations were based on deduction from the graphs and literature thus, recommendations may not be feasible as something written on paper could have different outcomes when implemented. There are multiple interventions, policies, and external factors that were not explained since there was a lack of information on various time periods from grey and scholarly literature. Thus, more thorough analysis and data need to be obtained and conducted. However, the most important aspect is Nepal’s willingness to improve and be ready for any possible future Pandemics shown through their improvements and updating their COVID-19 Disease Response Plans.
Limitations of the study: There was a lack of sources regarding contextual information in wave two, thus more sources are needed to gain accurate inferences. Inferences were based upon available resources, thus only what was reported is known. Additionally, the author acknowledges that many solutions and interventions recommended may only be effective on paper but not in real-life scenarios.
Future scope of the study: An in-depth analysis of policies’ effectiveness using mathematical modeling such as linear regression for more accurate predictions of mortalities and morbidities.
What is already known on this topic: There are a few studies that provide contextual information on what the policies have done in Nepal at the individual level.
What this study adds: This study contributes to changes in the Covid-19 Nepal Preparedness and Response Plan in April 2021.
Acknowledgments: I wish to thank Dr. Marahatta and all the UC DAVIS faculty and students for being part of my journey and providing this opportunity to contribute to Nepal’s efforts in disease mitigation.
Conflict of interest: None
References
- Nepal COVID-19 Dashboard & Daily Situational Reports. Accessed May 21, 2022.
- Rayamajhee B, Pokhrel A, Syangtan G, et al. (2021) How Well the Government of Nepal Is Responding to COVID-19? An Experience From a Resource-Limited Country to Confront Unprecedented Pandemic. Front Public Health. 9:597808.
- Responding to COVID-19 Health sector preparedness, response and lessons learnt. Published online 2021.
- Srivastava N, Nepal B, Gauchan B, Kennedy A (2021). Policy Responses to the COVID-19 Pandemic in Nepal. 0 ed. International Food Policy Research Institute.
- Sah R, Khatiwada AP, Shrestha S, et al. (2021). COVID-19 vaccination campaign in Nepal, emerging UK variant and futuristic vaccination strategies to combat the ongoing pandemic. Travel Medicine and Infectious Disease; 41:102037.
- Uwishema O, Abbas KS, Torbati T, et al. (2021). The second wave of COVID‐19 hits Nepal: Burden for Nepal’s healthcare system. Health Sci Rep. 4:e371.
- Basnet BB, Bishwakarma K, Pant RR, et al. (2021). Combating the COVID-19 Pandemic: Experiences of the First Wave From Nepal. Front Public Health. 9:613402.
- Baniya J, Bhattarai S, Pradhan V, Thapa BJ. Visibility of Invisible: Covid-19 and Nepal-India Migration. Tribhuvan University Journal. Published online September 27, 2020:101-114.
- Nepal confirms new mutant of “Delta” variant of Covid-19. The Times of India.
- Prasain S. Nepal’s lockdown 2.0, new Covid curbs on travel. The Kathmandu Post. Published April 28, 2021. Accessed May 21, 2022.
- Sharma S, Bhatta J. Public health challenges during the COVID-19 outbreak in Nepal: a commentary. JHR. 2020; 34:373-376.
- Sharma JR. Marginal but Modern: Young Nepali Labour Migrants in India. YOUNG. 2013; 21:347-362.
- Panthee B, Dhungana S, Panthee N, Paudel A, Gyawali S, et al. (2020). COVID-19: the current situation in Nepal. New Microbes and New Infections. 37:100737.
- Kansakar S, Dumre SP, Raut A, Huy NT. From lockdown to vaccines: challenges and response in Nepal during the COVID-19 pandemic. The Lancet Respiratory Medicine. 2021; 9:694-695.
- Mahase E. Delta variant: What is happening with transmission, hospital admissions, and restrictions? BMJ. 2021; 373:n1513.
- Analysis of second wave of COVID-19 cases in Nepal with a logistic model | Asian Journal of Medical Sciences. Accessed March 22, 2022.
- Giri AK, Rana DR. Charting the challenges behind the testing of COVID-19 in developing countries: Nepal as a case study. Biosafety and Health. 2020; 2:53-56.
- Ricks S, Kendall EA, Dowdy DW, Sacks JA, Schumacher SG, Arinaminpathy N. Quantifying the potential value of antigen-detection rapid diagnostic tests for COVID-19: a modelling analysis | SpringerLink. Springer Published March 9, 2021. Accessed May 22, 2022.