Publication Information
ISSN: 2641-693X
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Left Atrial Myxoma with Systemic Emboli and Neovascularization: A Case Report
Hind Tahri Joutey*, Saousan Serbout, Meryem Haboub, Marouane Selmaoui, Ghali Bennouna, Leila Azzouzi, Rachida Habbal
Department of Cardiology, Ibn Rochd University Hospital, Casablanca, Morocco
Received Date: March 03, 2020; Accepted Date: March 09, 2020; Published Date: March 18, 2020
*Corresponding author: Hind Tahri Joutey, Department of Cardiology, Ibn Rochd University Hospital, Casablanca, Morocco. Tel: +212660008535; Email: tahri-hind@hotmail.fr
Citation: Joutey HT, Serbout S, Haboub M, Selmaoui M, Bennouna G, Azzouzi L, Habbal R (2020) Left Atrial Myxoma with Systemic Emboli and Neovascularization: A Case Report. Int Jr Cardiac Sci and Res: IJCSAR-118.
Abstract
Background: Primary intracardiac tumors are rare. Approximately 50% of them are myxomas, located most frequently in the left atrium. Despite the benign histological nature of myxomas, its intracardiac localization engages vital prognostic primarily due to embolic complications. We hereby present a rare case of left atrial myxoma with systemic emboli and neovascularization.
Case Report: A 63-year-old female with no conventional vascular risk factors such as hypertension, diabetes, dyslipidemia or tobacco use, was admitted with left hemiplegia one month prior to the current evaluation complaining of severe headaches. Infarction over the right middle cerebral artery was disclosed on magnetic resonance imaging study. The biological evaluation was normal without any relevant abnormalities. Echocardiography showed dilated left atrium due to large left atrial mass consistent with a primary myxoma .The mass was attached to the inter-atrial septum and prolapsed into left ventricle during diastole. During hospitalization, she complained of an abdominal pain after which a CT-scan was performed revealing signs of a hepatic infarct. Pre-surgical coronary angiography showed the presence of a vascular structure originating from the left circumflex coronary artery to the left atrial tumor suggestive of neovascularization. The treatment of choice was surgical and the cardiac myxoma was removed with positive outcomes. At the 6 months follow up, an echocardiography was performed with no signs of recurrence.
Conclusion: Atrial myxoma is a common benign cardiac tumor which can present in different ways. Stroke is a key clinical evaluation and complication which can support its diagnosis .We emphasize that patients with multiple emboli should be carefully followed up for atrial myxoma and surgical resection remains the gold standard for the prevention of embolization.
Keywords: Atrial Myxoma; Neovascularization; Stroke; Systemic Embolization
Background
Primary cardiac tumors are rare with an autopsy frequency of only 0.001-0.03%. Of the primary cardiac tumors encountered in adult patients, over 72% are benign of which the lesions are myxomas [1]. Despite its benign histological nature, the intracardiac localization engages vital prognostic primarily due to embolic complications [2]. It’s also characterized by a clinical polymorphism which complicates the clinical evaluation; for this reason, the echocardiogram represents the gold standard for the diagnosis of myxomas [3]. With regards to clinical interventions, surgical resection is the only proven effective treatment to prevent the complications associated with myxomas. This highlights the importance of adequate and appropriate resection, precise exploration of the four cardiac cavities, and a regular echocardiography guided follow-up. Lastly, it is important to note that tumor neovascularization in cardiac myxomas has been reported in some cases.
In this case-report, we present the clinical case and evolution of a patient with an intracardiac myxoma associated with systemic emboli; cerebral and hepatic. This myxoma was also characterized by the presence of a neovascularization from the left circumflex.
Case Report
The patient was a 63-year-old female with a past medical history negative for diabetes, tobacco use, hypertension, and dyslipidemia who presented to the emergency department one month prior to the current admission for a left hemiplegia associated with recurrent headaches. Cerebral computerized tomography scan and magnetic resonance imaging (MRI) were performed revealing an acute ischemic stroke of the right middle cerebral artery (Figure 1).
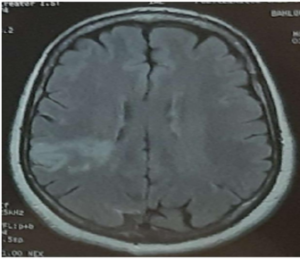 Figure 1: Brain MRI revealed cerebral infarct in right middle cerebral artery.
Figure 1: Brain MRI revealed cerebral infarct in right middle cerebral artery.
Furthermore, and in the setting of the ischemic stroke, we conducted an arterial doppler echocardiography of supra-aortic trunks which revealed an atheromatous surcharge without significative stenosis and permeable arteries with adequate downstream flow. We also conducted a transthoracic echocardiogram (TTE) which revealed a non-dilated left ventricle without signs of hypertrophy with regular contractility and a preserved systolic function with the presence of a 61mm x 31mm solid ovoid mobile mass in the left atrium inserted in the interatrial septum prolapsing in the left ventricle during diastole consistent with a primary myxoma of the left atrium (Figure 2). The patient was then admitted in the cardiology department within our institution.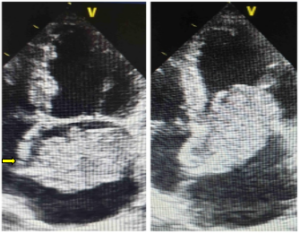 Figure 2: TTE showing a mass measuring 61×31 mm attached to interatrial septum (arrow) and prolapsing through the mitral valve consistent with left atrial myxoma.
Figure 2: TTE showing a mass measuring 61×31 mm attached to interatrial septum (arrow) and prolapsing through the mitral valve consistent with left atrial myxoma.
Upon admission to the cardiology department, she was conscious with a Glasgow score of 15, a maintained left hemiparesis, and presented stage II dyspnea. The heart rate was normal at 75 bpm and the blood pressure was 120/70 mmHg. The cardiac rhythm on electrocardiogram was abnormal sinus rhythm with T-waves inversion in lead V1, V2, and V3. The biological evaluation was normal without any relevant abnormalities.
During hospitalization, she complained of an abdominal pain for which a thoracoabdominal CT scan was performed which showed non-enhancing hypodense areas in his liver suggestive of hepatic infarct and showed also the intracardiac mass (Figure 3).
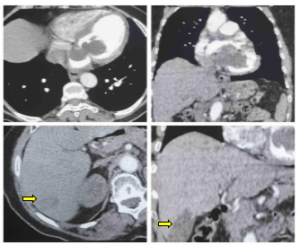 Figure 3: CT thoracoabdominal scan showing the intracardiac mass and a hypodense lesion (arrow) in the liver suggestive of a hepatic infarct in axial and coronal section.
Figure 3: CT thoracoabdominal scan showing the intracardiac mass and a hypodense lesion (arrow) in the liver suggestive of a hepatic infarct in axial and coronal section.
Presurgical coronary angiography (CAG) was realized to eliminate the presence of significative coronary lesions and revealed an angiographically normal coronaries with the presence of an intramyocardial bridge in the middle interventricular artery and a neovascularization initiating from the left circumflex and expanding towards the mass in the left atrium (Figure 4).
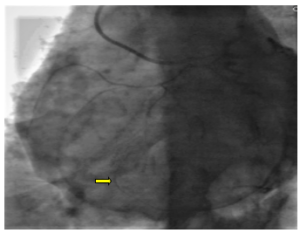 Figure 4: CAG showing a feeding artery (arrow) originating from the left circumflex artery supplying the left atrial mass.
Figure 4: CAG showing a feeding artery (arrow) originating from the left circumflex artery supplying the left atrial mass.
The patient was placed under extracorporeal membrane oxygenation for the surgical intervention to completely extract the mass. The intervention was without complications and the postoperative evolution was uneventful. At the 6 months follow up, an echocardiography was performed and showed no residual intracardiac tumor.
Discussion
Myxoma is the cardiac tumor of most frequent incidence representing 50% of all primitive cardiac tumors [4]. There are commonly located in the left atrium and mainly originates from an area in the atrial septum near the fossa ovalis. Other locations involved such as the right atrium and the ventricles have been reported in various case reports [5]. Cardiac myxomas are sporadic with an incidence primarily identified in middle-aged women where the lesions are most often isolated. The intracardiac obstruction of cardiac myxomas is the origin of the clinical symptoms such as mitral stenosis, coronary embolization, systemic embolization, or systemic constitutional manifestations [2]. Of these complications, systemic emboli are well known and frequent as they can occur in 40-50% of patients; in most cases, the cerebral arteries, including the retinal arteries, are affected. Embolization to other arterial systems including coronary arteries, upper and lower extremities, kidney, spleen, and liver can also occur [6]. Similarly, our patient had cerebral and hepatic infarct due to tumor embolization.
Arterial emboli associated to cardiac myxomas concern the coronary field in 10% of cases [7] and the cerebral arterial field in 50% of cases [8]. The emboli correspond to fragments of the tumor in most cases or thrombi forming at the surface of the mass [9]. The cardiac echocardiography is the gold standard clinical evaluation imaging to confirm a positive diagnosis with a sensitivity of 93% for the transthoracic technique and 97% of the trans-esophageal technique [10]. TTE allows determining and evaluating the embolic risk of myxomas. The morphology of the myxoma is directly correlated to the embolic risk; polypoid masses are considered fragile and thus are more likely to embolize compared to masses with a gelatinous and regular morphology [11]. On the other hand, the size of the myxoma, which can vary from a few millimeters to over 15 centimeters, is not correlated to the risk of emboli [1]. As in our case, an intermittently prolapsing mass seen in echocardiography puts the patient at high risk of embolism [12].
The only curative treatment for myxoma is the surgical resection under extracorporeal circulation. The removal of atrial myxoma carries an operative mortality rate of 5% or less. Atrial myxomas can recur following surgical resection and overall risk of recurrence is approximately 12% for familial tumors and only 1% to 3% for sporadic tumors [2].
The presence of neovascularization in cardiac myxomas has been reported in some cases. During CAG, such neovascularization is usually verified. In our case, anomalous tortuous vascular structure originating from the left circumflex coronary artery to the left atrial tumor suggestive of neovascularization was found. CAG should be performed routinely in order to eliminate any coronary lesions and to detect the presence of tumor-supplying vessels. Other studies have suggested that CAG should only be performed in the case of selected patients, particularly those over the age of 40 years and those with atherosclerotic risk factors undergoing surgical removal of a cardiac mass [13]. Presence of a large feeding artery substantially changes the operative strategy because large feeding arteries must be ligated in addition to excision of the myxoma [14].
Conclusion
Embolic accidents represent a major complication of myxomas which can complicate the prognosis of these tumors which are benign in nature. The treatment gold standard is surgical and urgent notably in the presence of morphological characteristics predictive of embolism risk under echocardiography. Surgical intervention remains the primary preventive treatment for systemic emboli.
Competing Interests: The authors declare that they have no competing interests.
References
- Cohen R, Singh G, Mena D, Garcia CA, Loarte P, et al (2012) Atrial Myxoma: A Case Presentation and Review. Cardiol Res 3: 41-44.
- Latifi AN, Ibe U, Gnanaraj J (2019) A case report of atrial myxoma presenting with systemic embolization and myocardial infarction. Eur Heart J Case Rep 3: 1-5.
- Karabinis A, Samanidis G, Khoury M, Stavridis G, Perreas K (2018) Clinical presentation and treatment of cardiac myxoma in 153 patients. Medicine (Baltimore) 97: e12397.
- Lam KY, Dickens P, Chan AC (1993) Tumors of the heart. A 20-year experience with a review of 12,485 consecutive autopsies. Arch Pathol Lab Med 117: 1027-1031.
- Snyder SN, Smith DC, Lau FY, Turner AF (1976) Diagnostic features of right ventricular myxoma. Am Heart J 91: 240-248.
- Wu Y, Fu X-M, Liao X-B, Zhou X (2018) Stroke and peripheral embolisms in a pediatric patient with giant atrial myxoma: Case report and review of current literature. Medicine (Baltimore) 97: e11653.
- Kamata S, Kawada T, Kikuchi K, Miyamoto S, Nishimura K, et al (1996) [Clinical analysis of embolism with left atrial myxomas]. Kyobu Geka 49: 297-300.
- Bayir H, Morelli PJ, Smith TH, Biancaniello TA (1999) A left atrial myxoma presenting as a cerebrovascular accident. Pediatr Neurol 21: 569-572.
- Shrestha S, Raut A, Jayswal A, Yadav RS, Poudel CM (2020) Atrial myxoma with cerebellar signs: a case report. J Med Case Rep 14: 29.
- Braun S, Schrötter H, Reynen K, Schwencke C, Strasser RH (2005) Myocardial infarction as complication of left atrial myxoma. Int J Cardiol 101: 115-121.
- Ha JW, Kang WC, Chung N, Chang BC, Rim SJ, et al. (1999) Echocardiographic and morphologic characteristics of left atrial myxoma and their relation to systemic embolism. Am J Cardiol 83: 1579-1582, A8.
- Selkane C, Amahzoune B, Chavanis N, Raisky O, Robin J, et al. (2003) Changing management of cardiac myxoma based on a series of 40 cases with long-term follow-up. Ann Thorac Surg 76: 1935-1938.
- Kim YK, Yong HS, Kang E-Y, Woo OH (2009) Left atrial myxoma with neovascularization: detected on cardiac computed tomography angiography. Int J Cardiovasc Imaging 1: 95-98.
- Dubey L, Chaurasia AK (2012) Neovascularization in Left Atrial Myxoma. Int Cardiovasc Res J 6: 133-134.