Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Impact of Timing and Surgical Decompression with Posterior Stabilization on Clinical Outcome in Patients of Thoracolumbar Spine Injury
Tausif Ahmed A. Shikalgar*, Surendra K. Shukla, Nishat Goda, Pankaj Singh
Department of Orthopaedics, K. J. Somaiya Medical College and Hospital, Sion, Mumbai, India
Received Date: April 25, 2022; Accepted Date: May 10, 2022; Published Date: May 17, 2022
*Corresponding Author: TausifAhmed A. Shikalgar, Department of Orthopaedics, K. J. Somaiya Medical College and Hospital, Sion, Mumbai, India. Email: Dr.tausifahmedshiklgar@gmail.com
Citation: Shikalgar TA, Shukla SK, Goda N, Singh P (2022) Impact of Timing and Surgical Decompression with Posterior Stabilization on Clinical Outcome in Patients of Thoracolumbar Spine Injury. Adv Ortho and Sprts Med: AOASM-165.
DOI: 10.37722/AOASM.2022201
http://doi.org/10.37722/AOASM.2022201
Abstract
Objective: To evaluate the impact of timing and Surgical decompression and stabilization on the clinical and neurological outcome in patient with thoracolumbar spine injury.
Study Design: Prospective study
Material and Methods: In all, a total of 25 cases were evaluated from April 2017 to April 2018. The pre-operative neurological status was graded on basis of ASIA grading. Patients in one group underwent posterior stabilization, decompression of the cord and fusion whereas patients of another group underwent only posterior stabilization with fusion without any direct decompression to evaluate the impact of decompression on neurological recovery. Patients were followed up regularly in OPD after the discharge. Neurologic status of each patient was evaluated during each follow up visits.
Results: Significant improvement was observed in ASIA score of the patients with direct decompression as compared to indirect decompression at discharge and subsequent follow-ups (p<0.05). Significant improvement was observed in ASIA score of the patients with interval between injury and surgery ≤24 hours as compared to interval between injury and surgery >24 hours at discharge and subsequent follow-ups (p<0.05).
Conclusion: Early surgery (≤24 hours) and posterior instrumentation with direct decompression has better outcome than late surgery (>24 hours) and posterior instrumentation with indirect decompression.
Keywords: Thoracolumbar spine injury. Direct Decompression, Indirect Decompression, ASIA Score, Neurological recovery
Introduction
The spinal trauma is one of the leading problems in orthopaedic practice, more so in modern era where the individuals are more at risk due to high energy trauma. It is one of the grave injuries that cause infinite morbidity and disability to the patient. The hopelessness and helplessness experienced by patient and doctors until the present time has been expressed by writer Edwin Smith Papyrus.
Thoracolumbar spinal segment is the 2nd most commonly involved segment after the cervical segment in spinal injuries, about 30 to 60% of all spinal injuries. Thoracolumbar injuries in trauma are concentrated at the thoracolumbar junction region, 60% occurring between T12 and L2 [1]. 15 to 20% patients with fracture at thoracolumbar level have associated neurological injury [2].
Acute spinal cord injury remains an important cause of morbidity and mortality. It involves both primary and secondary mechanism of injury.
Primary Mechanism
The primary mechanism is the initial mechanical injury due to local deformation and energy transformation from acute compressive, lacerating, distracting or shear forces.
Secondary Injury
It is a cascade of primary injury mechanism. It includes ischemia, electrolyte derangement, lipid per oxidation, vascular changes, neurotransmitter accumulations, free radical production and oedema, inflammation, ATP depletion and apoptosis. Secondary injury can also arise from poorly immobilised unstable injuries which cause a further mechanical injury with further displacement. Secondary injury is preventable and may be reversible. The treatment options for unstable thoracolumbar spine fractures and fracture dislocations have long been controversial. Many authors, advised non-operative treatment, but later report emphasized the advantage of open reduction internal fixation with posterior instrumentation [3, 4]. Most authors agree that neurological improvement is independent of treatment modality.5But the advocates of surgical decompression point at advantages of surgery in improving neurological deficits. Lately consensus is evolving around the world for stabilization of spine, with fusion and instrumentation in unstable fracture [3]. Historically, thoracolumbar fractures have been treated with recumbency i.e. to bed rest for a period of 8-12 weeks [5]. This mode of treatment is accompanied with complication due to recumbency. Internal fixation and stabilization of spinal lesion allows early mobilization of all patients, regardless of neurological deficit, while protecting the neurological structures from further injury and enhancing their recovery [6].
Surgical treatment can be anterior, posterior or anterioposterior. As most orthopaedic and spinal surgeons are more experienced in posterior approach and at the same time this approach requires less operative time with less blood loss, hence a safe alternative [1]. Decompression of neural elements, stabilization of the spine and maintenance of the tissue perfusion are fundamental to optimizing outcomes in spinal cord injury. Removal of damaging bone, disc and ligament fragments to decompress the swollen cord should limit the secondary damage and improve the outcome. The goals of surgery are to achieve stability, to correct deformity, early mobilization, to expedite post-operative recovery and to decrease pseudoarthrosis. The pedicle screw, plate or rod construct helps to achieve all these [8]. In Variable screw placement the fixation achieved is more rigid as the screw is passed through the “force nucleus” of the vertebrae [9]. This is the post through which five anatomical structures - the superior facet, the inferior facet, the lamina, the pedicle and the transverse process, channel all posterior forces that are transmitted to the body [10]. Optimal timing of decompression and surgical stabilization of spinal fractures is controversial. No clear consensus can be inferred from the literature about optimal timing of decompressive surgery. Information about the effect of early surgical decompression of spinal fractures with neurological deficit at thoracolumbar region is sparse. So we aimed to evaluate the impact of timing of decompression and stabilization on the clinical and neurological outcome.
Methodology
This study is a prospective clinical study of thoracolumbar spinal injuries by posterior instrumentation (pedicular screw and rod fixation in thoracic, lumbar, and thoracolumbar spinal fractures). In all, a total of 25 cases were evaluated and assessed during the period from April 2017 to April 2018. The study was conducted in the Department of Orthopaedics, K. J. Somaiya Medical College and Hospital Sion, Mumbai.
All the patients underwent treatment, as per a specific treatment plan. All the patients were initially assessed in the outpatient department or emergency department according to their presentation and then they underwent a detailed evaluation of their hemodynamic status, spine, neurological status and other injuries if associated with trauma. The patients were interviewed; their epidemiological, historical, subjective and physical findings were noted. After initial investigations and hemodynamic stabilization, patients were assessed neurologically in detail. A neurological chart was maintained for each patient. All the patients had routine X-rays of thoracolumbar spine anterioposterior and lateral views. In all the patients, MRI was done. X-ray of other areas is done if injuries are suspected. All patients under went all routine blood and radiological investigations to rule out any co-morbidities.
The pre-operative neurological status was graded on the basis of ASIA grading. It was also used to assess post-operative recovery and follow-up. The indication for the surgery was thoracolumbar spine injury having instability with neurological deficit and /or spinal canal compromise and compression on the spinal cord. Patients of Thoracolumbar spine injury having instability with neurological deficit and /or spinal canal compromise and compression on the spinal cord and patients with stable medical condition and normal biochemical profile are included in the study Patients with intact neurological status, unstable clinical condition and abnormal biochemical profile, severe multi system injury (having major chest and abdominal trauma), patients with polytrauma, patients with secondaries and malignancy (Pathological fractures) are excluded from study. After necessary preoperative investigation, all patients will be operated under general anesthesia as early as possible. Patients in one group underwent posterior stabilization, decompression of the cord and fusion whereas patients of another group underwent only posterior stabilization with fusion without any direct decompression to evaluate the impact of decompression on neurological recovery.
All the patients were given post op intravenous antibiotics (third generation cephalosporin + aminoglycoside) for 5 days. They were switched over to oral antibiotics till suture removal. Intravenous dexamethasone 4 mg IV was given for 3 days. Physiotherapy was started from first day post operatively. Sutures were removed on fourteenth day. On the second day patients were allowed to roll from side to side. They were allowed to sit up and were mobilized on a wheel chair after application of knight tailor brace on third or fourth post-operative day. A close watch was kept for any improvement or deterioration in the neurological status.
Patients wore knight tailor brace for about 6 weeks. Those with incomplete neurological deficits were given physiotherapy and gradually ambulated. Patients with complete neurological deficits were given physiotherapy and ambulated on wheel chair. Routine postoperative X-rays were taken prior to discharge. The neurological grading and radiological parameters were recorded on 3rd day of the operation.
Patients were followed up regularly in OPD after the discharge from the hospital. Patients were initially followed up every 4 weeks for 3 months, then at every 12 weeks till the last follow up. Neurologic status of each patient will be evaluated during each follow up visits. Statistical Analysis was performed with help of Epi Info (TM) 7.2.2.2 EPI INFO is a trademark of the Centers for Disease Control and Prevention (CDC). Descriptive statistical analysis was performed to calculate the means with corresponding standard deviations (S.D.)test of proportion was used to find the Standard Normal Deviate (Z) to compare the difference proportions and Chi-square () test was performed to find the associations. t-test was used to compare two means. Pearson Correlation Co-efficient was calculated to find the correlation between two variables. p<0.05 was taken to be statistically significant (Figure 1, 2, 3 and 4).

Figure 1: showing pre-op X-ray of the patient with fracture of L1 vertebra.
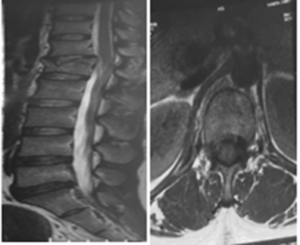
Figure 2: showing MRI of the patient with cord compression at L1 level.
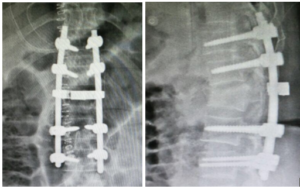
Figure 3: showing immediate pre-op X-ray of the patient.
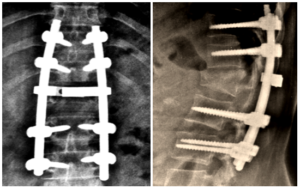
Figure 4: showing x-ray at 6 months follow up.
Results
In our study we had 72% males and 28% female patients. The mean age (mean ± S.D.) of the patients was 28.44±6.29 years with range 19 – 39 years and the median age was 28 years (Table 1). We noted fall from a height in 68% patients as the most common mode of injury and was mainly the result of work injury. Road traffic accident was the second commonest cause 32% of patients (Table 2).In our series most of injuries were at L1 (32.0%) followed by D12 (24.0%), L2 (20.0%) and D11 (16.0%) which were significantly higher than other (Z=2.82; p<0.01) (Table 3).Surgeries performed after 24 hours of injury were 60% and surgeries performed before 24 hours were 40%. Only 3(12.0%) of the patients were operated within 6 hours after the injuries. Posterior Stabilization with Direct Decompression was underwent (52.0%) which was higher than Posterior Stabilization with Indirect Decompression (48.0%) but it was not significant (Z=0.56; p>0.05) (Table 4).
There were no significant differences in all the base parameters of the patients who were underwent two different types of surgeries (p>0.05) i.e. posterior stabilization with direct decompression vs posterior stabilization and indirect decompression. Thus the patients of the two groups were matched for age, gender, place of residence and mode of injury.
There was no significant difference in ASIA score of the patients before surgery (p>0.05) and significant association was found ASIA score of the patients at discharge. Significant improvement was observed in ASIA score of the patients with direct decompression as compared to indirect decompression at discharge (p<0.05). Significant improvement was observed in ASIA score of the patients with direct decompression as compared to indirect decompression at subsequent follow-ups after discharge (p<0.05). There were no significant differences in all the base parameters of the patients who were underwent surgeries after 24 hours and within 24 hours (p>0.05). Thus the patients of the two groups were matched for age, gender, place of residence and mode of injury.
There was no significant difference in ASIA score of the patients before surgery (p>0.05) and significant association was found ASIA score of the patients at discharge. Significant improvement was observed in ASIA score of the patients with interval between injury and surgery≤24 hours as compared to interval between injury and surgery>24 hours at discharge (p<0.05). Only 5(20.0%) of the patients had post-operative complications which was not significant (Z=1.26>0.05). Out of the post-operative complications 60.0% of the patients had Pulmonary Complications (60.0%) which was significantly higher than that of Local Wound Infection (40.0%) (Z=2.82; p<0.01) (Table 5).
Pulmonary complication was higher in Indirect Decompression as compared to direct Decompression. Also, all the complication were with the patients with interval between injury and surgery>24 hours (p<0.001). There was no complication with the patients with interval between injury and surgery≤24 hours. The mean duration of hospital stay (mean ± S.D.) of the patients was 29.92±11.13 days with range 14 – 56 days and the median was 28 days. Most of the patients were discharged within 4 weeks (56.0%) (Z=2.06; p>0.05). Only 12.0% of the patients were discharged beyond 6 weeks. There no significant difference in mean duration of hospital stays of the patients undergoing posterior stabilization with direct decompression or posterior stabilization with indirect decompression. However the mean duration of hospital stay of the patients with interval between injury and surgery>24 hours was significantly higher than that of the patients with interval between injury and surgery≤24 hours (p<0.001). (in years) (n=18) (n=7) Complications
Age Group
Gender
TOTAL
Male
Female
<20
0
1
1
20 -29
10
3
13
30 – 39
8
3
11
TOTAL
18
7
25
Mean ± SD
29.16±6.41
26.57±6.02
Median
28
28
Range
20 - 39
19 – 35
Mode of injury
Number
%
Fall from height
17
68.0%
RTA
8
32.0%
Total
25
100.0%
Level of injury
Number
%
D10
1
4.0%
D11
4
16.0%
D12
6
24.0%
L1
8
32.0%
L2
5
20.0%
L3
1
4.0%
Total
25
100.0%
Procedure done
Number
%
Posterior Stabilization and Indirect Decompression
12
48.0%
Posterior Stabilization with Direct Decompression
13
52.0%
Total
25
100.0%
Post-operative
Number
%
Local Wound Infection
2
40.0%
Pulmonary Complications
3
60.0%
Total
5
100.0%
Discussion
In our study we had 72% males and 28% female patients. The mean age (mean ± S.D.) of the patients was 28.44±6.29 years with range 19 – 39 years and the median age was 28 years. Most of the patients (52.0%) were in the age group between 20 – 29 years followed by 30 – 39 years which were significantly higher than other age group (Z=6.62;p<0.001). Thus thoracolumbar spine injuries were more prevalent in the age group between 20 – 29 years in this study. Gregory F. Alvine et al. [11] in their study found that average age was 31 years, with a male predominance. Nasser M.G et al. [12] in their study found that average age was 28.8 years with a male predominance. Rick C. Sasso et al. [13] in their study had 77% males and 23% females with a mean age of 34 years. Razak M. et al. [14] in their study found that average was 30 years with a male predominance.
Nasser M.G. et a. [12] in their study noted that the main cause of injury was fall from a height and road traffic accident was the second commonest. Gregory F. Alvine et al11 noted that in 52% of patients injuries resulted from fall from a height, in 39% patients due to road traffic accidents and 9% due to fall of heavy objective. Razak M et al. [14] in his study noted that 69% of injuries were caused from fall from height, 31% due to road traffic accident. In our series most of injuries were at L1 (32.0%) followed by D12 (24.0%), L2 (20.0%) and D11 (16.0%) which were significantly higher than other (Z=2.82; p<0.01). Nasser M.G. et al. [12] in their study noted that the commonest vertebra to be fractured was L1 comparable to our study. Gregory F. Alvine et al. [11] noted that in 72.5% of cases the injury was at level of T11-L2. Rick C. Sasso et al. [13] noted that in 80% of cases the injuries were at T11-L2 levels. Razak M et al. [14] noted that in 92% of cases the injuries were at the L1 and L2 vertebral levels. In our series surgeries performed after 24 hours of injury were 60% and surgeries performed before 24 hours were 40%. Only 3(12.0%) of the patients were operated within 6 hours after the injuries.
Étienne Bourassa, et al. [15], in their study 72% of patients were operated <24h post-trauma where as 28% were operated ≥24h post-trauma. Campagnolo et al [7] grouped patients in Early spinal Stabilization group:<24h; Late spinal stabilization group:>24 h. McLain and Benson [16] grouped patients in Urgent surgery group: <24 h; early surgery group: from 24 to 72 h. JR Wilson, et al. [17] performed grouped analysis comparing the cohort of patients who received early surgery (<24h after SCI) to those receiving delayed surgery (>24h after SCI). In our series mostly Posterior Stabilization with Direct Decompression were underwent (52.0%) which was higher than Posterior Stabilization with Indirect Decompression (48.0%) but it was not significant (Z=0.56; p>0.05). Deuk Soo Jun, et al. [18] in their study laminectomy and direct decompression was performed in all patients. In study conducted by Zhigang Zhang, et al. [19] posterior indirect reduction and pedicle screw fixation were conducted for all the patients. Whereas in study conducted by Subarna Mishra, et al. [20] posterior stabilization with Direct or indirect decompression was done. Significant improvement was observed in ASIA score in our series of the patients with direct decompression as compared to indirect decompression at subsequent follow-ups after discharge (p<0.05).
Olumide A. danisa, et al. [21] in their study concluded that posterior surgery, takes the least time, causes the least blood loss, and is the least expensive of the three procedures. Cengiz, et al. [22] in their study concluded that early surgery may improve neurological recovery. Thomas M. Frangen, et al. [23] in their study concluded that patients were not harmed by an early operation. Deuk Soo Jun, et al. [18] in their study concluded that the posterior direct decompression could be used as one of treatments for lower thoracic and lumbar fractures combined with neurologic injuries. Mahmoud Yousefifard, et al. [24] concluded that early spinal decompression surgery can improve neurologic recovery and is associated with less post-surgical complications. There was no significant difference in ASIA score of the patients before surgery (p>0.05) and significant association was found ASIA score of the patients at discharge. Significant improvement was observed in ASIA score of the patients with interval between injury and surgery≤24 hours as compared to interval between injury and surgery>24 hours at discharge (p<0.05). McLain and Benson [16] in their study concluded that urgent group (<24 hours) showed a higher mean neural improvement & recovery. JR Wilson, et al. [17] concluded that surgical decompression performed before 24 h post injury has the potential to result in superior motor recovery in comparison with late surgery performed at or after 24 h post injury. Marcel F. Dvorak, et al. [25] concluded that for an incomplete acute SCI in the cervical, thoracic, or thoracolumbar spine, surgery performed within 24 h from injury improves motor neurological recovery. Étienne Bourassa, et al. [15] concluded that early surgical intervention within 24h following a traumatic complete SCI may promote neurological recovery. Subarna Mishra, et al. [20] in their study concluded that earlier the surgical decompression done, the better the neurological and bowel/bladder function recovery both in complete and incomplete paraplegic cases.
Only 5(20.0%) of the patients had post-operative complications which was not significant (Z=1.26>0.05). Out of the post-operative complications 60.0% of the patients had Pulmonary Complications (60.0%) which was significantly higher than that of Local Wound Infection (40.0%) (Z=2.82; p<0.01). Pulmonary complication was higher in Indirect Decompression as compared to direct Decompression. Also, all the complication were with the patients with interval between injury and surgery>24 hours (p<0.001). There was no complication with the patients with interval between injury and surgery≤24 hours. Mahmoud Yousefifard, et al. [24] concluded that early spinal decompression surgery can improve neurologic recovery and is associated with less post-surgical complications. Jeffrey G. Chipman, et al. [26] concluded that early surgery was associated with fewer complications. The mean duration of hospital stay (mean ± S.D.) of the patients was 29.92±11.13 days with range 14 – 56 days and the median was 28 days. Most of the patients were discharged within 4 weeks (56.0%) (Z=2.06; p>0.05). Only 12.0% of the patients were discharged beyond 6 weeks. There no significant difference in mean duration of hospital stay of the patients undergoing posterior stabilization with direct decompression or posterior stabilization with indirect decompression. However the mean duration of hospital stay of the patients with interval between injury and surgery>24 hours was significantly higher than that of the patients with interval between injury and surgery≤24 hours (p<0.001).
Campagnolo, et al. [7] concluded that when spinal stabilization is indicated, its performance <24 hours after injury is associated with significantly fewer days in the hospital. Kerwin, et al. [27] concluded that patients with thoracic spine trauma and a spinal cord injury had the greatest benefit in reduction of morbidity, HLOS and ICULOS from early stabilization. Cengiz, et al. [22] concluded that early surgery may improve neurological recovery and decrease hospitalization time. Thomas M. Frangen, et al. [23] noticed shorter ventilator support, fewer pulmonary complications, shorter ICU, and hospital stays confirm a faster recovery of the early-operated patients. Marcel F. Dvorak, et al. [25] in their study concluded that early surgery reduces length of hospital stay.
However there are certain lacunae in this study like sample size of 25 patients is very less and follow up period of 6 months is less. But at the end of this study we are able to draw conclusion. However further studies with greater sample size and longer follow up that will help to prove the conclusions drawn from this study.
Conclusion
We conclude thoracolumbar spine injuries were more prevalent in the age group between 20 – 29 years in this study with male predominance. However, the mean age of the female patients was lower than that of male patients. Thus females were at risk of having thoracolumbar spine injuries at younger age than males. The commonest mode of injury was fall from a height. Management of thoracic and lumbar spine fractures requires careful pre- operative planning, patient selection, neurological evaluation and meticulous intra-operative care and post- operative rehabilitation including counseling for good functional outcome. Still, neurological recovery after thoracolumbar spinal injuries poses a challenge to orthopaedic surgeons.
Severity of the primary cord damage at the time of accident is a major factor in the neurological recovery of the patients. Earlier the intervention and less number of transfer of patients from place to place (less secondary neurological damage) gives good prognosis. The posterior midline approach provides adequate exposure and direct visualization. Most of injuries were at L1, followed by D12, L2 and D11 which were significantly higher than other.
Significant improvement was observed in ASIA score of the patients with direct decompression as compared to indirect decompression at discharge (p<0.05). Significant improvement was observed in ASIA score of the patients with direct decompression as compared to indirect decompression at subsequent follow-ups after discharge (p<0.05).
Pulmonary complication was higher in Indirect Decompression as compared to direct Decompression and there no significant difference in mean duration of hospital of the patients of the two types of surgeries. Significant improvement was observed in ASIA score of the patients with interval between injury and surgery≤24 hours as compared to interval between injury and surgery>24 hours at discharge (p<0.05). Significant improvement was observed in ASIA score of the patients with interval between injury and surgery>24 hours and ≤24 hours at subsequent follow-ups after discharge (p<0.05).The complication were with the patients with interval between injury and surgery>24 hours (p<0.001). There was no complication with the patients with interval between injury and surgery≤24 hours. The mean duration of hospital stay of the patients with interval between injury and surgery>24 hours was significantly higher than that of the patients with interval between injury and surgery≤24 hours (p<0.001). Thus in our opinion early surgery (≤24 hours) and posterior instrumentation with direct decompression is better than late surgery (>24 hours) and posterior instrumentation with indirect decompression.
References
- Riggins RS, Kraus JF (1977) The risk of neurologic damage with fractures of the vertebrae. J Trauma 17: 126-133.
- Benson DR, Keenen TL (1990) Evaluation and treatment of trauma to the vertebral column. Instr Course Lect 39: 577-589.
- Leventhal MR (2003) Fracture, Dislocations, and Fracture Dislocation of Spine. 10th ed. (Missouri CST, ed.). Mosby; 2003.
- G. The Treatment and Rehabilitation of Patients with Injuries of Spinal Cord.
- Charles M. Court-Brown, James D. Heckman, Margaret M. McQueen PTI. Rockwood and Green’s Fractures in Adults EIGHTh EDITION. 8th ed.
- Jacobs RR (1984) Surgical management of thoracolumbar spine injuries. Clin Orthop Relat Res 189: 22-34.
- Campagnolo D, Esquieres R, Kopacz K (1997) Effect of Timing of Stabilization on Length of Stay and Medical Complications Following Spinal Cord Injury. J Spinal Cord Med 20: 331-334.
- Thomson VM, Arun B AM (2004) Thoracolumbar vertebral fractures - A review of literature. J Orthop. 1: 4.
- Steffee AD, Biscup RS, Sitkowski DJ (1986) Segmental spine plates with pedicle screw fixation. A new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop Relat Res. 203: 45-53.
- Tumothy R, Crosswell TR, Marshall PD (1988) Mechanical stability of the AO internal spinal function system compared with that of Hartshill rectangle and sublaminar wiring in the management of the unstable burst fracture of the thoracic and lumbar spine. Spine J 23: 111-115.
- Alvine GF, Swain JM, Asher MA, Burton DC (2004) Treatment of thoracolumbar burst fractures with variable screw placement or Isola instrumentation and arthrodesis: case series and literature review. J Spinal Disord Tech 17: 251-264.
- Nasser R, Yadla S, Maltenfort MG, Harrrop JS, Anderson DG, et al. (2010) Complications in spine surgery. J Neurosurg Spine 13: 144-157.
- Sasso R, Renkens K, Hanson D, TR-CS, 2006 Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. journals.lww.com.
- Razak M, Mahmud M, Omar A, Mohktar SA (2000) Thoracolumbar fracture--dislocation results of surgical treatment. Med J Malaysia 55 Suppl C:14-7.
- Bourassa-Moreau É, Mac-Thiong JM, Li A, Feldman DE, et al. (2016) Do Patients with Complete Spinal Cord Injury Benefit from Early Surgical Decompression? Analysis of Neurological Improvement in a Prospective Cohort Study. J Neurotrauma 33: 301-306. doi:10.1089/neu.2015.3957
- McLain RF, Benson DR (1999) Urgent surgical stabilization of spinal fractures in polytrauma patients. Spine 24: 1646-1654.
- Wilson JR, Singh A, Craven C, Verrier MC, Drew B, et al. (2012) Early versus late surgery for traumatic spinal cord injury: the results of a prospective Canadian cohort study. Spinal Cord 50: 840-843. doi:10.1038/sc.2012.59
- Jun DS, Yu CH, Ahn BG (2011) Posterior Direct Decompression and Fusion of the Lower Thoracic and Lumbar Fractures with Neurological Deficit. Asian spine journa 5: 146-154.
- Zhang Z, Chen G, Sun J, Wang J, Yang H, et al. (2015) Posterior indirect reduction and pedicle screw fixation without laminectomy for Denis type B thoracolumbar burst fractures with incomplete neurologic deficit. J Orthop Surg Res 10: 85. doi:10.1186/s13018-015-0227-3
- Misra S, Sen S, Das S, Chatterjee A, Senguptha A, et al. Evaluation the results of surgical management of traumatic paraplegia in traumatic thoracolumbar fractures. Int J Res Med Sci 4: 2262-2270.
- Danisa OA, Shaffrey CI, Jane JA, Whitehill R, Wang GJ, et al. (1995) Surgical approaches for the correction of unstable thoracolumbar burst fractures: a retrospective analysis of treatment outcomes. J Neurosurg 83: 977-983. doi:10.3171/jns.1995.83.6.0977
- Cengiz ŞL, Kalkan E, Bayir A, Ilik K, Basefer A (2008) Timing of thoracolomber spine stabilization in trauma patients; impact on neurological outcome and clinical course. A real prospective (rct) randomized controlled study. Arch Orthop Trauma Surg 128: 959-966. doi:10.1007/s00402-007-0518-1
- Frangen TM, Ruppert S, Muhr G, Schinkel C (2010) The Beneficial Effects of Early Stabilization of Thoracic Spine Fractures Depend on Trauma Severity. J Trauma Inj Infect Crit Care 68: 1208-1212. doi:10.1097/TA.0b013e3181a0e558
- Yousefifard M, Rahimi-Movaghar V, Baikpour M, Ghelichkhaniet P, Hosseini M, et al. (2017) Early versus late spinal decompression surgery in treatment of traumatic spinal cord injuries; a systematic review and meta-analysis. Emerg (Tehran, Iran) 5: e37.
- Dvorak MF, Noonan VK, Fallah N, Fisher CG, Finkelstein J, et al. (2015) The Influence of Time from Injury to Surgery on Motor Recovery and Length of Hospital Stay in Acute Traumatic Spinal Cord Injury: An Observational Canadian Cohort Study. J Neurotrauma. 32: 645-654. doi:10.1089/neu.2014.3632
- Chipman JG, Deuser WE, Beilman GJ (2004) Early Surgery for Thoracolumbar Spine Injuries Decreases Complications. J Trauma Inj Infect Crit Care 56: 52-57. doi:10.1097/01.TA.0000108630.34225.85
- Kerwin AJ, Frykberg ER, Schinco MA, Griffen MM, Murphy T, et al. (2005) The effect of early spine fixation on non-neurologic outcome. J Trauma 58: 15-21.