Evaluating the Effectiveness of Ketamine Plus Atropin as Anesthesia for Intrathecal Chemotherapy and Bone Marrow Procedure at Hue Central Hospital, Vietnam
Pham Nhu Hiep1, Tran Kiem Hao2, Nguyen Thi Kim Hoa2*, Phan Canh Duy1,Chau Van Ha2, Nguyen Huu Son2
1Adult Oncology Center, Hue Central Hospital, Vietnam
2Pediatric Center, Hue Central Hospital, Vietnam
Received Date: 19 July, 209; Accepted Date: 24 July, 2019; Published Date: 02 August, 2019
*Corresponding author: Nguyen Thi Kim Hoa, Pediatric Center, Hue Central Hospital, 16 Le Loi Street, Hue city, Vietnam. Email: kimhoa.fmi@gmail.com
Citation: Hiep PN, Hao TK, Hoa NTK, Duy PC, Ha CV, Son NH (2019) Evaluating the Effectiveness of Ketamine Plus Atropin as Anesthesia for Intrathecal Chemotherapy and Bone Marrow Procedure at Hue Central Hospital, Vietnam. Jr surg opetech anesthesia: JSOPA-108
Abstract
Background: Ketamine is a phencyclidine and cyclohexamine derivative. Ketamine and atropine have increasingly been used in recent years as an effective form of deep sedation/anaesthesia in children in developed countries, but not in developing countries like Vietnam.
Objective: This pioneer trial aimed to evaluate the effectiveness of using ketamine plus atropine as anaesthetic agents for paediatric oncology procedures. From this study, we establish a protocol for anaesthesia in paediatric oncology procedures.
Methods: A descriptive and prospective study on 223 paediatric patients of both sexes (129 males and 94 females) aged 7.2 months to 15 years (mean age: 4.0 ± 3.4 years) and with body weight between 6.5 to 55 kg (mean weight: 15.3 ± 6.2 kg) was carried out from January 2015 to June 2019. The patients had been diagnosed acute leukaemia, lymphoma or solid tumor. They underwent intrathecal chemotherapy and bone marrow aspirations or bone marrow biopsy for diagnostic as well as therapeutic purposes. After obtaining informed consent from their parents, the research was performed. Datas were analysed by Medcalc software.
Results: The total number of procedures was 810. Bone marrow aspiration was performed 402 times, bone marrow biopsy was done 30 times and intrathecal chemotherapy given 378 times. All procedures were successfully completed. The mean dose of ketamine and atropine used 1.55 ± 0.31 mg/kg and 0.100 ± 0.029 mg respectively. The recovery time was 9.2 ± 7.3minutes. Only 0.12% experienced apnoea; 1.2% muscular hypertonicity; 4.3% nystagmus, and hyperactivity; 3.7% hypersalivation, 2.5% hallucination and 5.5% vomiting; none of the patients had laryngospasm or transient rash. All of the patients’ parents were satisfied with the use of anaesthetics.
Conclusions: This is a pioneer trial for children in Vietnam. 1.5 mg/kg intravenous ketamine and 0.1 mg atropine were found to be effective and suitable dose in children requiring deep sedation for painful procedures and produce only minimal side effects. We established a protocol with the above doses and continue to apply this in order to reduce pain, trauma, and complications and to practice safely.
Keywords: Anesthesia; Atropine; Children; Ketamine
Introduction
Ketamine is a phencyclidine and cyclohexamine derivative. It is unique among the sedative analgesics in producing disociative state between the thalamus and the limbic system which is is characterized by four features: sedation, analgesia, ammesia and catalepsy. Ketamine does not lead to loss of protective reflexes. In developed countries, Ketamine and atropine has been increasingly used in recent years as an effective form of deep sedation, anesthesia in children.
In Vietnam, children with blood diseases, especially children with cancer are often carried out painful procedures such as bone marrow aspiration/biopsy, intrathecal chemotherapy for diagnosis and treatment. Therefore, using sedative analgesics limit the pain and fear for patients is necessary, minimize the trauma for the children. However, to our knowledge there is no established anesthetic protocol yet.
So, we conducted a study using the combination of ketamine and atropine at Pediatric Hematology-oncology Department - Hue Central Hospital with purposes: [1]. To evaluate the effectiveness and safety of using ketamine combination with atropine as sedative analgesics in painful procedures in children [2]. To recommend anesthetic protocol appling for pediatric patients.
Patients and Method
Patients
223 patients admitted Hue Pediatric Center, Hue Central Hospital, Vietnam from 1/2015 to 6/2019, in which there were 129 boys and 94 girls. The exclusive criteria: Age less than 3 months; Active pulmonary infection; History of airway instability, tracheal surgery or tracheal stenosis; Cardiovascular disease in which raised BP or HR may be deleterious (eg. angina, heart failure, aneurysm or uncontrolled hypertension); Adverse reactions to ketamine; Raised intracranial pressure; Glaucoma; Psychiatric illness; Full meal within 3 hours of administration.
Method
A prospective and descriptive study (Figure 1) is the protocol for using anesthesia. The present study was approved by the Hue Central Hospital Review Board and conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. Statistical analysis: Data were analyzed using Medical program.
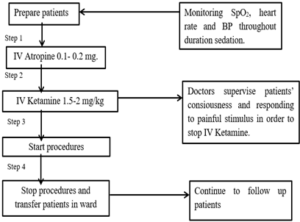
Figure 1: Protocol for using anesthesia.
Results
Two hundred and twenty-three patients were enrolled to the study, of these there were 129 boys and 94 girls, the ratio of male/female = 1.38/1.Theage ranged between 7.2 months to 15 years, mean age was4.0 ± 3.4 years, and body weight ranged 6.5 to 55 kg (mean weight: 15.3 ± 6.2 kg).
The total numbers of procedures performed were 810, in which there were 402 times of bone marrow aspirations, 30 times of bone marrow biopsy 378 times of intrathecal chemotherapy (302 times: 1 drug and 75 times: 3 drugs).The mean dose of ketamin was 1.55 ± 0.31mg (range 1.0 – 2.2 mg) and the mean dose of atropine was 0.100 ± 0.029 mg (range 0.10 - 0.32 mg).
The recovery time was 9.2 ± 7.3 minutes (range 1-40 mins) and mean duration of the procedure was 8.0 ± 1.5 minutes (range 6-15 mins).
There wasn’t any difference about Sp02 saturation before and after using anethesia (p=0.12). Heart rate and blood pressure before and after using anesthesia were the same too (Table 1). Side effects after using drug were seen in one patient with apnea (0.12%), 3.7% hypersalivation and 5.5% vomiting. There was 10 times (1.2%) that patients experienced muscular hypertonicity. Hallucination happened in 2.5% patients (Table 2). There was 4.3% nystagmus and hyperactivity.99.8% procedures were done, except one patient appeared apnea, so we had to cancel to conduct procedure.100% parents were satisfied when their childrens were used sedative analgesics during the procedures.
The average value before IV
The average value after IV
P
The mean Sp02 (%)
97.5 ± 1.8
97.0 ± 3.6
0.12
The mean heart rate (beats/min)
121.1 ± 22.6
121.7 ± 24.1
0.56
The mean systolic blood pressure (mmHg)
89.7 ± 6.7
90.3 ± 8.3
0.1
The mean diastolic blood pressure (mmHg)
58.5 ± 10.7
57.6 ± 11.2
0.83
Variables
Quantity
%
Apnea
1
0.12
Hypersalivation
30
3.7
Vomiting
45
5.5
Muscular hypertonicity
10
1.2
Hallucination
20
2.5
Discussion
In our study, the ratio of male/female was 1.38/1. According to Kidd, Ng KC and Heinz, the ratio was higher: 1.75/1, 1.9/1 and 1/9/1 respectively [1, 3]. The mean age was 4.0 ± 3.4 years, and body weight ranged 6.5 to 55 kg (mean weight: 15.3 ± 6.2 kg). Similarly, Traivaree chosed 46 children aged 6 months to 15 years [4]. According to Kidd and Heinz, they chosed anesthesia with bigger child, age ranged between 14 months to 15 years, 13 months to 14.5 years respectively [1, 3].
The mean dose of ketamin was 1.55 ± 0.31mg which was the same dose in Heilbrunn and Evans’ research [5, 6]. Similarly, Heinz, Mason used a little bit higher dose of Ketamine (2mg/kg) than our dose [3, 7]. Contrast to us, Traivaree used lower dose of Ketamine (1mg/kg) and it was effective for invasive procedures in children with malignancy [4]. So, through many researches, with the dose of intravenous ketamineup to 2 mg/kg is an effective sedative for oncology procedures [3, 5-7]. And our mean dose of atropine was 0.100 ± 0.029 mg. Similarly, Heinz, Yu Chan Kye showed the minimum dose of atropin was 0.1 mg; the usual dose of atropine was 0.01 mg/kg [3, 8].
The recovery time was 9.2 ± 7.3 minutes and mean duration of the procedure was 8.0 ± 1.5 minutes. Similarly, Evans showed the mean duration of the procedure was 6.6 mins and the recovery time was 11 mins [6]. Heinz showed the mean time of the procedure was 10.5 minutes [3].
(Table 1) showed there wasn’t any difference about Sp02 saturation before and after using anethesia (p=0.12), except one patient appeared apnea then he recovered with supporting stimulation and providing oxygen. Similarly, in Slonim’s research, one patient had oxygen desaturation < 90% [9]; in Brown’result, transient airway complication occurred in 3.2% with just one (brief desaturation) felt [10]. (Table 1) also showed heart rate and blood pressure before and after using anesthesia were the same too. According to Patterson, Ketamine caused modest increase in systolic pressure, diastolic blood pressure and heart rate [11].
When using Ketamine and atropine, our patients experienced some side effects. There was one patient having apnea. This was the first case we used sedation, we didn’t have experience, we gave intravenously ketamine too quickly, so the patient had apnea. Contrast to us, Evans showed no major airway complications occurred [6].
Our patients experienced 3.7% hypersalivation. Similarly, Yu Chan Kye showed hypersalivation occurred in 1.5% respectively [8]. Jiaxiao Shi showed the group receiving atropine had reduced hypersalivation [12]. According to Heinz and Traivaree, the rate of hyper salivation was higher: 11.4 % and 26.1% respectively [3, 4]. Vomiting happened in 5.5% patients, which was higher comparing with Yu ChanKye: 4.4% [8]. Contrast to us, Heinz showed higher percentage patients with vomiting 9.1% [3].
In our study, there wasn’t any patients had laryngospasm or transient rash. Similarly, Sheikh didn’t see any side effects of laryngospasm or transient rash. Contrast to us, Heinz experienced 22.7% rash and 9.1% laryngospasm [3].There were 10 times (1.2%) that patients experienced muscular hypertonicity and recovered without treatment. This was a reason that some protocols combined midazolam with ketamine and atropine. Hallucination happened in 2.5% patients. Similarly, Travivaree showed hallucination appeared in 4.2% [4]. Nystagmus and hyperactivity were dued to ketamine‘s side effects, with rate 4.3%. Contrast to us, the ratio of hyperactivity in Heinz’s study was 20.5% [3].
Ketamine causes dissociation between the thalamocortical pathways and limbic systems. After using ketamine and atropine, patients didn’t cry or struggle, didn’t feel painful. So, taking bone marrow was easier. There wasn’t any state that the doctors didn’t take enough marrow to do tests and the anesthetic helped doctors to avoid trauma for patients when the doctor did intrathecal chemotherapy procedures, and it helped to limit blast cells infiltrated the central nervous system, reduced the patient’ stress. Similarly to Mason, all procedures (solid organ biopsies) were successfully completed, and there were no major adverse events [7].
In our study, 100% parents were satisfied when their childrens were used sedative analgesics during the procedures, so the children weren’t afraid and didn’t feel painful.According to Heinz, the satisfaction rating with excellent, good, satisfactory and poor were 74.4%, 18.6%, 2.3% and 4.7% respectively [3].
Conclusion
This is a pioneer trial for children in Vietnam. Ketamine combined Atropine were found effective and suitable in children requiring deep sedation for painful procedures. With 1.5mg/kg intravenous ketamine and minimum dose of atropine were found effective. Ketamine was tolerated well. The recovery time was short: 9.2 ± 7.3 minutes. Only 0.12% of our procedures experienced apnea; 1.2% muscular hypertonicity, 4.3% nystagmus, hyperactivity; 3.7% hypersalivation, 2.5% dream; 5.5% vomiting; none of the patients had laryngospasm or transient rash. And 100% their parents were satisfied with the use of anesthetics. Thereby, we establish protocol with the above doses and continue to apply this in order to reduce pain, trauma, and complications and to practice safely.
Funding: No funding or grant support was received for this work.
Authorship: All authors attest that they meet the current ICMJE criteria for authorship.
Conflict of Interest: The following authors have no financial disclosures.
Acknowledgments: The authors are grateful to Prof. Pham Nhu Hiep- director of Hue Central Hospital; physicians, administrative staff at Pediatric Center and Adult oncology Center of Hue Central Hospital for allowing us to undertake this research.
References
- Kidd LR, Lyons SC, Lloyd G (2016) Paediatric procedural sedation using ketamine in a UK emergency department: a 7 year review of practice. Br J Anaesth 116: 518-23.
- Ng KC, Ang SY (2002) Sedation with ketamine for paediatric procedures in the emergency department--a review of 500 cases. Singapore Med J 43: 300-304.
- Heinz P, Geelhoed GC, Wee C, Pascoe EM (2006) Is atropine needed with ketamine sedation? A prospective, randomised, double blind study. Emerg Med J 23: 206-209.
- Traivaree C, Jindakam W, Monsereenusorn C, Rujkijyanont P, Lumkul R (2014) The factors of ketamine that affect sedation in children with oncology procedures: parent satisfaction perspective. J Med Assoc Thai 2: S19-24.
- Heilbrunn BR, Chang TP, Liu DR (2015) A retrospective comparison of ketamine dosing regimens for pediatric procedural sedation. Eur J Emerg Med 22: 111-116.
- Evans D, Turnham L, Barbour K, Kobe J, Wilson L, el al (2005) Intravenous ketamine sedation for painful oncology procedures. Paediatr Anaesth 15: 131-138.
- Mason KP, Padua H, Fontaine PJ, Zurakowski D (2009) Radiologist-supervised ketamine sedation for solid organ biopsies in children and adolescents. AJR Am J Roentgenol 192: 1261-1265.
- Kye YC, Rhee JE, Kim K, Kim T, Jo YH, el al (2012) Clinical effects of adjunctive atropine during ketamine sedation in pediatric emergency patients. Am J Emerg Med 30: 1981-1985.
- Slonim AD, Ognibene FP (1998) Sedation for pediatric procedures, using ketamine and midazolam, in a primarily adult intensive care unit: a retrospective evaluation. Crit Care Med 26: 1900-1904.
- Brown L, Christian-Kopp S, Sherwin TS, Khan A, Barcega B, el al (2008) Adjunctive atropine is unnecessary during ketamine sedation in children. Acad Emerg Med 15: 314-318.
- Patterson AC, Wadia SA, Lorenz DJ, Stevenson MD (2017) Changes in blood pressure and heart rate during sedation with ketamine in the pediatric ED. Am J Emerg Med 35: 322-325.
- Shi J, Li A, Wei Z, Liu Y, Xing C, el al (2018) Ketamine versus ketamine pluses atropine for pediatric sedation: A meta-analysis. Am J Emerg Med 36: 1280-1286.
