Publication Information
ISSN 2691-8803
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2019
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Euthanasia in Organ Donation Can Be Avoided through Coordination Dynamics Therapy
Giselher Schalow*
NGOMR: Non-Government-Organized-Medical-Research
Received Date: September 22, 2021; Accepted Date: September 27, 2021; Published Date: October 04, 2021;
*Corresponding author: Giselher Schalow, NGOMR: Non-Government-Organized-Medical-Research. Email: g_schalow@hotmail.com
Citation: Schalow G (2021) Euthanasia in organ donation can be avoided through Coordination dynamics therapy. Adv Pub Health Com Trop Med: APCTM-132.
DOI: 10.37722/APHCTM.2021304
Summary
With four case reports it is shown that in very severe brain injury substantial brain repair can be achieved through Coordination Dynamics Therapy (CDT). With efficient long-lasting therapy at least some brain-injured patients would not drift into brain death. But with inefficient or no treatment they would drift into brain death and could be used as organ donors. The real possibility exists that physicians are not fighting for the survival of the severely brain injured patients, but let the patient die and use then the organs. The in mass-media reported case that one day before organ donation the ‘dead’ patient recovered from coma spontaneously is no unique case. In case report one, the 22-years-old traumatic brain-injured patient Manolis recovered fully from permanent coma through 5 years of CDT, relearned to speak with 6 years of CDT and central nervous system (CNS) functions steadily improved further with 7.5 years of CDT. In case report two, the brain-injured patient Fovios had the chance to recover spontaneously from coma because the parents refused organ donation. 16 years later his mental and movement functions improved quickly through CDT. In case report three, it is shown that even the breathing center, damaged in brain death, can be repaired through CDT. In case report four, it is shown that CNS functions, including hand function, could be improved substantially in the 12-year-old Alen through 6 weeks of CDT, even though persistent hemiplegia was diagnosed. A comparison with Hitler Germany shows that money and lack of knowledge are the main reasons for euthanasia. A change from the “opt in” (only those who have given explicit consent are donors) to the “opt out” voluntary consent (anyone who has not refused consent to donate is a donor) would increase euthanasia.
Keywords: Coordination dynamics therapy; Electrophysiology; Euthanasia; Human repair-neurophysiology; Organ donation; Oscillatory firing; Phase and frequency coordination; Single-nerve fiber action potentials; Surface EMG
Introduction
Euthanasia
The motivation for writing this article is a report in a Swiss newspaper concerning Euthanasia (Figure 1). A young man should be used for organ transplantation and when the sister wanted to say goodbye to him before the organs were supposed to be removed next day, the ‘dead’ brother woke up. If the physicians would have removed the organs, they would have murdered this patient.
 Figure 1: Shortly before organ donation the ‘dead Lewis’ woke up.
Figure 1: Shortly before organ donation the ‘dead Lewis’ woke up.
Most organ donations for transplantation are done in the setting of brain death. Brain death may result in legal death, but still with the heart beating and with mechanical ventilation, keeping all other vital organs alive and functional for a certain period of time. Given long enough, patients who do not fully die in the complete biological sense, but who are declared brain dead, will usually start to build up toxins and wastes in the body. In this way, the organs can eventually dysfunction due to coagulopathy, fluid or electrolyte and nutrient imbalances, or even fail. Thus, the organs will usually only be sustainable and viable for acceptable use up until a certain length of time. This may depend on factors such as how well the patient is maintained, any comorbidities, the skill of the healthcare teams and the quality their facilities. The decision of brain death is nowadays safe.
The problem with organ donation occurs bevor brain death, namely due to inefficient repair treatment administered to the patient with a severely damaged brain. With inefficient treatment, the pathologic processes win slowly against the innate physiologic processes and the patient becomes brain dead. Through efficient and intensive coordination dynamics therapy (CDT), the damaged brain can partly be repaired and the patient may not suffer brain death on the long term (case report 1, Manolis).
Euthanasia is an old problem and was practiced already in ancient Greece. To handle the problem carefully, expert knowledge has to be used. But the usage of knowledge and logic can also be dangerous as Socrates experienced (Figure 2).
 Figure 2: The Death of Socrates, by Jacques-louis David (1787), depicting Socrates prepared to drink hemlock, following his conviction for corrupting the youth of Athens.
Figure 2: The Death of Socrates, by Jacques-louis David (1787), depicting Socrates prepared to drink hemlock, following his conviction for corrupting the youth of Athens.
Euthanasia can be categorized in different ways, which include voluntary, non-voluntary, or involuntary:
- Voluntary euthanasia is legal in a growing number of countries.
- Non-voluntary euthanasia (patient’s consent unavailable) is legal in some countries under certain limited conditions, in both active and passive forms.
- Involuntary euthanasia (without asking consent or against the patient’s will) is illegal in all countries and is usually considered murder.
Euthanasia is considered here with respect to patients with very severe brain injuries and being in coma.
In Hitler-Germany there were different places where disabled were killed or horrible experiments performed (Figure 3). Probably there were also other places in the world, as for example Canada (children), were patients or healthy were murdered.
 Figure 3: Places in Germany between 1939 and 1945, where different kinds of euthanasia were performed.
Figure 3: Places in Germany between 1939 and 1945, where different kinds of euthanasia were performed.
Human repair-neurophysiology to avoid euthanasia?
For repairing the human nervous system, human anatomy, human neurophysiology and repair strategies of the human nervous system are needed. Repairing the CNS of human patients is also research on human, especially when based on theory, because the CNS repair data from severely injured patients can be used for the repair of slightly CNS-injured patients.
In mainstream medicine, with respect to organ transplantation, there seems to be that much interest in organs that involuntary euthanasia it performed (Figure 1). Not much treatment effort is taken to repair the very severely injured CNS of patients, but let them drift into brain death to obtain the organs. And sometimes organs are even removed before the patient is brain-dead.
The mildly injured CNS can repair itself spontaneously. The severely injured one needs real therapy for substantial functional recovery. But the very severely injured CNS cannot help itself anymore and drifts into direction of brain death, unless efficient long-lasting therapy is administered. Without repair effort, the severely brain-injured patient is soon ready for organ donation. If the relations of the patient cannot deny organ donation, there will be more organs available and money can be earned.
On an international conference on the repair of pediatric acquired brain injury, there was absolutely no interest to get informed about or to try out the special CDT device (Figure 4). Scientific publications are ignored and participants at conferences do avoid to get informed. A real CNS repair is not of interest to mainstream medicine. The new development to repair the injured human CNS is hushed up.

Figure 4: Poster of the Author Schalow G (Number 38) at the international conference IPBIS2018 in Belfast 2018: Pediatric acquired brain injury repair. The poster is not especially good because of lack of money. But the repair progress of the nervous system in children can clearly be seen. It is also shown that human anatomy and physiology is needed for repair.
Figure 5 shows some principles of human repair-neurophysiology. By measuring the impulse traffic running in and out of the CNS and analyzing CNS functioning under physiologic and pathologic conditions, the movement-based learning therapy CDT was developed and applied to patients. Figure 5C was taken from the very good anatomy book ‘Pernkopf’. Probably the anatomist Pernkopf was related to involuntary euthanasia in Hitler-Germany and was in prison, were he finished his high-quality anatomy books.
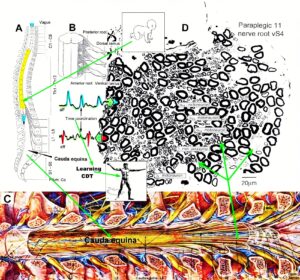
Figure 5: Principle of human neuroscience research to repair the human nervous system. It starts with humans. A. schematic anatomy of the spinal canal with the spinal cord, nerve roots (B) and cauda equina nerve roots due to the Ascensus of the spinal cord. C. Painting of the spinal canal with the cauda equina nerve roots, taken from Pernkopf (‘Topographische Anatomie des Menschen’, University Library Turku, Finland). In reality, the caudal sacral nerve roots are much thinner than pictured. D. A real cross-section of the ventral sacral root S4. Single-nerve fiber action potentials, conducted into (aff) and out of the CNS (eff) for communication of the CNS with the outside world, are inserted. Out of the difference of the impulse patterns, under physiologic and pathologic conditions, a movement-based learning therapy was developed (CDT) with which patients can get their CNS repaired and leave the wheelchair behind.
It was shown that Coordination Dynamics Therapy (CDT) can improve or repair central nervous system (CNS) functioning after stroke [1], traumatic brain injury [2, 3], spinal cord injury (SCI) [4-8], cerebellar injury [9, 10], cerebral palsy [11], hypoxic brain injury [12], in Parkinson’s disease [13], spina bifida (myelomeningocele) [14] and scoliosis [15]. Speech had been induced and improved in a patient with severe cerebral palsy [16]. A permanent coma patient could be brought out-of-coma and relearned to speak [17]. Cancer grows could be inhibited through CDT [18, 19]. Cardio-vascular performance could be improved. There is indication that the general health can be improved via CDT to live longer with a better quality of life for 10 to 20 years [20], including patients with very severely injured CNS.
In this report, it will be shown that, based on human repair-neurophysiology, very severe brain injuries can partly be repaired. With respect to the repair of the CNS, mainstream medicine is something like 30 years out-of-date. Too much money is wasted in inefficient treatments. Human repair-neurophysiology is not organized and real expert knowledge is not of interest to the society. Medical faculties of universities are not trying to get up to date for teaching and medical research. Movement-based learning is besides drug therapy and operations a third leg of medicine. Since the nervous system is involved in nearly all body functions, an improvement of nervous system functioning will improve health in general.
In the Method, the human-science-based CDT is shortly introduced and in the Results the repair of the severely and extreme severely injured CNS of patients is displayed to show that the very severely injured CNS can partly be repaired and often brain death avoided. Treatment priority should first be given to the injured patient. And if efficient long-lasting treatment is unsuccessful, only then physicians/therapists should think of organ donation and not just waiting for the brain death to remove the organs.
Method
Anatomy
The real new step in human repair-neurophysiology is the development of a new recording technique, the single-nerve fiber action potential recording method in human. Hodgkin and Huxley used the special anatomy of the squid giant axon (up to 1mm in diameter) to clarify the excitation of nerve fibers [21]. The Author used the Ascensus of the human spinal cord which give rise to long nerve roots. The thin long sacral roots are ideal to record single-nerve fiber action potentials in human under rather physiologic conditions to explore the functioning of the human central nervous system (CNS).
Figure 6 shows the opened spinal canal with its nerve roots and the dura in place, taken from the anatomy book “Pernkopf”. When removing the dura and pia mater, the long nerve roots become visible (Figure 5C).
Real cauda equina nerve roots can be seen in a dissection from the Author (Figure 7C). Even thin long lower sacral nerve roots can be seen. The cross section of a ventral S4 root is shown in Figure 5D.
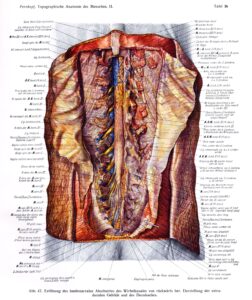 Figure 6: Opened lumbo-sacral spinal canal, from Pernkopf (‘Topographische Anatomie des Menschen’, University Library Turku, Finland).
Figure 6: Opened lumbo-sacral spinal canal, from Pernkopf (‘Topographische Anatomie des Menschen’, University Library Turku, Finland).
Human Neurophysiology
With the single-nerve fiber action potential recording method, single-nerve fiber action potentials can be recorded from sacral nerve roots, running in and out of the spinal cord (Figure 7) [22].
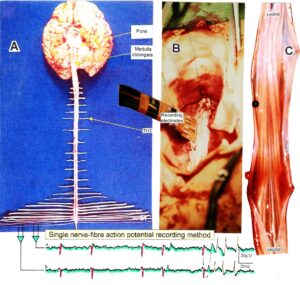 Figure 7: Layout of the recording of single-nerve fiber action potentials to analyze the self-organization of neuronal networks of the human CNS under physiologic and pathophysiologic conditions. A, B, C. By recording with two pairs of platinum wire electrodes (B) from sacral nerve roots (cauda equina, C) containing between 200 and 500 myelinated nerve fibers, records were obtained in which single nerve-fiber action potentials (APs) were identified from motoneurons (main AP phase downwards) and afferents (main AP phase upwards). A. Human CNS with the schematic illustration of the recording layout and an original record of single nerve-fiber action potentials. Note the time calibration of 2ms. B. Intraoperative recording layout (when implanting a bladder stimulator) with two pairs of wire electrodes and one temperature sensor. A thin nerve root is positioned over the platinum wire electrodes. C. Dissection of the human cauda equina. At the caudal end, the filum terminalia and thin nerve roots can be seen. Dissections of the Author apart from the laminectomy in B.
Figure 7: Layout of the recording of single-nerve fiber action potentials to analyze the self-organization of neuronal networks of the human CNS under physiologic and pathophysiologic conditions. A, B, C. By recording with two pairs of platinum wire electrodes (B) from sacral nerve roots (cauda equina, C) containing between 200 and 500 myelinated nerve fibers, records were obtained in which single nerve-fiber action potentials (APs) were identified from motoneurons (main AP phase downwards) and afferents (main AP phase upwards). A. Human CNS with the schematic illustration of the recording layout and an original record of single nerve-fiber action potentials. Note the time calibration of 2ms. B. Intraoperative recording layout (when implanting a bladder stimulator) with two pairs of wire electrodes and one temperature sensor. A thin nerve root is positioned over the platinum wire electrodes. C. Dissection of the human cauda equina. At the caudal end, the filum terminalia and thin nerve roots can be seen. Dissections of the Author apart from the laminectomy in B.
By measuring the conduction times and with the known electrode pair distance of 10 mm, conduction velocity distribution histograms were constructed in which the myelinated nerve fiber groups larger than 4mm could be characterized by group conduction velocity values (Figure 8). After the recording, morphometry was performed. Distributions of nerve fiber diameters were constructed and nerve fiber groups were characterized by the peak values of asymmetrical distributions (Figure 8). By correlating the peak values of the conduction velocity distributions with those of the diameter distributions, obtained for the same root (Figure 8), a classification scheme was constructed of the human peripheral nervous system (Figure 9) [23, 24]; the only existing one for human peripheral nerve fibers.
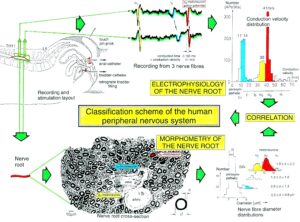
Figure 8: Development of a classification scheme for human peripheral nerve fibers. Conduction velocities (V) and nerve fiber diameters (Æ) of afferent (from receptors) and efferent (motor) nerve fiber groups in normal humans and in patients with a traumatic SCI for 0.5 to 6 years.
This classification and identification scheme represents a solid basis for classifying and identifying nerve fiber groups in the human peripheral nervous system (PNS) and analyzing CNS functions at the single-neuron level. It became thus possible to record natural impulse patterns simultaneously from identified single-afferent and efferent nerve fibers and to analyze self-organizing mechanisms of the human CNS under physiologic and pathologic conditions.

Figure 9: Classification scheme for human peripheral nerve fibers. Conduction velocities (V) and nerve fiber diameters (Æ) of afferent and efferent nerve fiber groups in normal humans and in patients with a traumatic spinal cord injury for 0.5 to 6 years. The splitting of the a1-motoneurons into the 3 subgroups, a11, a12, a13, has not yet been confirmed. This is the only existing classification scheme for human peripheral nerve fibers!
The most important finding with the single-nerve fiber action potential recording method was that nerve cells in the human CNS are organizing themselves through “Phase and Frequency coordination” [25, 26] (Figure 10). In nerve fibers, this phase and frequency coordination can easily be measured, because the three motoneuron types fire for high activation oscillatory [27] and offer in this way a structure to which the timed firing of neurons can be related to. Since the α2-motoneuron oscillations are most stable, firing phases of neurons can be related best to the α2-motoneuron firings.
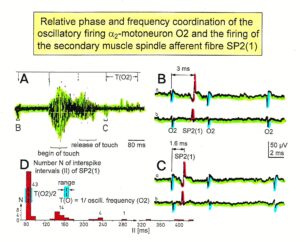 Figure 10: Time relation between the occurrence of the action potentials (APs) of the oscillatory firing a2-motoneuron O2 and the firing of the secondary muscle spindle afferent fiber SP2(1). Brain-dead human HT6. S4 dorsal root recording. A. Overall view of the used sweep piece; only trace “a” shown. Four oscillation cycle periods of the motoneuron O2 are indicated (T(O2)). The APs of the impulse trains can be recognized only partly, because of the slow time base and poor digitalization. One impulse train (dashed arrow) is lost in the touch stimulated activity, which consists of a touch (large overall activity) and a release part (lower overall amplitude). B, C. Sweep pieces from A, time stretched. In B, motoneuron impulse train APs are marked O2, spindle afferent APs are marked SP2(1). Note that the APs of the spindle afferent fiber are not time-locked to the first AP of the impulse train of the rhythmically firing motoneuron (relative phase coordination). D. Occurrence of interspike intervals of the secondary muscle spindle afferent fiber SP2(1). The numbers give the amount of IIs in each distribution peak. The oscillation period of motoneuron O2 (and the range of variation) and the half period are indicated by short dashed lines. Note that the IIs of fiber SP2(1) are very similar to the oscillation period (or the half of it) of a2-motoneuron O2 (relative frequency coordination).
Figure 10: Time relation between the occurrence of the action potentials (APs) of the oscillatory firing a2-motoneuron O2 and the firing of the secondary muscle spindle afferent fiber SP2(1). Brain-dead human HT6. S4 dorsal root recording. A. Overall view of the used sweep piece; only trace “a” shown. Four oscillation cycle periods of the motoneuron O2 are indicated (T(O2)). The APs of the impulse trains can be recognized only partly, because of the slow time base and poor digitalization. One impulse train (dashed arrow) is lost in the touch stimulated activity, which consists of a touch (large overall activity) and a release part (lower overall amplitude). B, C. Sweep pieces from A, time stretched. In B, motoneuron impulse train APs are marked O2, spindle afferent APs are marked SP2(1). Note that the APs of the spindle afferent fiber are not time-locked to the first AP of the impulse train of the rhythmically firing motoneuron (relative phase coordination). D. Occurrence of interspike intervals of the secondary muscle spindle afferent fiber SP2(1). The numbers give the amount of IIs in each distribution peak. The oscillation period of motoneuron O2 (and the range of variation) and the half period are indicated by short dashed lines. Note that the IIs of fiber SP2(1) are very similar to the oscillation period (or the half of it) of a2-motoneuron O2 (relative frequency coordination).
Figure 11 shows schematically the oscillatory firing patterns of the three kinds of motoneurons and the muscle fiber types they innervate.
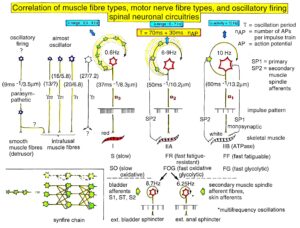 Figure 11: Correlation of muscle fiber types, motor nerve fiber types, and oscillatory firing spinal neuronal networks (oscillators), based on histochemical, morphological and neurophysiological properties. This figure provides a simplified correlation between muscle fiber, motoneuron and sacral oscillator types. No additional subtypes have been included. The existence of a1-motoneuron (FF) oscillators firing at 10 Hz has been predicted and they have been identified in paraplegics. a = motoneuron, g1, g2 = dynamic and static fusimotors, parasympathetic = parasympathetic preganglionic motoneuron. S1, ST, S2 = stretch, tension and flow receptor afferents.
Figure 11: Correlation of muscle fiber types, motor nerve fiber types, and oscillatory firing spinal neuronal networks (oscillators), based on histochemical, morphological and neurophysiological properties. This figure provides a simplified correlation between muscle fiber, motoneuron and sacral oscillator types. No additional subtypes have been included. The existence of a1-motoneuron (FF) oscillators firing at 10 Hz has been predicted and they have been identified in paraplegics. a = motoneuron, g1, g2 = dynamic and static fusimotors, parasympathetic = parasympathetic preganglionic motoneuron. S1, ST, S2 = stretch, tension and flow receptor afferents.
By comparing CNS functioning in brain-dead humans (where the spinal cord is functioning rather physiologically) and patients with spinal cord injury, injury-induced changes of CNS functioning can be measured and partly repaired. Mainly the phase and frequency coordination of neuron firing becomes impaired following injury. This impaired coordination among neuron firings can efficiently be repaired through exercising on the special CDT device (Figures 4, 19A, 20E).
The drawing back of the single-nerve fiber action potential recording method is that it is an invasive recording method. But with the surface electromyography (sEMG) [28] one can record non-invasively coordinated firing among motoneurons via their motor units if one records from suitable patients, like incomplete spinal cord injury patients, when a certain muscle is only innervated by a few motoneurons.
In Figure 12, the recordings from motoneurons and motor units are compared. The firing patterns of α1, α2 and α3-motoneurons can easily recorded with the single-nerve fiber action potential recording method but not with the sEMG (Figure 12). From spinal cord injury patients, on the other hand, single-motor unit APs can be easily recorded from α1 motor units but not from α2 and α3 motor units (Figure 12), because their AP amplitude seems to be too small. Clinical sEMG recordings therefore show mainly the activity of α1 motor units. The generation of motor patterns of α1-motoneuron firings with increasing load and the phase and frequency coordination among single-motor unit firings can be recorded with sEMG (Figure 13).
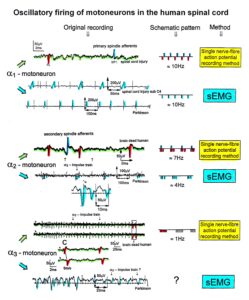 Figure 12: Oscillatory firing patterns of a1, a2, and a3-motoneurons recorded from motoneuron axons with the single-nerve fiber action potential recording method and by surface electromyography (sEMG) from FF, FR, and S-type motor units. The left panel shows original recordings, the middle panel the schematic patterns; the recording methods are indicated on the right side. The recordings were taken from patients with spinal cord injury and Parkinson’s disease and from brain-dead humans.
Figure 12: Oscillatory firing patterns of a1, a2, and a3-motoneurons recorded from motoneuron axons with the single-nerve fiber action potential recording method and by surface electromyography (sEMG) from FF, FR, and S-type motor units. The left panel shows original recordings, the middle panel the schematic patterns; the recording methods are indicated on the right side. The recordings were taken from patients with spinal cord injury and Parkinson’s disease and from brain-dead humans.
The neural networks of the human brain organize themselves by phase and frequency coordination among neuron firings and neural subnetworks as for example the network oscillators of which the motoneuron is a part. This coordination is achieved by the organization tendencies of the network, the descending impulse patterns from the brain and the spatiotemporal afferent impulse patterns from the periphery.
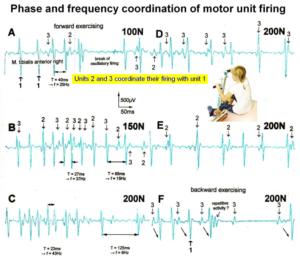
Figure 13: Phase and frequency coordination between oscillatory firing of 3 motor units (FF-type, motor units ‘2’ and ‘3’ are partly marked) during the generation of a motor program when exercising on the special coordination dynamics therapy device at loads increasing from 100 to 200N. Oscillation periods (T) and oscillation frequencies (f [Hz]) of oscillatory firing motor unit 1 (largest motor unit) are partly indicated. ‘C, F’ soleus electrodes shifted to gluteus muscles. In ‘F’, some coordination’s between motor unit ‘3’ and ‘1’ are marked.
If the premotor spinal oscillators would not coordinate their firing and synchronize their firing for longer periods of time, tremor would occur. Such pathologic synchronization can be observed in patients with Parkinson’s disease [29, 30]. If the neural networks are damaged by trauma, degeneration or malformation, the coordination between neuron firings becomes impaired and has to be repaired by movement-based learning (CDT). Drugs and operations cannot repair neural network functioning.
Improvement of the stability and exactness of phase and frequency coordination to allow specific patterns formation and learning transfer (System Theory of Pattern Formation)
The importance of stable and exact phase and frequency coordination, to allow specific pattern formation and in consequence learning transfer to other patterns, can be understood at the neuron level [31] and at the collective variable level (System Theory of Pattern formation [32-34]).
At the collective variable level, the behavioural information Finf of the coordination pattern dynamics, characterized by equations of motion of collective variables, dX/dt = Fintr(X) + ∑cinfFinf(X,t), affect the whole coordination pattern dynamics, including stability, rather than only certain coordination patterns. If the behavioural information includes the exercising of extremely coordinated, integrative movements, like exercising on the special CDT device for turning (Figure 4), then the quality of CNS self-organization can be enhanced by improving the exactness of self-organization, namely the precision of phase and frequency coordination between neuron and neural assembly firings. By improving the precision of organization of the intrinsic dynamics Fintr(X), that is, the specific variability of the injured networks, certain patterns do then already re-appear. In the permanent coma patient Manolis, the consciousness pattern re-appeared through 4.5 years of mainly exercising on the special CDT device [17] (Results).
At the neuron level, neurons often serve more than one network pattern at the same time by time sharing of neuron firing and, in this way, give rise to learning transfer among the activated patterns. If subnetworks are improved in the organization of one pattern, the organization of the other pattern will also improve. Neurons involved in the organization of breathing and activating intercostal muscles, for example, are also involved in the organization of trunk stability. By reducing the spasticity of the trunk (in patients with Parkinson’s disease), the breathing will also improve. Similarly, sphincteric motoneurons are involved in continence and pelvic floor weight bearing. If during pregnancy the pelvic floor is not trained, sometimes incontinence occurs. This stress incontinence after birth can be repaired by learning transfer from coordinated movements. By mainly exercising on the special CDT device and jumping on springboard, urinary bladder functions can be repaired by learning transfer in healthy women.
Measuring CNS functioning by the arrhythmicity of exercising (coordination dynamics value)
The impaired phase and frequency coordination at the single-neuron level, the assembly level and the macroscopic level can be measured macroscopically when the patient is exercising on a special coordination dynamic therapy device (Figure 25) on which arms and legs turn with a slightly different frequency (transmission 19 (arms) : 18 (legs)). The phase coordination between arms and legs is imposed by the device. The loss of phase and frequency coordination between arm and leg movements becomes visible and measurable by the arrhythmicity of turning. During a turning cycle the coordination between arms and legs changes between pace and trot gait and according to the difficulty of the coordinations, the turning frequency increases and decreases. This frequency variation (df/dt; f = frequency) can be recorded, quantified and displayed on a computer screen (Figures 20, 26, 31) and is called coordination dynamics value. CNS functioning is therefore measured though pattern change (continuous change from trot gait to pace gait) according to the System Theory of Pattern Formation.
During the functional reorganization of the injured CNS of patients, the relative phase and frequency coordination of neuron firing has to be entrained as exactly as possible by the movement induced afferent impulse patterns from the receptors (learning through feedback information) to restore coordination in the range between 3 and 5 milliseconds (approximate lengths of postsynaptic potentials). The device has therefore to impose the exercising patient a coordination in the millisecond range for the different coordination’s of arm and leg movements between pace gait and trot gait. The easy pace and trot gait coordination’s, but not the difficult intermediate coordination’s, can often be performed by the patient easily. Therefore, the continuous change from the easy to the difficult coordination’s and backwards diagnoses the capability of the CNS to organize easy and difficult organizational states. If the movement states can be easily generated by the neuronal networks of the CNS, then the frequency variation of turning is small during the turning cycle, and if the movement state is difficult to be organized by the CNS, then the frequency variation is large (the coordination dynamics value is large).
As long as the patients are in the coma and the patients are made moving passively, the coordination dynamics value cannot be measured. But when brought out-of-coma through CDT or when recovering spontaneously from coma, it becomes possible to measure CNS functioning (Figures 20, 26, 31).
Unique properties of special CDT devices
The special CDT device has three important properties. First, the patient performs coordinated arm, leg and trunk movements when exercising on it. The training of integrative patterns take care of that the pathologic organization cannot escape from repair by shifting to another part of the CNS and the whole CNS, including the injured parts, is reorganized so that other CNS parts can take function over through plasticity. Second, the device is extremely exact, so that the endplate potentials in the neural networks (approximately 5ms long) overlap, to improve the efficiency of organization. In spinal cord injury, for example, the transmission over the injury site will increase. Third, the coordination between arm and leg movements changes from pace to trot gait, imposed by the device. The intermediate coordination patterns between pace and trot gait are difficult to generate for the CNS neural networks. If the patients CNS learns to generate these intermediate patterns, imposed by the device, then the neural networks have learned to function better in the deep complexity of CNS organization. The patient’s nervous system learns by turning from the device, to function more physiologic through improving especially the phase and frequency coordination among neuron firings. This phase and frequency coordination can be recorded by the single-nerve fiber action potential recording method (Figure 10) invasively and by single-motor unit surface electromyography non-invasively (Figure 13).
When exercising on the special CDT device, including speech therapy (Figure 14), the whole sensory-motor cortex is activated and entrained, including the premotor areas and the association field, and also the basal ganglia and other nuclei or structures.

Figure 14: A cerebral palsy girl during exercising on a special CDT device. At the same time, the mother (teacher herself) is administering speech therapy to her. In such a very integrative training setting, nearly the whole somatosensory and motor cortical fields are activated with their associated fields for repair. – Cortical fields are taken from Penfield W and Rasmussen T, New York, 1950. – This special CDT device for measuring and therapy (int.pat.) is produced by the firm: Giger Engineering, Martin Giger dipl.Ing.ETH/SIA, Herrenweg 1, 4500 Solothurn, Switzerland, www.g-medicals.ch.
Interpersonal coordination and co-movement
To induce learning of movement patters in the hemiparetic Alen (case 4), interpersonal coordination and co-movement were used. When the therapist is performing the movement simultaneously in interpersonal coordination [32], she/he can draw the patient into a better movement pattern.
When a hemiparetic patient performs with both arms, hands, fingers or legs the same movement, then the paretic side can learn from the good side the movement pattern. Such learning/pattern transfer can be very fast, even immediately. In the patient Alen, the CNS learned very fast power (Figures 32 and 33) and precision grip (Figure 34).
Coordination dynamics therapy adapted to coma patients
The movement-based learning therapy of coma patients consists mainly of exercising them passively on a special CDT device for improving mainly the impaired phase and frequency coordination (Figure 15AB) and sky-walking (Figure 15C-D) to train the walking and the upright position for counter-acting an orthostasis syndrome. Additional conventional physiotherapy and speech therapy can be administered. When the patient fully recovered from coma, additional movements can be trained. When the speech is repaired, all kinds of communication can be trained.

Figure 15: Movements administered to a 23-year-old male patient in the vigilant coma by family members. All movements were performed passively, because the patient was in coma. A, B. Exercising on the special CDT device in the lying position (both hands are fixed) and sitting position. C, D, E. Exercising on a sky-walker.
Learning occurs as a modification of existing structures and processes. By inducing trial and error-elimination processes [35] in subunits of the changing nervous system, optimal repair may be achieved. To teach the injured CNS to repair itself by trial-and-error elimination processes, the CNS has, in similarity to development, to recognize through CDT, which sub-networks, regulation units or sub-loops are not functioning properly or missing and to repair them by error-elimination, including the possibility that other parts of the brain partly take functions over and sub-networks are built anew to a limited extent.
Results
With 4 case reports the scientific background will be given to show that euthanasia is likely to be performed through mainstream medicine worldwide because with respect to CNS repair the universities are 30 years out-of-date (1), money seems to be more important than the life of patients (2) and protection of vested rights is more important than improving medicine and safe the life of patients (3).
Case report 1, Manolis, permanent coma recovery through coordination dynamics therapy
Recovery situation before CDT was started
The 22-year-old Manolis suffered an extreme severe brain injury in a car accident. In the accident a metal shard went into his right brain and nervous tissue was lost. The severances of the injury can partly be seen in Figure 16. After surgeries in a university clinic, he was sent to a conventional rehabilitation center. At the beginning of conventional rehabilitation, his relations could communicate with him via eye blinking. After a few months this communication was lost. The pathologic processes seemed to have won against the physiologic ones. The family did not want that Manolis would die. They took him from the rehabilitation center and started CDT at home with a lot of vegetative nervous system problems at the beginning of therapy as for example the blood pressure [36].
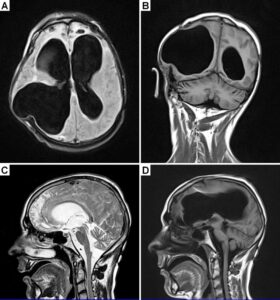
Figure 16: MRI of a 23-year-old male patient with a very severe traumatic brain injury. The pictures were taken one year after the car accident. Since a metal shard went into the brain during the accident, some probably infected brain tissue had to be removed. A shunt was installed to regulate brain pressure. Because of the loss of nervous tissue, the ventricles are enlarged; they look like in cases of hydrocephalus. Many parts of the brain were damaged during the accident, including both frontal lobes (A, C).
Realizing the very severe damage of the brain of Manolis (Figure 16), the Author himself had doubts whether it would be possible to get him back to life through CDT. Based on his experience with rehabilitation, the neurosurgeon, who operated the patient after the accident, predicted that the family members should be happy if they could keep the health level of the patient (Figure 17A), which means vegetating in the coma for ever till he would die on a complication within approximately 5 years.
Repair through 5-years-CDT
Following 3 to 5 years of CDT with 20 hours therapy per week, Manolis came via the minimally consciousness state [37] out-of-coma. When the Author saw him first time to lift his head and kissed the mother, after 4 years of CDT, he had the feeling that Manolis raised from the dead. After 3 years of CDT, the permanent coma patient slowly reached the minimally consciousness state. After 5 years of CDT, six years after the accident, Manolis was fully conscious. He could play and laugh with the mother or other relatives (Figure 17B), sit freely on bed and could just keep the crawling position. He could also sit freely, but he could not stand and walk. He could generate sounds, but could not speak. The left hemisphere, where the main speech centers are, was not damaged that much. It seemed therefore possible that the patient could re-learn a bit to speak. After being out of coma and being able to move a bit on volition the head, trunk and right arm, the repair of the former coma patient seemed to speed up. But there were a lot of spasticity and pain problems and whether he could ever reach a meaningful life state was unclear.
 Figure 17: A. Picture of the 23-year-old patient being 1.5 years in the vigilant coma following a car accident. The impression in the face is unhealthy. The photo shows the patient 2 years before when he was in the army. B. The facial expression of Manolis following 5.7 years of CDT during counting in English the numbers one-two-three-four-five. Note the improvement of the facial expression.
Figure 17: A. Picture of the 23-year-old patient being 1.5 years in the vigilant coma following a car accident. The impression in the face is unhealthy. The photo shows the patient 2 years before when he was in the army. B. The facial expression of Manolis following 5.7 years of CDT during counting in English the numbers one-two-three-four-five. Note the improvement of the facial expression.
Repair through 5.5-years-CDT
Following 5.5 years of CDT, 6.5 years after the accident, Manolis became able to activate old-learned movement patterns as eating and playing partly violin. Old-learned movements are helpful for CNS repair, because they are stored in the cerebellum or other lower parts of the CNS. If for example patients could ride a bicycle before the accident, this movement pattern should be used, if possible, also for repair.
Manolis could still not speak. When being pushed to say mama, he succeeded to say ‘ma’. It was thought that maybe he could re-learn with further therapy to say ‘yes’ and ‘no’ and ‘mama’ and ‘papa’, especially because the brain repair seemed to speed up.
Repair through 5.7-years-CDT
Through 5.7 years of CDT, Manolis became nearly suddenly able to speak again, which was completely unexpected. He could repeat every word in Greek (mother tongue) or English. The pronunciation was good. The mother said, that when her son became able to speak at the 20.7.2018, she had the feeling to have got wings for going on with the therapy. When playing with one of the sisters, he could also smile (Figure 18). Even though Manolis had re-learned to speak, a discussion was not possible because of the still missing cognitive functions.

Figure 18: Manolis during playing with a sister. From the expression of the face it can be seen that he enjoyed to play. He could smile again.
Repair through 6-years-CDT
Following 6 years of CDT, 7 years after the accident, Manolis became able to turn a bit on the special CDT device by himself. According to experience, when patients become able to exercise by themselves on a special CDT device (before the patient was exercised passively), further functions become repaired. Cognitive functions and memory slowly re-occurred in Manolis. He started to remember songs from before the accident. When showing him numbers he could say the numbers and count also a bit. Real communication started to become possible. For example: “Why don’t you use also the left hand for exercising” – “because I have pain in the left arm”. He became able to eat by himself; artificial nutrition was reduced. Manolis developed strong muscle power in the right arm and hand and became over-active. All the time he moved about and played with the right hand to get contact and input.
Repair of the left body side
A further big problem of the now conscious patient was the repair of the left body side due to the mainly lost right cerebral hemisphere (Figure 16) in similarity to stroke patients or patients following hemispherectomy [38]. The pyramidal tract (lateral corticospinal tract) from the mainly lost right hemisphere was mainly atrophied and little activation seemed to come so far from the left hemisphere via the left uncrossed anterior corticospinal tract. How much the left hemisphere can take function over by plasticity via the uncrossed anterior corticospinal tract has to be seen.
In children, may be up to 10 years, the other hemisphere can take some function over by plasticity [39]. In a 9.5-year-old girl a transient regeneration of the spinal cord following spinal cord injury was achieved through CDT [7]. The 12-year-old Alen, with a persistent hemiplegia from birth, learned quickly through CDT some hand functions of the paretic side (case report 4).
Manolis could move a bit the left leg during training on the special CDT device. He could also move a bit the left arm and hand. But he had pain from the elbow joint. Osteophytes had grown. Two years ago, one had to see the pain in his face. Now he was clearly telling when he had pain and tried to avoid it. It has to be tried to exercise the whole body so that the nervous system is not giving up the left body side in similarity to stroke patients.
Repair through 6.5-years-CDT
The movement and cognitive functions further improved. He could clearly exercise a bit by himself on the special CDT device with the right hand and both legs, which reduced the training load on the mother, the two sister and two brothers. Exercising with both hands and legs would have been more efficient for repair. Manolis re-learned to stand with support and could also play with a ball, when siting freely on bed. Her re-learned to drink and eat, but he needed as young children the help of the mother. The sexual function returned.
Through 6.5 years of CDT, 7.5 years after the accident with 20 hours therapy per week, he was back to life. The training of Manolis looked now like the training of a normal severely brain-injured patient with the deficits from the brain injury as for example spasticity, pain and missing control of muscles. But one should not forget, Manolis was at least 4 years in coma and most likely would have died or would have stayed at best in the coma forever with conventional physiotherapy.
Repair through 7.5-years-CDT
Manolis became able to stand (Figure 19C) and walk a few steps if the left leg was supported. When sky-walking, only one or two persons were needed for support (Figure 19). At the beginning of treatment up to four persons were needed (Figure 15C). A second person was only needed, to stimulate the patient to use both hands during sky-walking. In the background of Figure 19A, a sister of Manolis is exercising on the special CDT device to reduce back pain, which she probably suffered when supporting the care and treatment of Manolis.

Figure 19: A, B. Manolis during sky-walking, only one or two persons are needed for support. In the background of A, one sister is exercising on a special CDT device. C. The patient Manolis during standing.
The most important repair progress was that Manolis learned to exercise by himself on the special CDT device (Figure 20E) for more than one hour, with the consequence that firstly the training load for the family was further reduced strongly and secondly that it became possible to measure his CNS functioning (Figure 20A-D) and quantify his CNS repair with further treatment.
It can be seen from Figure 20A-D that the patient could exercise in the forward (Figure 20A) and backward (Figure 20C) direction. He could exercise better backwards. When increasing the load from 4 to 13Newton, the coordination dynamics value got worse (higher) as in healthy subjects. They increased from 21 to 24 and 26 to 31 for exercising in the forward and backward direction. Satisfying is that the patient exercised transiently faster (Figure 20A, arrows), typical for young children during development, indicating that the CNS of Manolis was still in the phase of brain repair.
 Figure 20A-D: Coordination dynamics of the formerly permanent coma patient Manolis. The load of exercising is increased from A, C to B, D. In A, transient fast exercising is indicated by arrows. For designations, see Figure 26. The coordination dynamics cannot directly compared with those of Figures 26 and 31 because they are performed on different devices. Further, the patient exercised only with the right arm, because of pain in the left one.
Figure 20A-D: Coordination dynamics of the formerly permanent coma patient Manolis. The load of exercising is increased from A, C to B, D. In A, transient fast exercising is indicated by arrows. For designations, see Figure 26. The coordination dynamics cannot directly compared with those of Figures 26 and 31 because they are performed on different devices. Further, the patient exercised only with the right arm, because of pain in the left one.
Figure 20E shows the patient Manolis when exercising on the special CDT device during measuring the coordination dynamics. It can be seen that he exercised only with one arm, because of pain in the left elbow joint. The strong extensor spasticity would shift the body all the time in a more extended position. He was therefore fixed for not shifting, marked in Figure 20E by arrows. This strong extensor spasticity made it hard for the family to exercise him passively for years (Figure 15A). When motivated, he exercised now by himself and because of very strong power in the right arm and hand, he had no problems to exercise with one hand and the two legs against the extensor spasticity. With respect to repair, active exercising is more efficient for brain repair than passive exercising. Further brain repair can be expected with further therapy. Sometimes, the patient could be motivated to exercise with both hands in spite of the pain. The pain problem could not be solved so far.
 Figure 20E: The formerly coma patient Manolis during exercising on the special CDT device with one arm. Arrows indicate fixation against shifting, caused by extensor spasticity.
Figure 20E: The formerly coma patient Manolis during exercising on the special CDT device with one arm. Arrows indicate fixation against shifting, caused by extensor spasticity.
Brain repair in the patient Manolis who suffered an extreme severe brain injury in a car accident
It was shown with Manolis that, based on a new development in human repair-neurophysiology, the human nervous system could partly be repaired by a new treatment, called CDT, in a patient with an extremely injured brain. Even the speech could be re-paired and the higher mental functions improved. Manolis could precisely repeat every word in English or Greek and started with further repair to use the speech for communication. During instructive training, when exercising on a special CDT device (Figure 15A), he was even counting 1-2-3, in similarity to a self-instructive training. He realized the situation around him. Without telling him, he understood from discussions of the Author with the mother that the Author was working on a scientific paper. It seems possible that he can reach the meaningful life state. But whether he can start to work again is unclear.
To achieve consciousness was the most difficult step in brain repair
Actually, two important steps were achieved in this former permanent coma patient. The first step was to get him fully out-of-coma and the second to make him speak and communicate again. A third step would be to reach the meaningful life state. The very big therapy effort was to get him fully out of the coma. Approximately 5 years of CDT were needed. The speech, including memory and improvement of cognitive functions, was achieved with less effort, namely with one additional year of CDT.
Reconnection of speech networks
The rather sudden occurrence of the speech makes it likely that the speech areas were in principle operational. But they had to be re-connected functionally to the whole brain organization again (re-connection treatment). The improvement of the phase and frequency coordination, in the deep complexity of neural network organization (in the association fields), may have contributed to the activation of the speech pattern in similarity to the activation of the old-learned pattern ‘playing violin’.
Epigenetic regulation for repair
Such tremendous repair achieved via CDT, especially in the permanent coma case, seems only possible if the epigenetic regulation for repair had been substantially activated by movement-based learning. CDT had induced the stimulation of those pathways that regulate neural network repair. Epigenetic mechanisms, stimulated by physiologic network activation, are likely key players within signaling networks, as DNA methylation, chromatin remodeling and small non-coding RNAs superfamily and are required for the fine-tuning and coordination of gene expression during neural network repair by learning. The complexity of the epigenetic regulation is tremendous.
To generate repair in the nervous system, it is likely that permanent changes in gene expression patterns are achieved through permanent changes in chromatin remodeling without changes in DNA sequence. The concept of chromatin remodeling addresses a key challenge of how stable changes in gene expression are induced [40] in neural networks to produce long-lasting changes in repair. DNA methylation is one of the many epigenetic modifications that can alter gene expression. Dynamic and reversible DNA methylation may be essential for learning and memory formation and could transmit repair influences onto adult neurogenesis (Figure 21).
Such tremendous brain repair makes it likely that also new nerve cells were built during the 7.5 years of movement-based learning (CDT) through excitation-neurogenesis coupling [41].
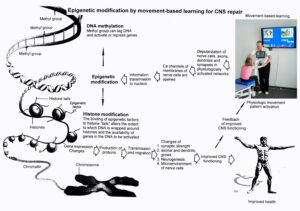 Figure 21: Epigenetic regulation for repair by movement-based learning. CDT-induced stimulation of the pathways that regulate neural network repair is a proven therapeutic and preventive tool. Epigenetic mechanisms, stimulated by physiologic network activation, are likely key players within signaling networks, as DNA methylation, chromatin remodeling and small non-coding RNAs superfamily are required for the fine-tuning and coordination of gene expression during neural network repair by learning. Since the nervous system is involved in nearly all body functions, CDT will improve health.
Figure 21: Epigenetic regulation for repair by movement-based learning. CDT-induced stimulation of the pathways that regulate neural network repair is a proven therapeutic and preventive tool. Epigenetic mechanisms, stimulated by physiologic network activation, are likely key players within signaling networks, as DNA methylation, chromatin remodeling and small non-coding RNAs superfamily are required for the fine-tuning and coordination of gene expression during neural network repair by learning. Since the nervous system is involved in nearly all body functions, CDT will improve health.
Case report 2, Fovios, very fast repair after 16 years of getting worse
Recovery situation before CDT was started
The 17-year-old Fovios suffered in a motor cycle accident a very severe brain injury. The neck hit a street border stone. Brain and brain stem were injured and he was unconscious following the accident. Most likely he was ventilated. The parents were asked whether they agree that Fovois could be used as a potential organ donor. They refused. Unexpectedly, the young man recovered from coma after 7 months spontaneously. The patient was continent. The remained continence was also unexpected, because in very severe brain injury also the continence is lost. But in a rather complete spinal cord injury also sometimes the continence is remained. Conventional physiotherapy was administered with little progress. A leg operation was performed 4 years after the accident. Fovios became able to move slowly in the upright position without support.
Repair through 3 therapy sessions of CDT
16 years later, at an age of 33, the father came with his son three times for consultation and treatment to the Author. The patient needed for upright moving support (Figure 22A). Together with the Author a highest speed of 3m per 35s was achieved (which is an extremely slow speed) when the Author was holding both hands for support and balance (Figure 22B).

Figure 22: A. Patient Fovios with a severe brain injury during moving. B. The patients speed of moving, when supported by the Author, was 3m per 35s.
The right hand and arm were spastic (Figure 22A) like in stroke patients. When the Author was holding both hands the spasticity in the right hand reduced (Figure 22B). Through exercising on a special CDT device for 30min to 60 min, the right-hand spasticity reduced strongly in the short-term memory as in stroke patients.
When the right hand was fixed to the handle of the special CDT device, the patient learned unexpectedly quickly to exercise by himself. First the Author supported the turning (Figure 23). Then the Author included during the support coordinated instructive training by counting in coordination with the handle position “one – two – three – “(Figure 24). After approximately 30min of exercising the CNS functioning had improved that much so that the patient became able to turn by himself. It became thus possible, besides the training for repair, to measure the improvement of CNS organization via the coordination dynamics in the three therapy sessions two to three days apart (Figure 25). The improvement of CNS functioning will now be analyzed.
 Figure 23: The Author is supporting the exercising on the special CDT device, because the patient is at the beginning of treatment unable to turn by himself. The right hand had to be fixed to the handle by a bandage.
Figure 23: The Author is supporting the exercising on the special CDT device, because the patient is at the beginning of treatment unable to turn by himself. The right hand had to be fixed to the handle by a bandage.
 Figure 24: The Author is including during the supported exercising the instructions “1 – 2 – 3 – …” in coordination with the turning movements to speed up the learning process. The speaking of the Author is suggestive as can be seen from the expression of his face.
Figure 24: The Author is including during the supported exercising the instructions “1 – 2 – 3 – …” in coordination with the turning movements to speed up the learning process. The speaking of the Author is suggestive as can be seen from the expression of his face.

Figure 25: The patient became able to exercise by himself and the nervous system functioning could be measured.
Increase of the turning frequency as the first sign of improvement of CNS functioning
In Figure 26 the improvement of CNS functioning is shown from the beginning of the first to the third therapy session. When the patient became able in the first therapy session to turn by himself, he could turn only slowly (Figure 26A, 0.339Hz). Then he became able to turn faster (Figure 26B, 0.464Hz). During the second therapy session he could turn further faster (Figure 26C, 0.529Hz) and during the third session still faster (Figure 26D, 0.679Hz). The increase of the turning frequency is one indication of improvement of CNS functioning. It increased by 50%. For comparison, the inner frequency of turning of the Author is in the range of 1.5Hz.
Reduction of coordination dynamics values as the second sign of CNS functioning improvement
The coordination dynamics values also improved (reduced). They reduced from 57.845 (Figure 26A) to 57.530 (Figure 26B) in the first therapy session and further to 50.131 (Figure 26C) to 46.110 (Figure 26D) during the second and third therapy sessions. The improvement of CNS functioning, quantified by the coordination dynamics value, was by 20%. The decrease of the coordination dynamics values is a second measure for the improvement of CNS functioning. For comparison, the healthy and trained Author has a low-load coordination dynamics value in the range of 2.3 (Figure 31E) in comparison to 46, which the patient reached. The Authors CNS functioned at that time 20 times better.
The first selective improvement of the pace and trot gait automatisms are a third sign of CNS repair
Interesting is further, how the different coordination patterns during exercising improved, which can be judged here by the frequency of turning. At the beginning of CNS repair, there was nearly no preference to a certain exercise pattern (Figure 26A). The patient got often nearly stuck. Then slowly the trot gait pattern (K) improved (Figure 26B), because he could turn continuously with higher frequency around the trot gait pattern. During the second session, pace (P) and trot gait (K) movement patterns improved strongly. During the third therapy session a rather continuous exercising became possible. The patient only seldom got stuck for certain exercise patterns. The frequency did not reduce transiently to zero (Figure 26). On the coordination dynamics trace of the healthy and trained Author no priority of certain patterns can be seen. His CNS manages all movement patterns between pace and trot gait well (Figure 31E, F).
In conclusion, during the repair through CDT, the CNS gave first priority to the repair of the automatism patterns pace and trot gait, which humans need for crawling, walking and running. That means that during the repair of the CNS, for life most important patterns are repaired first. The repair of the automatism patterns pace and trot gait is a third measure for the improvement of CNS functioning.

Figure 26: Coordination dynamics improvement of the patient Fovios with a very severe brain injury due to a motor cycle accident. P = pace gait, K = trot gait. The frequency and the coordination dynamics values are mean values of 1min exercising. The coordination dynamics trace gets out of range because of poor coordination between arm and leg movement and in turn because of strong impairment of the phase and frequency coordination among neuron firings.
To keep the level of CNS functioning
With several inefficient treatment Fovios could not keep during 16 years the level of CNS functioning. First, he managed to move without a stick. Now at an age of 33 he needed a stick to slowly move. To keep the level of achieved CNS functioning, he may have to train every day for one hour. Against the advice of the Author, the therapy was not continued.
Prognosis
Even though the patient did not get better over 16 years, but got worse, he could be improved in three sessions with up to one-hour duration. An intensive CDT with 20 hours therapy per week would improve most likely the right-hand function, improve breathing and would make him walk again. The problem was that after 16 years and trying out many inefficient and ‘hocus-pocus’ treatments the patient and the relations did not believe in anything anymore and were worn out to fight again.
Because of insufficient breathing, his speech was quietly. An improvement of the breathing center would improve his speech. Even though his higher mental functions are probably only little impaired, an urgent therapy would be necessary, because he attempted already once to suicide. With an intensive efficient therapy like CDT, Fovios would have a good prognosis to get rather fully back to life, because his CNS improved quickly in its functioning already through three sessions of CDT.
Necessity for an improvement of the breathing center functioning
During the third therapy session, Fovios got problems with the breathing. He could not sufficiently inspirate to get sufficient oxygen supply for exercising and neural network repair. For sure he was not fit. Probably he had not trained fitness for years. During repair, power is needed for muscle activation and for neural network repair. The CNS neural networks have ‘stress’ to generate the especially complicated patterns between pace and trot gait. During exercising for repair, the patients with severe brain injuries sweat because of muscle power generation and neural network repair. The CNS has difficulties to generate, in the deep complexity of CNS organization, the complicated patterns between pace and trot gait and has therefore stress and the patient sweats.
For repairing efficiently his CNS, priority has to be given first to the repair of the breathing center in the formation reticularis in the brain stem (case report 3). For turning faster and longer, may be, oxygen has to be administered during the therapy sessions.
Comparison to very severe brain injury
In comparison to a severe brain injury as in the patient Manolis, Fovios with probably mainly a brain stem injury (a new MRI was not available) is well up, because his higher mental functions are probably only little impaired and his brain stem injury can be repaired through CDT. Since the breathing is an automatism, the genetics will help for efficient repair as found out in animal experimentation. When the breathing center was damaged in a dog, it recovered spontaneously within two hours [42, 43].
Case report 3, Rafaela, breathing repair and cancer treatment
Breathing center injury repair
When jumping on a trampoline, the eight-year-old Rafaela fell on the back and hit probably with the neck the metal support surrounding [44] in some similarity to Fovios. As can be seen from her MRI, Rafaela had suffered an incomplete injury of the spinal cord extending from the thoracic segments Th1/2 rostral till to the medulla oblongata (Figure 27B). All the cervical spinal cord segments were damaged probably by pressure, caused by the edema and/or lack of blood supply caused by the pressure.
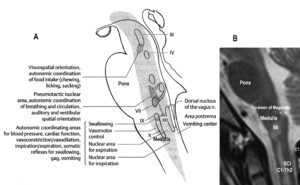 Figure 27: Injury of the medulla (MI) and the spinal cord (SCI, C1-Th2) of the eight-year-old patient Rafaela. By comparing the MRI (B) with an anatomical picture (A) and the clinical picture, it turned out that at least the nuclear area for inspiration/expiration, the nuclei of the vagus nerve (X), the phrenic nerves (C3-5) and the accessory nerve (XI, C2-4) were injured.
Figure 27: Injury of the medulla (MI) and the spinal cord (SCI, C1-Th2) of the eight-year-old patient Rafaela. By comparing the MRI (B) with an anatomical picture (A) and the clinical picture, it turned out that at least the nuclear area for inspiration/expiration, the nuclei of the vagus nerve (X), the phrenic nerves (C3-5) and the accessory nerve (XI, C2-4) were injured.
It seems that the injury included also a damage of the caudal part of the reticular formation and the nuclei of the vagus (X) and accessory nerve (XI). The caudal reticular formation is the nuclear area for inspiration and expiration. This conclusion is supported by the clinics. Rafaela, being in the coma, had problems with breathing and was connected to a respirator. Five years later, Rafaela was operated because she had stones in the kidneys and a big stone in the bladder, indicating that, most likely, also the vagus nerve/nucleus was damaged, because the vagus nerve regulates the secretion of the kidneys. From Figure 28A it can be seen that the shoulders of Rafaela are too much curved forwardly.
With intensive CDT for three months her breathing and her movement functions improved (Figure 28) [44]. She could stand up by herself from the sofa with a few trials (Figure 28B, C) and exercise on the sky-walker (Figure 28D).
 Figure 28: A. The patient Rafaela (with mother and sister) with an incomplete spinal cord injury extending from the thoracic Th1/2 segments rostrally to the medulla oblongata (including all cervical segments). Note the bending of the shoulder and the hanging of the arms, due to the injury. The expression of her face characterizes her psychological state. B, C. Through CDT, Rafaela succeeded to get up from the sofa by herself. D. She became able to perform sky-walking following three months of therapy. Her laughing indicates that also her breathing had improved with therapy.
Figure 28: A. The patient Rafaela (with mother and sister) with an incomplete spinal cord injury extending from the thoracic Th1/2 segments rostrally to the medulla oblongata (including all cervical segments). Note the bending of the shoulder and the hanging of the arms, due to the injury. The expression of her face characterizes her psychological state. B, C. Through CDT, Rafaela succeeded to get up from the sofa by herself. D. She became able to perform sky-walking following three months of therapy. Her laughing indicates that also her breathing had improved with therapy.
When the coma regressed in Rafaela 10 days after the accident, she had no motor functions below the injury level and she was connected to a respirator. The physicians told the mother that Rafaela will stay like this for the rest of her life, but Rafaela recovered quite well with respect to motor functions and breathing. She was good at a normal school. With further CDT, Rafaela would improve further her motor functions and her breathing to become able to raise her voice.
The injury of Fovios was much more severe because Rafaela was 10 days in the coma and Fovios 7 months (case 2), which seems to be the average limit that a patient, following severe brain injury, can recover from coma spontaneously; even though the Author knows a case, where a 17-years-old lady (at accident) recovered spontaneously from the coma even 1.5 years after the severe brain injury. The severely brain-injured patient Manolis (case 1) recovered from permanent coma through 4 to 5 years of aggressive CDT. Interesting is that when the Author studied medicine, after engineering and theoretical physics, he had the impression that after 4 to 5 years of learning medical facts, the learning improved including the memory. Long-lasting learning is powerful in brain repair and brain functioning improvement.
Rafaela’s case report indicates that the breathing center can also be repaired in human, in accordance with animal research [42, 43]. That means that having a severely brain-injured patient who is in coma and cannot breathe, the passive turning in the lying position is possible (Figure 15A), even when connected to a respirator. This also holds for Covid-19 infected patients in intensive care units. They would have a better prognosis when passively exercised on a special CDT device while ventilated.
Authors own experience of using the special CDT device in hospital for improving body function repair
The Author suffered a ‘squamous cell carcinoma (epithelioma)’ (a malign tumor) in the maxilla. The tumor (stage between 1 and 2) was removed by surgery and a neck dissection performed. Two lymph nodes with formation of metastases were removed and two stages of further lymph nodes and lymph vessels were removed for safety reasons. Radiation therapy and chemotherapy were administered to the tumor area to reduce the risk of tumor recurrence from 30% to 15%. To mitigate the side effects of the anti-cancer treatment, the Author performed CDT for fifteen hours per week.
One year after the tumor extirpation and neck dissection, a reconstruction of the maxilla was performed. The Author was fit by the time he went for the fibula-transplantation operation and the hematocrit was high (no blood needed in the operation). He exercised one hour before the operation on the special CDT device to counteract the down-regulation of BDNF and other factors due to the coming stress event (operation). During the nine-hour operation, pieces of the fibula and the skin with its supplying artery and vein were removed from the right leg. Bone and skin were placed to the former site of the tumor and artery and vein were connected with the temporalis blood vessels. The transplant had to receive blood supply within seven hours in order to avoid rejection. The Author was informed that during the long operation he will get edema and breathing difficulties because of the removed lymph nodes and vessels following the previous neck dissection. However, only minor neck edema occurred during the operation because the CDT had partly repaired the lymphatic system by performing CDT. One day after the reconstructive operation parts of the transplant were blue, indicating poor blood supply, even though the transplanted artery was open and was supplying blood. The surgeon informed the Author that he would lose some tissue because of poor blood supply.
The Author, having brought the special CDT device into the hospital, exercised on the special device, in spite of the many tubes he was connected to, to improve the blood supply to the head including the transplant site. As a result of the enhanced blood circulation, the transplant area received more blood and healed fully. No transplanted tissue was lost. The surgeon was amazed that his 9-hour lasting complicated work was fully successful. He himself said that the reconstruction was 100% successful. Therefore, CDT had helped to reduce the risk of severe neck edema occurring during the operation and a tracheotomy could be avoided and CDT had helped to improve the blood supply also in the head with the result that the transplant was fully accepted. The Author’s one hour exercising before the operation may have helped in this long-lasting and difficult operation and may have helped to improve the lymph circulation in the short-term memory to reduce edema during the operation.
In conclusion, all surgery went well, aided by the continuously performed CDT. CDT had helped to repair the body after cancer treatment and probably had helped to avoid cancer recurrence.
It is important to note that following the neck dissection (and tumor resection, radiation and chemo therapy) the lost or impaired taste, swallowing, coughing and other automatisms, partly reappearing spontaneously, recovered better due to CDT. The exercising of the complicated coordination’s between pace and trot gait when exercising on the special CDT device, which stimulate the autonomic nervous system, helped to achieve better repair. Even though the eyes are a part of the nervous system and should be reached by CDT, the improvement of the eye functions (wetting of the cornea, opacity of the vitreous body) seems to be most difficult to be repaired by CDT. Ten years after the cancer treatment the wetting of the cornea and the opacity of the vitreous body had improved but are still disturbed. Generally, not all side effects of chemo and radiation therapy had disappeared following ten years of CDT. The sleep, for example, is still disturbed. The chemotherapy probably impaired nervous system functioning and in consequence many body regulations. It is known that the drug Vinblastine, which was administered to the Author, is nervous system toxic. The patients may get polyneuropathy. For further see [18].
In order to reduce the risk of a tumor recurrence after the removal of the epithelioma, radiation and chemotherapy (Vinblastine) was administered to the Author. But experiencing the long-lasting side effects (more than 10 years), may be, the Author should have left out chemo and radiation therapy. A reduction of the probability of cancer recurrence can also be achieved through performing CDT, because CDT improves cardio-vascular performance and generates additionally NK immune cells (natural killer cells) [45]. The improved immune system has therefore better access to regrowing cancer cells and small metastases anywhere in the body [18]. Generally, physical activity improves the prognosis of cancer patients [46, 47]. But physical activity during cancer treatment is not organized.
Case report 4, Alen, wrong prognoses and treatment of mainstream medicine
With the first case report it was shown that a permanent coma patient could be brought out-of-coma and could live much longer with a better quality of life. The medical prognosis and treatment were wrong. With the second case report it was shown that even after 16 years of getting continuously worse, substantial repair through CDT was possible. With the third case report it is shown that even the breathing center can be repaired, which mostly impaired in patients is drifting in the direction of brain death because of missing adequate therapy. With the fourth preliminary case report it will be shown that the prognosis of repair was completely wrong. By withholding adequate therapy, it was tried to steal a young patient a better future.
Recovery situation before CDT was started
The patient Alen suffered a perinatal insult with asphyxia. He sustained a cerebral hemiplegia on the left side, a parenchyma defect of the basal ganglia and a degeneration of the pyramidal tract.
Alen was born through a cesarian. He could not breathe. When the fluid, mixed with blood, was removed from the lung, he started to breathe. The time period of apnea is unknown. At an age of 8 years, a parenchyma loss of the basal ganglia was diagnosed and a Wallerian degeneration of the pyramidal tract at the site of the pons found, indicating a degeneration of the lateral corticospinal tract and the anterior corticospinal tract. The loss of the parenchyma of the right basal ganglia was probably caused by post-ischemia and/or post-hemorrhage following a subependymal germinal matrix bleeding with pressure onto the close pyramidal tract. Brain injuries could therefore be caused at different sites of the brain (Figure 29).
At an age of 12 years, CDT was started. Alen had many movement deficits and also cognitive deficits. Here it will be concentrated on the cerebral plegia and especially the not functioning left hand. Alen could not use the left hand and was managing everyday life with the right hand.
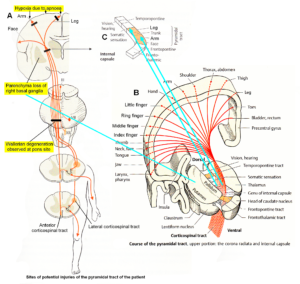
Figure 29: Sites of injuries of the CNS of the patient Alen. The Wallerian degeneration of the right pyramidal tract has consequences also on the ‘good’ right side through the anterior corticospinal tract. Figures partly taken from [48].
Hand function recovery through 6 weeks of Coordination Dynamics Therapy
Alen had never used the left hand in his life. When starting CDT and exercising with him on the special CDT device in the lying and sitting position (Figure 30A), the left hand was fixed to the leaver. Slowly some muscles in the left hand were activated and Alen became able to exercise on the special CDT device also a bit in the standing position, when supported by the mother (Figure 30B). Also, the measuring of the coordination dynamics values became possible to quantify CNS functioning improvement on the long term (Figure 31). For higher loads (55 Newton), the coordination dynamics value got much worse (higher), indicating that substantial brain repair (neural network reorganization) needed to be done.
Very important was to get useful functions in the left hand to manage better everyday life. Losing one hand function in Switzerland is a disability of 50%. The first step to learn left-hand functions was to learn the power grip and the precision grip.
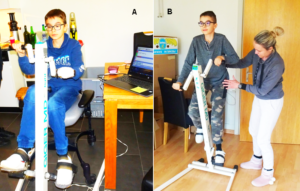
Figure 30: A, B. The patient during exercising on the special CDT device in the sitting (A) and standing position (B). In the sitting position, his CNS was measured to obtain the coordination dynamics value. The left hand had to be fixed, otherwise it would slip from the handle.
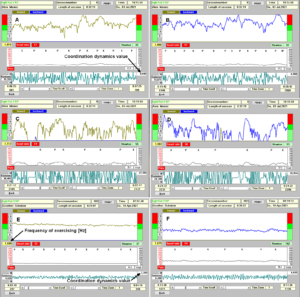 Figure 31: Low-load (32N) coordination dynamics in the forward (A) and backward (B) direction of the patient Alen. For higher loads (55N) (C, D) the coordination dynamics values are much worse (increase from 8.4 to 27.3 and from 6.9 to 26.9). E, F. Nearly ideal values from the Author for comparison (CDvalue37N = 2.4 and 162N = 6.0).
Figure 31: Low-load (32N) coordination dynamics in the forward (A) and backward (B) direction of the patient Alen. For higher loads (55N) (C, D) the coordination dynamics values are much worse (increase from 8.4 to 27.3 and from 6.9 to 26.9). E, F. Nearly ideal values from the Author for comparison (CDvalue37N = 2.4 and 162N = 6.0).
Through 6 weeks of CDT, Alen’s motor functions improved and he could hold longer times the left hand on the leaver without fixation when exercising on the special CDT device. But he was still not using the left hand in every-day life. Therefore, the Author started to work with know-how on the left hand to get it functioning.
Power grip
To induce the power grip pattern, the Author used the co-movement strategy for brain repair. Alen was asked to take with the right good hand the glass with no water and should simulate the water drinking. Of course, there was no problem. Then he was asked, to hold strongly with the right one glass and take with the left had the second glass (Figure 32A) and bring it to the mouth for drinking (Figure 32B, C) and put it back then to the table (Figure 32D). Unbelievable, he could manage through strong concentration. And then he was asked, by the mother, to perform the drinking performance with the left bad hand without holding with the right good hand the glass (Figure 32E-H). Unbelievable, he could manage. The power grip started to work a bit.

Figure 32: A-D. Power grip learning of the patient Alen. A-D. Through co-movement from the right good hand to the left bad hand, he could initiate the power grip in the left bad hand. E-H. After realizing that the left hand can do the drinking performance, he became able to use only the left bad hand for the drinking pattern.
The next step was the reality test. Is Alen able to perform the drinking in reality? Mother, Alen and the Author were going to the kitchen to see whether Alen could drink by himself with both hands. Alen opened the tap with the right good hand (of course no problem), took the glass with the bad left hand, filled the glass with water (Figure 33A), did drink water in the normal way (Figure 33B), and pore the rest of water into the basin (Figure 33C). After finishing the drinking, he was crying for joy, because first time in life, he managed to drink water in the normal way (Figure 33D). Before he had to open the tap with the right hand, take a glass with the right hand, get water into the glass, drink, put the glass back with the right hand and close the tap with the right hand.
 Figure 33: After 6 weeks of CDT, the patient Alen with a cortex and a basal ganglia injury learned at an age of 12 to drink with both hands (A-C), first time in life through 6 weeks of CDT. Ale is crying for joy because he succeeded (D).
Figure 33: After 6 weeks of CDT, the patient Alen with a cortex and a basal ganglia injury learned at an age of 12 to drink with both hands (A-C), first time in life through 6 weeks of CDT. Ale is crying for joy because he succeeded (D).
Precision grip
After being very successful with the learning of the power grip, the question arose, is Alen able to generate the precision grip, first time in life. Again, the co-movement strategy was used. First, he took a glass ball with the right good hand, which was of course working. Then, when holding one glass ball with the right good hand, he became able to take a second glass ball with the bad left hand (Figure 34A), bumping both balls together (Figure 34B) and put them back to the table. Then he was asked by the mother, to take a glass ball with the left hand only and he succeeded (Figure 34C, D). Even though, the right good hand was not in the precision grip pattern, still the fingers are a bit in that position (Figure 34C, D).

Figure 34: Through co-movement, the patient Alen became able to generate the precision grip pattern. Note, the positioning of the left wrist joint is plantar flexed (A-C). In D the wrist joint is in a quite well position. Note further, with the right good hand, he took the ball with two fingers (A,) and with the bad left hand he needed 3 fingers for the precision grip. Motor units could be activated coordinately in finger muscles (E).
That Alen learned the power grip and precision grip patterns through 6 weeks of CDT is a dimensional step forward (reduction of disability by approximately 30%). Still much more has to be learned by him through repair. As can be seen from Figure 33C, D and Figure 34, the fingers and the wrist of the left hand are often not activated in the right way. Also, the power was missing. Anyhow, some motor units were activated in the fingers in a very important physiologic pattern (Figure 34E). Alen became able to eat a bit with both hands, but the pattern of the left hand was pathologic.
The consequences of the improvement of the left hand and finger functions was that the patient for example became able to eat pasta with both hands in a rather physiologic way (Figure 35).
 Figure 35: Patient Alen during mixing (A) and turning the pasta in the spoon (B), first time in life.
Figure 35: Patient Alen during mixing (A) and turning the pasta in the spoon (B), first time in life.
Real power grip following 4 months of CDT
To generate the pattern for the power grip was a first step. But for a real power grip also power is needed. To generate more power, muscle fibers have to grow and that needs a few months.
Generally, it is not sufficient that the hands and fingers can perform certain movement patterns, also power is needed. On the special CDT device, Alen trained also to generate power, when training at higher Newtons. So far, he succeeded to train up to 50N. A healthy pupil could exercise approximately against 100N. To see the increase of power with CNS repair, the grip force was measured (Figure 36A). Within these 4 months the grip force of the left bad hand increased after a delay from around zero to 6kp and of the good right hand from 10 to 11kp (Figure 37). The power improvement in the left bad arm can be seen from the size of the biceps muscle (Figure 36B). Alen was proud of the increase of the biceps because even a girl at school noticed it.
 Figure 36: A. Measuring of hand grip force. B. The increase of size of the biceps muscle in Alen can clearly be seen. Even at school it was noticed.
Figure 36: A. Measuring of hand grip force. B. The increase of size of the biceps muscle in Alen can clearly be seen. Even at school it was noticed.
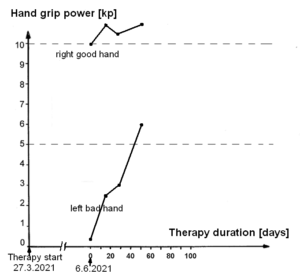
Figure 37: Development of hand grip power of the 12-year-old patient Alen.
Conclusion of the preliminary case report of Alen
Within 6 weeks of non-optimal coordination dynamics therapy, the 12-year-old hemiplegic patient Alen (from Switzerland) learned useful left-hand functions. Again, mainstream medicine failed in prognosis and treatment. Even accidently it could have been found out that some left-hand-functions can be learned by him.
Discussion
Danger of modern euthanasia
There are two main methods for determining voluntary consent: “opt in” (only those who have given explicit consent are donors) and “opt out” (anyone who has not refused consent to donate is a donor). In Germany was is intended to change from the “option in” to the “option out” consent. Since it is a tremendous effort to let not drift a severely brain-injured patient into the permanent coma or brain death (in Manolis 5 years of CDT with 20 hours therapy per week) and nearly no money can be earned, the possibility exists that no big effort is undertaken to bring the patient back to life, but let him die and use then the organs (as for example the kidneys) for other patients. Money can be earned with the transplantation of organs. The possibility of modern euthanasia exists with such a law. The inefficient and 30-years-out-of-date physiotherapy supports this euthanasia because it is that inefficient that in very severe brain injury the pathologic processes win against the physiologic repair mechanisms. The rehabilitation has even problems to diagnose the minimally consciousness state of very severely brain-injured patients [20]. It is therefore not a myth that if I agree to donate my organs, the hospital won’t work as hard and qualified to save my life.
At the 20.9.2021, the Swiss parliament (Ständerat) decided to switch from the “opt in” to the “opt out” system.
Comparison of euthanasia between Hitler-Germany and nowadays
In Germany there was a law discussed in the parliament with which surgeons should be allowed to remove organs from brain-dead-humans or other patients without permission in beforehand. It was stopped mainly for religious reasons. In Hitler-Germany also the church minded that disabled people were killed or used for horrible experiments. The places are given in Figure 3. In this paper, medical facts are presented which makes it likely that, in very severe brain injury, organs are removed from still living patients. The 30-years-out-of-date mainstream medicine with respect to brain repair cannot keep the patients alive and also seems not to be interested to do it. In the newspaper report (Figure 1) it was not mentioned that public prosecutor was interested in the case that a young man was nearly killed when he would have been used as an organ donor.
In times of Hitler Germany, very severely brain-injured patients did not survive because medicine was not advanced sufficiently and treatment was not available to improve CNS functioning in disabled humans. Nowadays first aid and intensive care units are developed further. But the following necessary long-lasting treatment is left out. In Hitler Germany and nowadays priority is given to money and not to the interest of the patient. Further, with respect to brain repair in humans, there is no infrastructure for brain repair. Biological research is no substitute for research on human.
After the times of Hitler-Germany, the great anatomist Pernkopf was punished for being related to euthanasia. He finished the ‘Pernkopf’ anatomy books (including the Figures 5C and 6) in prison. Nowadays, if organs are removed from still living patients (Figure 1) and for sure the patient is dead then, nobody seems to really mind.
To perform research (or treatment) on very severely brain-injured patients is hard work, especially mentally, but the knowledge can be used for other patients with less severe brain injuries.
Further, many permanent coma patients do not have such severe brain injury as the patient Manolis (Figure 16) and can have a meaningful life after brain repair. If for example the ARAS (ascending reticular activating system) network is impaired, the brain is not activated and the patient stays in coma. Most likely, also the ARAS can be repaired through CDT and the patient may even walk out-of-hospital after treatment and has a meaningful live.
Number of patients killed by euthanasia
It is not possible to estimate the number of patients killed through mainstream medicine. If 6 billion people live on earth and it is possible to live longer with a better quality of life for 10 years [20] and every hundreds patient has the mentally discipline to perform CDT, then 6 million human lives are lost per year if a life span of 100 years is assumed (1). How many living patients were used for organ donation and killed in this way is unclear (2). The estimated number of not reported cases will be high. How many patients died or stayed in coma for ever because of no real treatment is also unclear (3).
References
- Schalow G (2002) Stroke recovery induced by coordination dynamic therapy and quantified by the coordination dynamic recording method. Electromyogr. Clin. Neurophysiol. 42:85-104.
- Schalow G (2002) Improvement after traumatic brain injury achieved by coordination dynamic therapy. Electromyogr. Clin. Neurophysiol. 42:195-203.
- Schalow G and Jaigma P (2006) Improvement in severe traumatic brain injury induced by coordination dynamics therapy in comparison to physiologic CNS development. Electromyogr. Clin. Neurophysiol. 46:195-209.
- Schalow G (2003) Partial cure of spinal cord injury achieved by 6 to 13 months of coordination dynamic therapy. Electromyogr. Clin. Neurophysiol. 43:281-292.
- Schalow G, Jaigma P, Belle VK (2009) Near-total functional recovery achieved in partial spinal cord injury (50% injury) after 3 years of coordination dynamics therapy. Electromyogr. Clin. Neurophysiol. 49:67-91.
- Schalow G (2010) Cure of urinary bladder functions in severe (95%) motoric complete cervical spinal cord injury in human. Electromyogr. Clin. Neurophysiol. 50:155-179.
- Schalow G (2019) Regeneration of the human spinal cord via coordination dynamics therapy. Peertechz Publications, 97 eBook.
- Schalow G (2021) CNS repair in a girl with a spinal cord injury. Adv Pub Health Com Trop Med: APCTM-121.
- Schalow G (2006) Cerebellar injury improvement achieved by coordination dynamics therapy. Electromyogr. Clin. Neurophysiol. 46:433-439.
- Schalow G (2021) Cure-like brain-repair in a girl with atrophied cerebellum and pons through Coordination Dynamics Therapy. Adv Pub Health Com Trop Med 123:1-47. ISSN 2691-8803.
- Schalow G, Jaigma P (2005) Cerebral palsy improvement achieved by coordination dynamics therapy. Electromyogr. Clin. Neurophysiol. 45:433-445.
- Schalow G (2006) Hypoxic brain injury improvement induced by coordination dynamics therapy in comparison to CNS development. Electromyogr. Clin. Neurophysiol. 46:171-183.
- Schalow G, Pääsuke M, Ereline J, Gapeyeva H (2004) Improvement in Parkinson’s disease patients achieved by coordination dynamics therapy. Electromyogr. Clin. Neurophysiol. 44:67-73.
- Schalow G, Nyffeler T (2001) Koordinationsdynamik-Therapie: Myelomeningozele (Spina bifida). Physiotherapie.
- Schalow G and Nyffeler T (2000). Koordinatiosdynamik-Therapie: Skoliose. Physiotherapy.
- Schalow G (2013) Human Neurophysiology: Development and Repair of the Human Central Nervous System. Nova Science Publishers, Inc, Hauppauge NY, USA, 734.
- Schalow G (2019) Permanent coma patient re-learned to speak via Coordination Dynamics Therapy. Arch. Clin. Med. Case Rep. 3:33-50.
- Schalow G (2017) Breast cancer growth inhibition via Coordination Dynamics Therapy. In: “Horizons in Cancer Research. Volume 68”. Editor: Hiroto S. Watanabe. Nova Science Publishers, Inc, Hauppauge NY, USA. 125-151.
- Schalow G (2020) Anaplastic oligodendroglioma WHO III brain cancer-patient recovered following operation, radiation and chemotherapy through Coordination Dynamics Therapy, which is also a Covid-19 treatment without ventilator. Int. J. Med. Clin. Imaging 5:165-210.
- Schalow G (2020) To live longer with a better quality of life through coordination dynamics therapy especially in patients with severe brain injury and brain-cancer. Int. J. Med. Clin. Imaging 5:118-155.
- Hodgkin AL, Huxley AF (1952) A quantitative description of membrane current and its application to conduction and excitation in nerve. J. Physiol. 117:500-544.
- Schalow G, Lang G (1987) Recording of Single Unit Potentials in Human Spinal Nerve Roots: a New Diagnostic Tool. Acta Neurochir. 86:25-29.
- Schalow G (2009) The classification and identification of human somatic and parasympathetic nerve fibres including urinary bladder afferents is preserved following spinal cord injury. Electromyogr. Clin. Neurophysiol. 49:263-286.
- Schalow G (2020) Classification and Identification of Human Peripheral Nerve Fibers by Conduction Velocity, Nerve Fiber Diameter and Natural Firing Patterns with Consequences for CNS Repair and Covid-19 Infection Treatment. Int. J. Med. Clin. Imaging. 5:231-314.
- Schalow G (2005) Phase and frequency coordination between neuron firing as an integrative mechanism of human CNS self-organization. Electromyogr. Clin. Neurophysiol. 45:369-383.
- Schalow G (2021) Phase and frequency coordination improvement among neuron firing for improved CNS self-organization and neural repair in Parkinson and spinal cord injury. Int J Med Clin Imaging 6:350-425.
- Schalow G (1993) Spinal oscillators in man under normal and pathologic conditions. Clin. Neurophysiol. 33:409-426.
- Schalow G (2006) Surface EMG- and coordination dynamics measurements-assisted cerebellar diagnosis in a patient with cerebellar injury. Electromyogr. Clin. Neurophysiol. 46:371-384.
- Schalow G (2005) Tremor in Parkinson’s disease patients can be induced by uncontrolled activation and uninhibited synchronization of α2-motoneuron firing to which α1-motoneuron firing synchronizes. Electromyogr. Clin. Neurophysiol. 45:393-406.
- Schalow G (2021) Phase and frequency coordination improvement among neuron firing for improved CNS self-organization and neural repair in Parkinson and spinal cord injury. Int J Med Clin Imaging 6:350-425.
- Schalow G (2010) Scientific basis for learning transfer from movements to urinary bladder functions for bladder repair in patients with spinal cord injury. Electromyogr. Clin. Neurophysiol. 50:339-395.
- Kelso JAS (1995) Dynamic Patterns. The Self-Organization of Brain and Behavior. MIT Press, Cambridge.
- Schöner G, Zanone PG, Kelso JAS (1992) Learning as change of coordination dynamics: Theory and experiment. Journal of Motor Behavior 24:29-48.
- Zanone PG, Kelso JAS (1992) Evolution of behavioral attractors with learning: Nonequilibrium phase transition. Journal of Experimental Psychology: Human perception and Performance, 18:403-421.
- Piper MC, Darrah J (1994) Motor Assessment of the Developing Infant. W.B. Saunders Company.
- Schalow G (2015) Repair of the Human Brain and Spinal Cord. Nova Science Publisher, Hauppauge NY, USA.
- Schnakers C et al. (2009) Diagnostic accuracy of the vegetative and minimally conscious state: clinical consensus versus standardized neurobehavioral assessment. BMC neurology 9:35.
- Kliemann et al. (2019) Intrinsic functional connectivity of the brain in adults with a single cerebral hemisphere. Cell Reports 29:2398-2407.
- Hertz-Pannier et al. (2002) Late plasticity foe language in a child’s non-dominant hemisphere. A pre- and post-surgery fMRI study. Brain 125:361-372.
- Colvis CM, Pollok JD, Goodman RH et al. (2005) Epigenetic mechanisms and gene networks in the nervous system. J Neuroscience 25:10379-10379.
- Deisseroth K, Singla S, Toda H et al. (2004) Excitation-neurogenesis coupling in adult neural stem/progenitor cells. Neuron 42:535-552.
- Koepchen HP (1990) Physiology of rhythms and control systems: An integrative approach. In: Haken H, Koepchen HP editors. Rhythms in Physiological Systems. Berlin. 3-20.
- Lambertz M, Langhorst P (1998) Simultaneous changes of rhythmic organization in brainstem neurons, respiration, cardiovascular system and EEG between 0.05 Hz and 0.5 Hz. J. Auton Nerv Syst. 68:58-77.
- Schalow G (2019) Brain repair and general health improvement through human neurophysiology and repair physiology (Review of Coordination Dynamics Therapy (CDT)). Clin. Med. Rep. 2:1-68.
- Christensen JF, Jones LW, Andersen JL, Daugaard G, Rorth M et al. (2014) Muscle dysfunction in cancer patients. Ann. Oncol. 25:947-958.
- Brown JC, Winters-Stone K, Schmitz KH (2012) Cancer, physical activity, and exercise. Compr. Physiol. 2:2775-2809.
- The Lancet (2004) Cancer survivors: living longer, and now, better. 364:2153-2154.
- Baehr M, Frotscher M (2005) Duus‘ Topical Diagnosis in Neurology. Thieme Verlag, Stuttgart. (a very good book for medical neuroscience since it correlates structure and function in human nervous system injuries; only human neurophysiology is missing).