Epidemiological and genetic aspects in 20 pediatrics patients with Type 1 Diabetes and Celiac Disease
Alejandro Alberto Guouman1*, Patricia Mota4, Zulma Caballero2, Osvaldo Enrique1, Noelia Pegoraro1, Amanda Benitez2, Jorge Zappa2, Marina Karina4, Myriam Medina3
1Servicio de Gastroenterología Infantil, Hospital Pediátrico Avelino Castelan,
2Servicio de Endocrinología y Diabetes,
3Departamento de Docencia e Investigación,
4Servicio de Histocompatibilidad, Hospital Julio Perrando, Resistencia Chaco, Argentina
Received Date: July 16, 2019; Accepted Date: July 22, 2019; Published Date: July 31, 2019
*Corresponding author: Alejandro Alberto Guouman, Servicio de Gastroenterología Infantil, Hospital Pediátrico Avelino Castelan, Resistencia Chaco, Argentina. Email: agudmman@intramed.net
Citation: Guouman AA, Mota P, Caballero Z, Enrique O, Pegoraro N, Benitez A, Zappa J, Karina M, Medina M (2019) Epidemiological and genetic aspects in 20 pediatrics patients with Type 1 Diabetes and Celiac Disease. Adv Endoc and Daib: AEAD-109.
Introduction
The association between Celiac Disease (CD) and type 1 diabetes (DB1) is described and demonstrated for a long time, trying to elucidate the reasons why both diseases occur in the same person, evaluating in depth the clinical, epidemiological and genetic aspects in a group of patients With both diseases, it is interesting from the scientific point of view, since it could provide objective conclusions to define early detection or prevention strategies.
CD and (DB1, share known genetic [1, 2, 3, 4, 5, 6, 7] epidemiological and immunological [8] factors; and probably also factors not yet elucidated so both are considered associated diseases. The triggers of DB1 and EC are not clarified, and it is not clear whether gluten has any relationship with DB1, although there is a bibliography that tries to prove it [9].
Objective
To define the moment of diagnosis of both diseases and establish a risk gradient in relation to the HLA-DQ, comparing our patients (with CD and DB1) with a control group in our population [10], of a work previously carried out in our province, and defining the consequent appearance between both diseases.
Material and Method
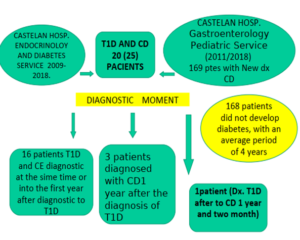
Retrospective and transversal work, evaluating patients with diagnosis of both diseases in our institution during a period of 10 years, (2009-2018), considering in both, date of diagnosis and genetic study, from information (database) of Children’s Gastroenterology Services ( 2011-2018) and Children’s Endocrinology Service (2009-2018) from our Pediatric Hospital.
The diagnosis of DB1 was made according to the criteria of the ADA (AMERICAN DIABETES ASSOCIATION), and of EC according to the classic criteria (2009 to 2011) and according to the criteria of the European Society of Gastroenterology, Hepatology and Pediatric Nutrition (ESPGHAN) (from 2012 to date).
We studied 20 pediatric patients with DB1 and EC 13 women and 7 men. Average age 8 years. 193 healthy adults as control group 101 women and 92 men. Average age 42 years.
HLA typification
DNA extraction was performed with QIA amp Blood Mini Kit Kit Qiagen. The alleles of the DQB and DQA loci were determined using generic amplification by polymerase chain reaction (PCR) and reverse hybridization with specific oligonucleotides (LIPA KEY-INNOGENETICS) and analyzed with LIPA Software.
Statistical analysis
The degree of association of an allele between patients and controls was expressed in odds ratio (OR), which was calculated using Wolf’s formula. The p value was determined according Yates correction or the Fisher exact test with two tails when one of the samples was less than 5. A p value ≤0.05 was considered significant.
Results
Of the 20 patients found with CD and DB1 during this period, in 16 cases the diagnosis was made simultaneously with the debut of DB1, in 3 patients the diagnosis of CD was later than that of DB1 (but within the 1st subsequent year to the diagnosis of DB1, and with the 1st study of antibodies requested to the patients); and in one patient the diagnosis of diabetes at one year and two months after the diagnosis of CD (over 169 patients diagnosed of CD in our institution in a period of 8 years (2011-2018).
Regarding the HLA obtained in the 20 patients with DB1 and CD, 75% (N 15) of the patients had double dose DQ2, double dose DQ8 or DQ2 / DQ8. In the remaining 5 patients, 2 were DQ2 in single dose and 3 DQ8 in single dose. We did not have patients with DQ2.2, nor DQ7.

DQX: DQ molecule other than DQ2, DQ8 and DQ7, p < 0,05 was considered statistically significant. NS: No significant
Conclusions
The diagnosis of both diseases was made simultaneously, at the debut of their DB1 (80%).168 of 169 patients diagnosed with CD did not develop DB1 after starting the gluten-free diet, witha mean follow-up of 4 years, despite having the genetic risk.The presence of double doses of DQ2.5 or double doses of DQ8 molecules or DQ2.5 / DQ8phenotype in 75% of patients with CD and DB1 indicates the high risk of developing bothdiseases. (P< O.O5)The absence of the DQ7 molecule makes us wonder if it confers protection to the development of diabetes.
References
- Cudworth AG, Woodrow JC (1974) Letter: HL-A antigens and diabetes mellitus. Lancet 2:1153.
- Sharma B, Nehara HR, Saran S, Bhavi VK, Singh AK, et al. (2019) Coexistence of Autoimmune Disorders and Type 1 Diabetes Mellitus in Children: An Observation from Western Part of India. Indian Journal of Endocrinology and Metabolism 23: 22-26.
- Vajravelu ME, Keren R, Weber DR, Verma R, De león DD, et al. (2018) Incidence and risk of celiac disease after type 1 diabetes: A population-based cohort study using the health improvement network database.Pediatric Diabetes 19: 1422-1428.
- Shahramian I, Bazi A, Sargazi A (2018) An Overview of Celiac Disease in Childhood Type 1 Diabetes. International Journal of Endocrinology and Metabolism 16: e66801.
- Verdu EF, Danska JS (2018) Common ground: shared risk factors for type 1 diabetes and celiac disease Nature Immunology 19: 685-695.
- Redondo MJ, Steck AK, Pugliese A (2018) Genetics of type 1 diabetes. Pediatric Diabetes 19: 346-353.
- Leonard MM, Camhi S, Kenyon V, Betensky RA, Sturgeon C (2019) Targeted genotyping for the prediction of celiac disease autoimmunity development in patients with type 1 diabetes and their family members. World Journal of Diabetes 10: 189-199.
- Haupt-Jorgensen M, Holm LJ, Josefsen K, Buschard K (2018) Possible Prevention of Diabetes with a Gluten-Free Diet. Nutrients 10: E1746.
- MottaPatricia, López María de los Angeles, Guouman Alejandro, Pegoraro Noelia, Enríquez Osvaldo, Marinic Karina Genotipos HLA-DQ yriesgo de Enfermedad Celiaca en población pediátrica de Chaco, Argentina. Simposio Panamericano de Enfermedad Celiaca, junio 2018.
