Endoscopic Balloon Dilatation for Treatment of Congenital Antral Web: A Case Series
Estefanía Carrión-Jaramillo1*, Andrea Vásconez-Montalvo2, Fabián Vásconez-Muñoz3, Camila Borrero-Cruz1
1Pediatrics Department, Hospital Metropolitano de Quito, Ecuador
2Medical Doctor, Pontificia Universidad Católica del Ecuador, Ecuador
3Pediatric Gastroenterology Department, Hospital Metropolitano de Quito, Ecuador
Recieved Date: 11 July, 2019; Accepted Date: 16 July, 2019; Published Date: 24 July, 2019
*Corresponding author: Estefanía Carrión-Jaramillo, Pediatrics Department, Hospital Metropolitano de Quito, Ecuador. Tel: +593984620532; Email: estefania.carrionj@gmail.com
Citation: Carrión-Jaramillo E, Vásconez-Montalvo A, Vásconez-Muñoz F, Borrero-Cruz C (2019) Endoscopic Balloon Dilatation for Treatment of Congenital Antral Web: A Case Series. Cr Res in Gastro and Hep: CRGH-102.
Abstract
Prepyloric antral webs are an infrequent cause of gastric outlet obstruction in infants and children. For this reason it is a commonly misdiagnosed condition. The main symptoms are non-bilious persistent vomiting, abdominal pain, weight loss, failure to thrive and refusal to feed. The treatment for congenital antral web is either surgical or endoscopic. We present 3 cases of children (2 males and 1 female) diagnosed of congenital antral web, all of them were successfully treated with endoscopic balloon dilatation (EBD). The procedure was well-tolerated and the symptoms resolved after EBD with a significant decrease in the length of stay.
Keywords: Congenital antral web; Endoscopic balloon dilatation; Gastric outlet obstruction; Upper gastrointestinal tract; Conservative treatment
Introduction
Congenital antral webs are thin circumferential mucous membranes that are usually found 1-2 centimeters proximal to the pylorus and narrow the gastrointestinal lumen. Its projection is perpendicular to the long axis of the antrum. It is an uncommon cause of gastric outlet obstruction in infants and children, with an incidence of 1 in 100,000 births [1, 2].
Clinical manifestations may vary according to the degree of obstruction. Central apertures of less than 1 cm can cause significant symptoms [3]. The main manifestation is persistent non-bilious projectile vomiting. Other reported symptoms, especially in older children are; abdominal pain, early satiety, refusal to feed and weight loss [4]. Significant associated anomalies (gastrointestinal and cardiovascular) are seen in about 30 % of children with an antral web [5].
Antral webs are commonly misdiagnosed or the diagnosis is delayed as physicians pursue more prevalent diagnoses. The diagnosis is established with an upper gastrointestinal series in up to 90% of the cases [3]. Upper endoscopy has also significant diagnostic value; finding a small fixed central aperture with no changes of its diameter with peristalsis as the gastric wall contracts normally [5]. Some patients are diagnosed in adulthood mainly in incomplete antral webs [2].
Endoscopic balloon dilatation is a relatively new technique for management of prepyloric antral webs that is more conservative and is as efficient as surgical myotomy. EBD is a safe procedure without the need for further surgical interventions [1]. Also feeding tolerance is achieved shortly after the procedure and therefore a reduction in the length of stay is expected in these patients.
Methodology
We retrospectively gathered the children that presented congenital antral web that were treated with endoscopic balloon dilatation. As the study was retrospective it was not necessary to obtain informed consent from the legal tutors. Data were extracted from clinical files and with no intervention in the patient at the moment.
The inclusion criteria were pediatric patients diagnosed of congenital antral web and treated with EBD from 2014-2019 in Hospital Metropolitano de Quito-Ecuador by the Pediatric Gastroenterology Department. We encountered 6 patients with a diagnosis of antral web and included 3 patients treated with EBD for this condition.
The main objective was to evaluate if this technique was well tolerated and how long after the procedure patients experienced relief of symptoms. Also, the length of stay after the procedure was noted. The main characteristics of the patients and their treatment are resumed in (Table 1). Male 3 y 8 m Female 11 2: Prepyloric antral web with a central aperture of 8 mm of diameter Male 3 y 2: Esophagitis, prepyloric antral web with a central aperture of 5 mm
Patient
Symptoms
Endoscopic findings
Follow up
N. of EBD
Length of stay
1
Vomiting, weight loss
Peptic esophagitis, circumferential antral web at the antrum with a central aperture of 3 mm of diameter
The patient remained asymptomatic immediately after EBD. No need for another EBD
1
24 hours after the procedure
2
Vomiting, abdominal pain
1: Peptic esophagitis, circumferential web at the prepyloric antrum with a central aperture of 6 mm of diameter
After 1 month of the first EBD, patient experienced early satiety and abdominal discomfort. A second EBD and remained asymptomatic since.
2
24 hours in the first EBD, ambulatory in the second EBD
3
Vomiting, hematemesis, and weight loss
1: Peptic esophagitis, circumferential web at the prepyloric antrum with a central aperture of 2 mm
Immediate relief of symptoms after first EBD with adequate weight gain. After 2 weeks postprandial sporadic vomiting, a second EBD was performed and patient remained asymptomatic since.
2
24 hours in the first EBD, ambulatory in the second EBD
Case Report
Patient 1
A 3 year 8 month old boy, with no previous diseases and a history of 15 days of postprandial non-bilious vomiting after every meal that was accompanied by weight loss and refusal to feed. He had received ibuprofen 15 days earlier for an acute gastroenteritis. He consulted the outpatient clinic of Pediatric Gastroenterology of Hospital Metropolitano de Quito-Ecuador and indicated that 24 hours earlier he had projectile vomiting. The physical exam was unremarkable. The first study performed was an upper GI series which found a dilated stomach with abundant gastric content.An upper endoscopy was performed at Hospital Metropolitano de Quito-Ecuador with an Olympus GIF- HQ 190 (9.9 mm of external diameter) finding peptic esophagitis and an antral web with a central aperture of 3 mm that did not allow the pass of the endoscope. A ballon dilatation was performed with different sized balloons from 10 mm to 15 mm with an adequate expansion of the antral web. No other strictures were evidenced. The pylorus and duodenum were normal. The patient only underwent 1 procedure and he initiated oral feeding 6 hours after EBD with satisfactory response and without incidental injuries. The procedure lasted 1 hour 25 minutes. He was started with PPI for 6 weeks and Sucralfate for 1 week. He attended the follow-up consultation a week after the procedure and he had gained weight and tolerated oral intake well. He has remained 5 years without any symptoms (Figure 1 A, B, C, D, E, F).
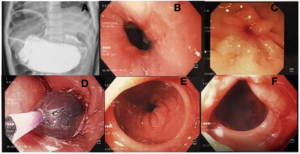
Figure 1 A, B, C, D, E, and F: upper GI series with gastric dilatation with delay in gastric emptying. B: Esophagus with signs of esophagitis. C: Circumferential antral web with central aperture before EBD. D: EBD. E: Dilated antral web and pylorus. F: Final outcome.
Patient 2
An 11 year old girl remitted from another center with a history of 1 month of projectile non-bilious vomiting and colicky abdominal pain. The patient underwent barium study of an upper gastrointestinal series, which revealed pyloric syndrome probably secondary to an inflammatory process. She had an upper endoscopy with the diagnosis of pyloric syndrome and peptic esophagitis and started a treatment with PPI and sucralfate. Despite the treatment, the vomiting was persistent. Therefore, she consulted the outpatient clinic of Pediatric Gastroenterology of Hospital Metropolitano de Quito-Ecuador. Another upper endoscopy was performed in our center finding esophagitis and a circumferential web at the prepyloric antrum with a central aperture of 6 mm of diameter, for which a balloon dilatation was performed. Initially, an Olympus GIF- HQ 190 (9.9 mm of external diameter) was inserted evidencing the antral web that could not be passed to the duodenum. Endoscopic re-examination with the Olympus GIF XP180N (5.5 mm of external diameter) was inserted through the aperture evidencing pylorus and duodenum of normal aspect. No other strictures were found. EBD was attempted using different sized balloons (14mm and then to 17 mm) achieving successful expansion of the antral web, no incidental injuries were observed. The procedure lasted 1hour 10 minutes. The patient tolerated the procedure adequately and started food tolerance 6 hours after EBD. She remained asymptomatic and was discharged the next day. She received PPI for 6 weeks and Sucralfate for 5 days. Three weeks after the first EBD, she attended the Pediatric Gastroenterology outpatient clinic for early satiety and abdominal discomfort. An upper endoscopy was programmed evidencing the antral web with a central aperture of 8 mm and proceeded to perform another EBD achieving dilatation of up to 20 mm with satisfactory results, the procedure was ambulatory and lasted 25 minutes. The patient has remained asymptomatic for a year and 3 months and no other dilatations were required. (Figure 2 A, B, C, D, E, F).
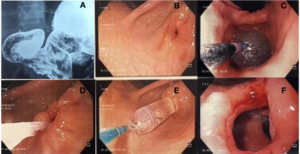
Figure 2 A, B, C, D, E, F: upper GI series with gastric dilatation with delay in gastric emptying. B: Circumferential antral web with central aperture before EBD. C: First EBD. D: Follow up endoscopy antral web aperture is wider 8mm. E: Second EBD. F: Final outcome.
Patient 3
A 3 year old boy, who was admitted in two different centers for non-bilious unenforceable vomiting and weight loss in the last month. He had received IV fluids and was discharged without a clear diagnosis. Two weeks after being discharged, he remained at home with sporadic vomiting and in the last 48 hours he presented hematemesis and consulted Hospital Metropolitano de Quito-Ecuador. An upper endoscopy was performed in our center with an Olympus GIF- HQ 190 (9.9 mm of external diameter) finding peptic esophagitis with an ulcer covered with fibrin and a circumferential web at the prepyloric antrum with a central aperture of 2 mm of diameter, therefore a balloon dilatation was performed using balloons from 11mm up to 15 mm achieving successful dilatation of the antral web, no incidental injuries were evidenced. The patient tolerated the procedure and he started oral tolerance 6 hours after with an adequate response. The procedure duration was 1 hour 10 minutes. He was started on PPI for 6 weeks and received sucralfate for 1 week. He was discharged 24 hours after the procedure. Three weeks later he attended the outpatient clinic of Pediatric gastroenterology with an adequate weight gain but the parents referred sporadic vomiting in the last week, so another upper endoscopy was performed finding a stricture at the same level and a EDB was performed with a balloon of 15 mm, the procedure was ambulatory and lasted 50 minutes. He maintained the PPI therapy for 8 weeks. After the second EBD the patient has remained asymptomatic for 7 months (Figure 3 A, B, C, D, E, F).

Figure 3A, B, C, D, E, F: Circumferential antral web with central aperture 2 mm before EBD. B: First EBD. C: outcome after first EBD. D: Follow up endoscopy antral web aperture is wider 5 mm. E: Second EBD. F: Final outcome.
Discussion
Prepyloric antral webs should be considered in the differential diagnosis in persisting vomiting in newborns, infants and children. Even if it is an uncommon cause of gastric outlet obstruction the symptoms might be very severe, as it has been described that distal obstruction can lead to neonatal gastric perforation [6]. Most patients reported in literature have experienced delayed diagnosis or have been treated for other conditions for long periods before the diagnosis [2, 3, 4]. Our patients experienced symptoms for 15 -30 days before diagnosis.
It has been described that the most frequent manifestation is non-bilious projectile vomiting; this was also evidenced in all of the subjects. The second most common symptom was weight loss that was experienced in 2 patients. One patient presented with abdominal pain which is compatible with reports of other symptoms that might be encountered in older children [4]. None of the patients presented symptoms before and this could lead to a delayed diagnosis, the eldest person reported to be diagnosed with antral web was 78 years old [11].
The diagnose can be made with upper GI series and/or endoscopy [1]. In the GI series, an image of a double-bulb can be observed, caused by the normal duodenal bulb with a proximal antral chamber between the web and the pylorus [3]. This finding was unclear in our patients, only 2 of them underwent upper GI series before the endoscopy. An upper endoscopy was performed in all our patients that were both diagnostic and therapeutic. Endoscopy is often required to confirm the diagnosis of gastric outlet obstruction and identify the specific etiology accompanied by a therapeutic assistance [7].
Endoscopic findings in all the patients were peptic esophagitis, one of them had esophageal ulcers. The circumferential antral webs found in the subjects had central apertures of 2-6 mm of diameter. It has been reported that symptoms are frequent when the antral web has an aperture of less than 1 cm [2].
After the diagnosis is established the treatment for these patients could be surgical or endoscopic. Surgical resolution consists in gastrectomy or excision of the membrane with pyloroplasty and it is the election treatment for patients with special anatomic considerations (thickness of the web, size of the aperture, degree of obstruction) and in premature babies or neonates with a weight of under 2 kg [1]. Therapeutic endoscopy can also be a recommended treatment, one option is endoscopic balloon dilatation that is a relatively new technique which is less invasive and is as efficient as surgery [2, 3]. EBD has become the first-line therapy in patients with benign causes of gastric outlet obstruction [7].
There are different criteria on an adequate endoscopic balloon dilatation end point; some have used balloons of up to 15 mm by most physicians. Balloons over 15 mm are not frequently used. In our patients 2 that were 3 years old, the balloon used for their EBD was 10-15 and in the older child the balloons used were 14-17 mm and in the second EBD the used balloons were up to 20 mm [7].
When comparing both procedures, considering that both treatments are efficient, EBD is a safe intervention without further need of surgery and is well tolerated as we could appreciate in our patients [1, 2, 3]. Tunell and Smith reported that 5 out of 7 patients with congenital antral webs that were treated with surgery experienced vomiting postoperatively. The patients in our study remained asymptomatic immediately after the procedure, this supports the statement that the procedure is well tolerated and the relief of symptoms is experienced shortly after EBD [8]. Another positive aspect of EBD is that patients initiate oral feeding sooner than patients that undergo surgical treatment and this reduces the length of stay, after some gastrointestinal interventions early feeding might not be adequate because of postoperative ileus and dysmotility secondary to intraoperative manipulation. New meta-analyses showed benefits on early post-operative nutrition with reduction of complications, but this is not possible after a gastrectomy. In any case, early feeding reduces the length of stay [9]. The patients in our study started oral intake 6 hours after EBD with an adequate tolerance and the subjects stayed 24 hours after the procedure. In the case in which the second EBD was needed it was an ambulatory procedure. Nowadays, EBD is an adequate alternative for treating gastric outlet obstruction secondary to congenital antral web, most patients with this condition can be benefited with this procedure but anatomical considerations should be taken into account in order to select patients correctly.
Morales et al. indicated in their study that adult patients with gastric outlet obstruction underwent repeated sequential balloon dilations and/or needle-knife incisions with steroid injection for alleviation of the obstruction [10]. This is consistent with our patients because 2 of them required a second EBD due to relapsing symptoms, after the second procedure they had a favorable evolution. Another study indicated that patients treated with EBD for antral webs require multiple treatment courses with only transient improvement in symptoms. Two subjects in our study needed further EBD but after the second procedure both patients remained symptomatic and there was no need for surgical resection [12].
Conclusion
Patients underwent endoscopic balloon dilatation with no complications it is a procedure that was very well tolerated, with minor or no pain after EBD and patients could start early feeding (6 hours after the procedure). Endoscopic balloon dilatation has not been widely applied in children as it is not a common condition but in selected patients it could be the election treatment. Even when endoscopic balloon dilatation is safe and efficient it has limitations and certain patients could be eligible for surgery instead of EBD, mainly in patients with anatomic considerations.
Further studies are needed in order to evaluate EBD as the first-line treatment for antral webs. The sample size was small as this in an infrequent condition.
References
- Peck J, Khalaf R, Marth R, Phen C, Sosa R, et al. (2018) Endoscopic Balloon Dilation for Treatment of Congenital Antral Web. Pediatric Gastroenterology Hepatology and Nutrition 21: 351-
- Lu JP, Huang Y, Wu J, Chen SY (2014) Uncommon congenital antral web misdiagnosed twice as pyloric ulcer: successful treatment with endoscopic balloon dilatation. The Turkish Journal of Pediatrics 56: 100-102.
- Lui KW, Wong HF, Wan YL, Hung CF, Ng KK, et al. (2000) Antral web: a rare cause of vomiting in children. Pediatric Surgery International 5: 424-425.
- Noel RJ, Glock MS, Pranikoff T, Hill ID (2000) Nonobstructive Antral Web: An Unusual Cause of Excessive Crying in an Infant. Journal of Pediatric Gastroenterology and Nutrition 31: 439-441.
- Antao BA, Lane VA (2017) Congenital Gastric Anomalies. pp 1337-1351.
- Byun J, Kim HY, Noh SY, Kim SH, Jung SE, et al. (2014) Neonatal gastric perforation: a single center experience. World Journal of Gastrointestinal Surgery 6: 151-155.
- Chao HC (2016) Update on endoscopic management of gastric outlet obstruction in children. World J Gastrointest Endosc 8: 635-645.
- Tunell WP, Smith EI (1980) Antral Web in Infancy. Journal of Pediatric Surgery 15: 152-155.
- Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, et al. (2017) ESPEN guideline: Clinical nutrition in surgery. Clinical Nutrition 36: 623-650.
- Morales SJ, Nigam N, Chalhoub WM, Abdelaziz DI, Lewis JH, et al. (2017) Gastric antral webs in adults: A case series characterizing their clinical presentation and management in the modern endoscopic era. World J Gastrointest Endosc 9: 19-25.
- Nissan A, Seror D, Udassin R (1997) Gastric outlet obstruction caused by prepyloric mucosal diaphragm mimicking duodenal ulcer: a case report. Acta Pediatrica 86: 116-118.
- Amin R, Martinez AM, Arca MJ (2019) Diagnosis and treatment of gastric antral webs in pediatric patients. Surgical Endoscopy 33: 745-749.
