Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Efficacy and Safety of Expanded Stem Cell Therapy and Platelet-Rich Plasma in Partial Knee Replacement: A Case Report
Hassan Mubark*
Rheumatologist, Institution: Auckland Regenerative Clinic, Ormiston Specialist Centre, Auckland
Received Date: March 30, 2022; Accepted Date: April 04, 2022; Published Date: April 08, 2022
*Corresponding author: Hassan Mubark, Rheumatologist, Institution: Auckland Regenerative Clinic, Ormiston Specialist Centre, 125 Ormiston Road, Flat Bush, Auckland 2019, New Zealand. Phone: +64 9 2713305; Mobile: +64 21843513; Fax: +64 9 2770769; Email: drhassanmubark@gmail.com
Citation: Mubark H (2022) Efficacy and Safety of Expanded Stem Cell Therapy and Platelet-Rich Plasma in Partial Knee Replacement: A Case Report. Adv Ortho and Sprts Med: AOASM-163.
DOI: 10.37722/AOASM.2022013
Abstract
This article aims to address the effectiveness and safety of intra-articular regenerative medicine in the partially replaced knee joint to slow or stop the progression of other compartments from developing florid knee osteoarthritis (OA).
Knee OA is the most common degenerative joint disease, followed by the hip joint and first carpometacarpal joint.
The knee joint comprises three compartments: medial, lateral, and patellofemoral. The medial and patellofemoral (PF) compartments are more commonly involved in the degenerative process.
Chondromalacia patella (CMP) is an indisposition of the hyaline cartilage layer of the articular surfaces of the bone. It results in the softening and consequent fissuring, tearing, and erosion of hyaline cartilage. Chondromalacia is often linked with microtrauma leading to wear and tear of the patellofemoral cartilage. Lateral positioning of the patella in the PF joint is a frequent cause of chondromalacia. Females are affected more than males due to increased Q angles in women. CMP usually progresses to premature PF osteoarthritis.
This article presents a fifty-five-year-old female patient who suffered bilateral knee pain since the age of 13; she failed to respond to conservative treatment and bilateral knee ligament release and subsequently bilateral hemiarthroplasty of the PF joints at the age of 48. Three years later, she developed continuous bilateral medial knee pain with functional impairment suggestive of OA with a right knee x-ray that revealed mild narrowing of the right knee joint space. She continued conservative treatment until age 55 and then elected regenerative medicine to treat her symptoms and avoid further surgical intervention. She underwent bilateral intra-articular platelet-rich plasma (PRP) combined with soluble hyaluronic acid (HA), and she had a reasonable response. She proceeded for autologous fat-derived expanded mesenchymal stem cell (MSC) therapy four months later; this was combined with PRP and HA as scaffolding techniques. The two treatments were associated with dramatic response in controlling the pain score and improving her quality of life. Her knee pain returned as she continued hard physical work, and repeat x-rays showed normal knee joint spaces compared to a baseline performed three years ago. She elected for a booster maintenance dose.
We predict from this case that intra-articular regenerative therapy of all kinds, including MSCs, PRP, and HA, is an effective and safe option in hemiarthroplasty for managing the other compartments on the joint. This therapy can be repeated multiple times with no harm.
Introduction
Osteoarthritis (OA) is a degenerative joint disease, and it is the most common type of arthritis; the knee joint is typically involved. Pathological processes in OA joint include osteophytes formation, subchondral bone thickening, variable grades of synovial inflammation, degeneration of menisci and ligaments of the knee joint, capsule thickening, and hypertrophy resultant in progressive articular cartilage destruction and reduction of joint space [1]. The etiology of OA is multifactorial and includes articular injury, aging, overweight, and heredity [2, 3].
Chondromalacia patella (CMP) is an indisposition of the hyaline cartilage layer of the articular surfaces of the bone. It results in the softening and consequent fissuring, tearing, and erosion of hyaline cartilage. The Q angle is the dimension of the pull of the quadriceps muscle compared to the force of the patella tendon on the patella [4]. The Q angle is more significant in females due to a wider pelvis than in males. An abnormally high Q angle signals lateral pull of the patella in the trochlear groove of the femur and a process of articular cartilage wear and tear.
CMP often leads to premature patellofemoral (PF) compartment OA and possible early hemiarthroplasty. Once the OA process starts then can be transferred to the other compartment, particularly the medial articular side.
We are trying to find some non-surgical techniques to protect patients from surgical intervention as much as possible with evolutionary medicine. Multiple randomized controlled trials revealed the positive influence of mesenchymal stem cells (MSCs) in OA [5,6,7]. Our article effectively and safely used regenerative medicine of combined expanded MSCs with platelet-rich plasma (PRP) and soluble hyaluronic acid (HA).
We use MSCs' specialized laboratory (lab) expansion method to get many MSCs; we harvest abdominal fatty tissue from the patient. The lipo-aspirate gets washed and then digested with 0.2 U/mL collagenases. The stromal vascular fraction (SVF) is separated from the digested adipose tissue through density centrifugation and then plated down and cultured using Dulbecco's Modified Eagle Medium. Cells grow to high confluency over six weeks or longer and then cryopreserved until injection time. The lab then measured the cell count manually and confirmed it with a hemocytometer, and the viability gets measured by trypan blue exclusion dye. We prepare the autologous PRP, which has several growth factors and functional proteins, using sterile tubes with anti-coagulation in an office centrifuge to make a fresh sample of PRP after good blood separation. We mix the PRP with the expanded MSCs in the same syringe; sometimes, we add soluble HA for additional scaffolding.
Case Presentation
In a fifty-five-year-old female patient who had suffered bilateral knee pain since the age of 13, the left side was worse than the right. Her condition progressed badly, which required left knee ligament release at the age of 20, followed by bilateral knee ligament release at 25. While her job working at the airport needs her to be on her feet for several hours a day, leading to ongoing knee pains. The orthopaedic surgeon recommended high tibial osteotomy when she was 43 years of age; she declined the operation. At 46, she underwent left PF hemiarthroplasty, then right PF replacement at 48. The outcome was good until three years later when she developed bilateral medial knee pains typical of medial compartment OA symptoms. Her pain was about 3/10 on the visual analog scale (VAS), continuous, particularly on movement; thus, she quit her physical job to do only admin work; she could not climb stairs and used the chair arms as a support to stand up. She used regular paracetamol, codeine phosphate, anti-inflammatory medicine, and night-time amitriptyline. She found it hard to bend due to the quadriceps disuse atrophy. She heard knee noises with the movement, and we confirmed crepitus on physical examination but no joint swelling. Pre-therapy X-rays revealed normal left medial and lateral compartments, while the right knee revealed mild narrowing of the medial and lateral compartments (Figure 1).
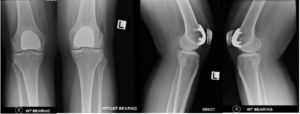
Fig 1: x-ray knees show pre-stem cell therapy reasonable medial and lateral joint spaces with patellofemoral hemiarthroplasty
She elected for a regenerative medicine trial to treat her symptoms and try to avoid further surgical intervention. At 55, she underwent bilateral knee intra-articular platelet-rich plasma (PRP) combined with soluble hyaluronic acid (HA). We prepared the PRP by taking 40 MLS of blood from her and place it in sterile ACD-A tubes and Regen tubes with combined PRP gel and HA. The tubes were centrifuged for eight minutes with good separation; the total fluid injected in each knee was 8 MLS containing 40 mg of HA with PRP and injected medially in each knee under ultrasound guidance. While She had a reasonable response within a short period, she proceeded to the fat harvesting mesenchymal stem cell (MSC) process; after informed consent, a qualified general surgeon harvested around 50 grams of abdominal adipose tissue. The lipo-aspirate was washed and then digested with 0.2 U/mL collagenases. The stromal vascular fraction (SVF) was separated from the digested adipose tissue through density centrifugation. The SVF was plated down and cultured using Dulbecco's Modified Eagle Medium (DMEM) and 10% human platelet lysate (HPL) to expand the MSCs population. Cells were grown to 90% confluency over six weeks and then cryopreserved until injection. During the lab process The MSCs get purified, sterilized with antimicrobial/antifungal agents, and expanded according to an approved protocol. Injections were prepared on the date of treatment. The cells were washed and filtered before being resuspended in Hartmann's solution with 10% HPL in syringes for administration. Cell count was measured manually and confirmed by a hemocytometer, and the viability was measured by trypan blue exclusion dye. Four months after the PRP injections, she underwent ultrasound-guided bilateral medial knee implantations with expanded MSCs in a dose of 60 x 106 combined with PRP and soluble HA with a total volume of 8 MLS injected under ultrasound-guidance in each knee. The PRP and HA used in the stem cell technique were like the previous standard procedure. As prophylactic antibiotics, we have prescribed her amoxicillin/clavulanic acid three times daily for one week following the intra-articular injections to avoid a low risk of prosthesis infection.
She responded well to the MSC therapy and dramatic knee pain control. The VAS went down to 0/10; she hardly needed analgesics with improved activities of daily living. She returned to physical work, stairs climbing, and she could get off the chair with no assistance. She felt more assertive in her quadriceps and able to bend normally. She had no more crepitus. While she continued to work around 12 hours a day in her supermarket, she developed knee pains, and the repeat x-ray of the knees three years post a baseline X-ray was unremarkable (Figure 2). She elected for a booster dose of MSCs with PRP to maintain her early clinical diagnosis of medial OA. Both PRP-HA and MSCs-PRP-HA therapies did not cause any infection or other complications.
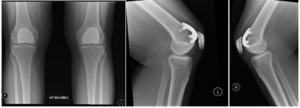
Fig 2: shows three-year post-stem cell therapy with normal medial and Lateral knee joint spaces with stable prosthesis
Discussion
MSCs are being examined in several research resources and clinical attempts to verify effectiveness and safety [8,9,10]. Corticosteroid injection is not recommended for post knee replacement to avoid the risk of prosthesis infection [11]. MSC therapy combined with surgical arthroplasty has been tried safely and effectively [12]; the safety may be attributed to the antimicrobial activities of both PRP and MSCs [13,14].
In our patient, we demonstrated the safe and effective use of intra-articular PRP with soluble HA in the first procedure, and then we performed the second procedure using MSCs together with PRP and HA. Additionally, there was no joint infection or other complications. This was reassuring in helping the patient's symptoms, improving quality of life, and maintaining good joint spaces. We recommend cautionary practice of post injections prophylactic antibiotics when injecting a prosthetic joint with any regenerative solution. At the same time, that is not the standard practice in the native joint.
Our patient showed a good response to the MSC therapy with no degenerative progression of the other joint compartments; thus, she was encouraged to proceed with a booster dose to avoid total knee replacement. The MSCs can be stored for many years; hence, further MSC therapies can be tried if needed safely.
Conclusion
We predict from this case that intra-articular regenerative therapy is an effective and safe option in hemiarthroplasty for managing osteoarthritis in the other compartments of the joint. We need to confirm our findings in large randomized controlled trials. We recommend a short course of antibiotics as a caution in hemiarthroplasty despite the antimicrobial nature of both autologous expanded mesenchymal stem cells and platelet-rich plasma.
Competing Interests: The author has declared that no competing interests exist.
References
- Chen D, Shen J, Zhao W, Wang T, Han L, et al. (2017) Osteoarthritis: toward a comprehensive understanding of pathological mechanism. Bone Res 5: 16044.
- Krasnokutsky S, Samuels J, Abramson SB (2007) Osteoarthritis in 2007. Bull NYU Hosp Jt Dis 65: 222-228.
- Loeser RF, Goldring SR, Scanzello CR (2012) Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum 64: 1697-1707.
- Chaudhary S, Jain S K, Sharma N, et al. (January 16, 2022) Analysis of Predictors Affecting Biomechanical Function of the Knee Joint and Its Relation to Anterior Knee Pain. Cureus 14: e21305. doi:10.7759/cureus.21305
- Han X, Yang B, Zou F, Sun J (2020) Clinical therapeutic efficacy of mesenchymal stem cells derived from adipose or bone marrow for knee osteoarthritis: a meta-analysis of randomized controlled trials. J Comp Eff Res 9: 361-374.
- Pas HI, Winters M, Haisma HJ, Winters M, haisma JH, et al. (2017) Stem cell injections in knee osteoarthritis: a systematic review of the literature. Br J Sports Med 51: 1125-1133.
- Kim SH, Ha CW, Park YB, Nam E, Lee JE, et al. (2019) Intra-Articular injection of mesenchymal stem cells for clinical outcomes and cartilage repair in osteoarthritis of the Knee: A meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 139: 971-980.
- Brown MH, Scholes C, Hafsi K, Marenah M, Li J, et al. (2019) Efficacy and safety of culture-expanded, mesenchymal stem/stromal cells for the treatment of knee osteoarthritis: a systematic review. J OrthopSurg Res 14: 34.
- Centeno CJ, Al Sayegh H, Freeman MD, Smith J, Murrell WD, et al. (2018) A multi-center analysis of adverse events among two thousand, three hundred and seventy-two adult patients undergoing adult autologous stem cell therapy for orthopaedic conditions. Int Orthop 40: 1755-1765.
- Bastos R, Mathias M, Andrade R, Raquel Bastos, Alex Balduino, et al. (2018) Intra-Articular injections of expanded mesenchymal stem cells with and without addition of platelet-rich plasma are safe and effective for knee osteoarthritis. Knee Surg Sports TraumatolArthrosc 26: 3342- 3350.
- Cheppalli NS, Singanamala N, Choi T J, Anand A (2021) Intra-Articular Corticosteroid Injection After Total Knee Replacement: Is it Safe?.Cureus 13(11): e19700. doi:10.7759/cureus.19700
- Freitag J, Wickham J, ShahK, Douglas Li, Norsworthy C, et al. (2020) Mesenchymal stem cell therapy combined with arthroscopic abrasion arthroplasty regenerates cartilage in patients with severe knee osteoarthritis: a case series. Regen Med 15: 1957-1977.
- Drago L, Bortolin M, C ,Taschieri S, Fabbro MD (2013) Antimicrobial activity of pure plateletrich plasma against microorganisms isolated from oral cavity. BMC Microbiology volume 13: 47.
- Alcayaga-Miranda F, Cuenca J, Khoury M (2017) Antimicrobial Activity of Mesenchymal Stem Cells: Current Status and New Perspectives of Antimicrobial Peptide-Based Therapies. Front Immunol 8: 339.