Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Differential Diagnosis of a Patient with Posterior Lateral Thigh Pain: A Case Report
Keisha M. Paul, Lynne C. Hughes*
Department of Physical Therapy, University of Texas Medical Branch, 301 University Blvd Galveston, TX, USA
Received Date: June 14, 2020; Accepted Date: June 22, 2020; Published Date: July 01, 2020
*Corresponding author: Lynne C. Hughes, Department of Physical Therapy, University of Texas Medical Branch, 301 University Blvd Galveston, TX 77555-1144, USA. Tel: +14097723068; Email: lyhughes@utmb.edu
Citation: Paul KM, Hughes LC (2020) Differential Diagnosis of a Patient with Posterior Lateral Thigh Pain: A Case Report. Adv Ortho and Sprts Med: AOASM-124.
DOI: 10.37722/AOASM.202021
Abstract
Background and Purpose
Gluteus medius tears are often mistakenly diagnosed as trochanteric bursitis due to the common presentations of posterior-lateral thigh pain, poor hip strength, decreased/painful range of motion, and gait deficits. The purpose of this case report was to present a differential diagnosis distinguishing trochanteric bursitis and a gluteus medius tear prior to diagnostic imaging.
Case Description
A 66-year-old female presented with insidious onset of left posterior-lateral thigh pain. Initial exam revealed normal active motion of the lumbar spine, decreased active hip motion, a positive Trendelenburg sign in both static stance and during gait, painful palpation laterally over the greater trochanter and posteriorly in the region of the gluteus medius, and lastly, posterior thigh pain was reproduced with the Slump test.
Outcomes
The exam led to the primary differential diagnoses of trochanteric bursitis and gluteus medius tear. A tear of the gluteus medius may be associated with chemical irritation to the sciatic nerve. The gluteus medius was a likely diagnosis due to significant weakness in hip abductor strength, positive Trendelenburg sign, and painful palpation over both the greater trochanter and gluteus medius. Lumbar radiculopathy was ruled out by a lack of symptoms with both posterior-anterior springing and active extension of the lumbar spine. Imaging confirmed tears of the left gluteus medius at the myotendinous junction.
Discussion and Conclusions
This case highlights the differential diagnosis between trochanteric bursitis and gluteus medius tears. The characteristic findings of gluteus medius tears are painful palpation that extends beyond the trochanter into the gluteus medius muscle, a greater degree of abductor weakness and pain with resistance in tears, and the presence of a positive Trendelenburg sign. It is important to note these differences in presentation and request an MRI to confirm diagnosis.
Keywords: Differential diagnosis, Gluteus medius tears, Greater trochanteric pain syndrome, Lateral hip pain, Physical therapy, Therapeutic exercise, Trochanteric bursitis
Hip pain is a common, self-limiting condition that affects individuals of varying age and activity level. Lateral hip pain has an estimated frequency of 1.8 persons affected per 1,000 annually [1, 2]. Nho, et al. reported the prevalence of gluteus medius tears in women and men with posterior-lateral hip pain to be up to 25% and 10% in men, respectively [3]. Speers and Bhogal further noted that these tears are seen most frequently in women during the 4th-6th decade of life [2-4]. The most common causes of hip pain are osteoarthritis, bursitis, intra-articular derangement, gluteus medius and/or minimus tears, labral tears, and lumbar radiculopathies [3-5]. Complaints of lateral or posterior-lateral thigh pain are often associated with greater trochanteric hip bursitis, lumbar radiculopathies, or gluteus medius tears [3-7].
Diagnoses associated with lateral or posterior-lateral thigh pain may present with decreased and/or painful active range of motion (AROM) at the hip joint, tenderness to palpation, palpable edema near the greater trochanter, and painful decreased strength with resistive testing [6, 8]. Clinical manifestations of lateral or posterior-lateral thigh pain may include gait deviations, discomfort when lying on the affected hip, and difficulty with prolonged sitting or standing [4].
Due to the similarities in subjective and objective findings of multiple hip diagnoses, a thorough examination is imperative to differentially diagnose posterior-lateral hip pain. In addition to examination, several studies have chronicled the appropriateness of Magnetic Resonance Imaging (MRI) for detecting tears of the gluteus medius [7, 8]. MRI is considered the leading form of diagnostic imaging for the successful diagnosis of muscle tears. Nho, et al. [3] reported a 95% specificity and 73% sensitivity for T2-weighted MRIs to aid in the diagnosis of gluteus medius tears.
Gluteus medius tears may be the result of trauma or of chronic non-traumatic damage to the muscle. Many gluteus medius tears are discovered during surgical management of a separate issue with the hip, due to its indistinct symptomology [9]. Clinically, these tears are often confused with trochanteric bursitis due to their common presentations of posterior-lateral thigh pain, poor hip strength, decreased painful range of motion, and gait deficits [5, 6, 8, 9].
Treatment for gluteus medius tears is typically conservative management with physical therapy [7]. However, severe tears found on MRI may be referred for surgical intervention. Undiagnosed tears may be incorrectly classified as greater trochanteric hip bursitis, resulting in prolonged treatment with minimal to no resolution that can decrease the well-being of the patient [4, 5].
This purpose of this patient case report is to describe a clinical scenario of evaluation of a patient with lateral hip pain with emphasis on the differential diagnosis of lumbar radiculopathy, trochanteric bursitis, or a gluteus medius tear. This differential was confirmed with diagnostic imaging. Further, this case presents the physical therapy treatment conducted over 9 weeks.
The Patient
The patient was a 66-year-old female who presented to physical therapy with a 10-year history of chronic, episodic, non-specific low back pain. Past medical history included previous diagnoses of left hip osteoarthritis and left trochanteric bursitis of the hip. Her comorbid conditions included hypercholesterolemia, hypertension, and hypothyroidism, all controlled by oral medications. She also described a several year history of left posterior-lateral thigh pain of insidious onset. The physical therapy referral included a diagnosis of left hip pain – and she had been told her condition was likely bursitis in her left hip. She reported a worsening of symptoms after a professional massage with an onset of new pain symptoms that radiated down the posterior thigh to the knee.
Pain management the previous few years included multiple steroid injections to the trochanteric bursa in addition to oral analgesics (acetaminophen with hydrocodone) as needed. The steroid injections only provided temporary relief.
She had successfully managed her pain with oral analgesics and the steroid injections, but reported these approaches were not working very well anymore. For this reason, her physician referred to physical therapy for the first time. Her goals for therapy were: 1) to be able to climb stairs, 2) to get on and off the floor without pain, and 3) to have increased tolerance for prolonged standing and walking.
Clinical Impression #1
This patient is a good candidate for a case report because her age is consistent with an increased incidence of gluteus medius tears in women in their 4th-6th decade of life and the insidious nature of her symptoms means this condition is often misdiagnosed as trochanteric bursitis [1, 2, 5, 10]. Her primary complaint on initial evaluation was of left posterior-lateral hip pain with radiating symptoms to the posterior-lateral thigh. Functional limitations included difficulty with stair negotiation, rising from low surfaces without upper extremity assistance, prolonged standing, and walking for long distances. A differential diagnosis was performed at initial evaluation when the symptoms did not align with the typical presentation of trochanteric bursitis. The working differential diagnoses included left hip trochanteric bursitis, gluteus medius tear, and lumbar radiculopathy with pain to the posterior-lateral thigh. Prior to physical therapy, the patient’s physician ordered an MRI that had not been conducted at the time of evaluation.
The examination procedures included: range of motion testing (ROM), including active ROM of the lumbosacral spine and active and passive ROM of the hip; joint mobility testing of lumbosacral passive intervertebral motion (PIVM), lumbosacral passive accessory intervertebral motion (PAIVM), and posterior-anterior (PA) vertebral springing with no elicitation of symptoms; neurodynamic testing using the Slump test; palpation of the greater trochanter and gluteus medius; resisted muscle testing of proximal and lateral hip muscles; and evaluation of function through observational gait analysis, Trendelenburg sign test, and functional activities analysis. The functional outcome measure of the Lower Extremity Functional Scale (LEFS) was administered as a self-report tool to assess the patient’s interpretation of her limitations secondary to her left hip pain.
Examination
Range of Motion Testing
The patient demonstrated AROM of the lumbar spine from a standing position. All motions (flexion, extension, lateral flexion, and rotation) were within normal limits and pain-free. Lumbar spine AROM was observed, to aid in ruling out lumbar involvement with the patient’s primary complaint of radiating pain to the left posterior-lateral thigh with concomitant chronic, non-specific low back pain. The patient’s right hip AROM was within normal limits and pain-free, although left hip AROM was limited and painful into extension and abduction. The patient also presented with limited and painful left hip into passive extension (see Table 1). AROM=active range of motion; PROM=passive range of motion; MMT=manual muscle test LEFS=Lower Extremity Functional Scale
Outcome Measure
At evaluation
At 4 weeks
At 8 weeks
Left Hip AROM
Abduction
25°
30°
30°
Extension
5°-0°
0°
7°
Left Hip PROM
Extension
0°
6°
10°
Left Slump test*
positive
negative
negative
Left Hip MMT
Abduction
2/5
3/5
3+/5
Extension
3+/5
3+/5
3+/5
Trendelenburg Sign
positive
positive
positive
LEFS Score
30/80
42/80
55/80
*positive or negative: based on reproduction of posterior thigh pain
Joint Mobility Testing
The patient had no restrictions or provocation of pain in lumbar spine during PIVM testing, PAIVM testing, or PA vertebral springing, nor was there provocation of symptoms with sacral springing. Passive and accessory intervertebral joint mobility with springing to the lumbosacral spine were assessed to aid in ruling out dysfunction of the lumbar spine or sacrum as the cause of her radiating posterior-lateral thigh pain.
Neurodynamic Test – Slump Testing
Slump testing was performed on the patient’s right and left lower extremity for comparison. Slump test on the right lower extremity was negative, whereas testing of the left lower extremity reproduced the patient’s posterior thigh pain following the addition of the distal component (ankle dorsiflexion) of the test (Table 1). Pain was not relieved when the cervical spine was extended, indicating a positive neurodynamic test. The Slump test is a special test that is one of the most commonly used to detect neural irritability in the lower extremities because it includes the addition of spinal flexion, which may increase overall neural tension [10, 11]. This particular test has demonstrated high sensitivity (91%) and moderately high specificity (70%) for identifying neuropathic pain associated with the lower extremity [11]. Neurodynamic testing was selected secondary to the patient’s complaint of pain radiating to the left posterior-lateral thigh.
Palpation
Palpation over both the left greater trochanter and the gluteus medius was significantly painful and tender as reported by the patient; however, the patient noted gluteus medius palpation was more painful in comparison. According to Speers and Bhogal, pain with direct palpation of the greater trochanter coupled with pain elicited within the first 30 seconds of single leg stance havea positive predictive value of 83% for diagnosis of greater trochanteric pain syndrome [4].This diagnosis is sometimes used by physicians to describe pain that is located at the greater trochanter and increases with weight-bearing or direct pressure and may worsen overtime. Trochanteric bursitis and gluteus medius tears are among findings that have been labeled greater trochanteric pain syndrome [3].
Resisted Muscle Testing
Manual muscle testing (MMT) was used to determine strength of the proximal and lateral hip musculature bilaterally (Table 1). MMT is reported as a common place technique of measuring the strength of a muscle [12, 13]. This procedure is used across health professions and requires proper positioning and resistance to determine the appropriate designation of strength. Strength is generally graded on a scale of 0 to 5 with 0 being no active contraction and 5 being strong against maximal resistance [12]. According to Fan et al. [13], MMT has been shown to demonstrate high inter-rater reliability [kappa agreement (95% CI) = 1.00 (0.55-1.00)] for lower extremity rating of muscle strength between pairs of clinicians trained in this technique. Hip extensors were tested with the patient in the prone position with the knee bent to bias toward the gluteus maximus. Hip abductors were tested first in side lying with the lower extremity extended posteriorly and externally rotated to bias the gluteus medius, then in the supine position when the patient was unable to hold the initial test position. Abnormal results were decreased strength in the left hip extensors (3+/5) and abductors (2/5).
Physical Function
Observational gait analysis revealed a hip drop on the right during midstance on the left and decreased left hip extension during terminal stance. Trendelenburg sign, also known as the single leg stance test, is one way to measure muscular hip abductor weakness. A positive Trendelenburg stance is noted when a patient is static standing on a single limb and is unable to maintain a level pelvis [5, 7]. When the hip on the patient’s non-stance limb drops below the stance limb hip, this is indicative of hip abductor weakness. This observation of a positive Trendelenburg sign in static stance, and positive Trendelenburg during gait analysis, combined with results of ROM testing and MMT, suggested decreased strength and motor control of the gluteus medius that also decreases the overall efficiency of gait [5, 7].
Functional activities analysis included stair negotiation and the ability to rise from a chair. The patient demonstrated hip drop on the right side during both concentric and eccentric negotiation of stairs (further demonstration of positive Trendelenburg [see above]). During her rise from a chair, the patient demonstrated bilateral genu valgus, excessive trunk flexion, and the use of upper extremities to rise from a chair [4, 5, 8, 14, 15]. The hip abductors are used to stabilize the hips and knees during closed chain activities (i.e. when the foot is fixed to the floor and the proximal components of the body perform the movement). When the knees dive inward towards each other during a movement (dynamic valgus), it is indicative of weakness in the hip abductors. This presentation, coupled with excessive trunk flexion and use of upper extremities to rise from the chair, suggested compensation for weakness in the hips.
Lower Extremity Functional Scale (LEFS)
The LEFS was completed during the initial evaluation. The LEFS is a self-report tool used to decipher the patient’s perception of his/her functional abilities and limitations based on lower extremity deficits [16]. Activities addressed in the LEFS include, but are not limited to, housework, getting in and out of a car, sitting for 1 hour, walking a mile, running, hopping, and rolling over in bed. Her initial LEFS score was 30/80, indicating a self-report of 62.5% disability (Table 1). Difficulty was noted with each of the following activities: going up and down stairs, rising from low surfaces (i.e., chairs or the floor), and prolonged standing and walking. The minimal clinical important difference is a 9-point increase, which indicates a patient’s perception of improvement with daily tasks [17].
Clinical Impression #2
Initial differential diagnoses considered were trochanteric bursitis, gluteus medius tear, and lumbar radiculopathy. Lumbar radiculopathy was ruled out due to no reproduction of symptoms with PIVMs, PAIVMs, PA springing of the lumbosacral spine, or active trunk extension. Trochanteric bursitis was ruled out due to tenderness to palpation extending beyond the greater trochanter, significant pain reported during resistive hip abductor testing, and left Trendelenburg noted in both static and dynamic positions. A tear of the gluteus medius with associated chemical irritation to the sciatic nerve was a likely diagnosis due to positive Slump testing, painful palpation over the greater trochanter extending to the gluteus medius, significant lack of hip abductor strength, and positive Trendelenburg in stance and during gait.
The initial intervention included focused strengthening of the proximal and lateral hip musculature, functional lower extremity strengthening based on activity limitations, and manual therapy interventions to address deficits of decreased active/passive left hip extension and active abduction. The patient was scheduled to be formally reassessed in 4 weeks to observe the progress in the initial outcome measures.
Approximately two weeks following the evaluation and initiation of the physical therapy plan of care, a diagnosis of a gluteus medius and partial gluteus minimus tear was confirmed by T2-weighted MRI (Figs. 1-4). Specific findings from imaging reveled a high-grade tear of the left gluteus medius at the myotendinous junction (a portion of the posterior distal gluteus medius tendon remained intact) along with a partial tear at the myotendinous junction of the gluteus minimus. The patient was directed back to her physician for a follow-up visit to discuss options of surgical intervention versus continued conservative management with physical therapy, given the magnitude of the tear. Ultimately, she decided to continue physical therapy in the hopes of avoiding a surgical intervention. The initial plan of care was for 4 weeks of therapy; however, the duration of therapy was lengthened after the results of the MRI were received. Increasing therapy to at least 8 weeks allowed for strength gains and the patient’s functional goals to be reasonably achieved.
T-2 weighted MRI: coronal view
Actual image used with permission
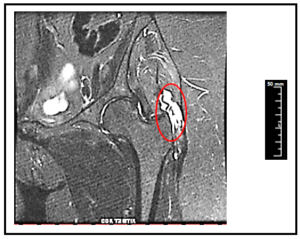
Figure 1: Left gluteus medius tear and inflammation.
T-2 weighted MRI: Coronal view
Actual image used with permission
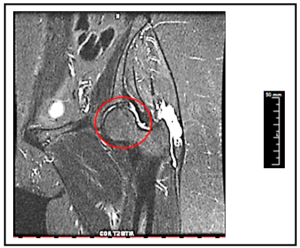
Figure 2: Inflammation in the left hip joint.
T-2 weighted MRI: Axial view
Actual image- used with permission
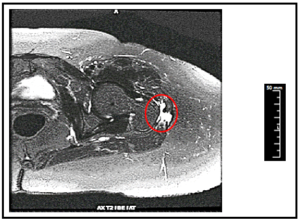
Figure 3: Left gluteus medius tear and inflammation.
T-2 weighted MRI: Axial view
Actual image- used with permission
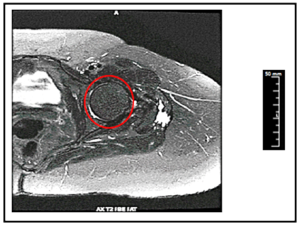
Figure 4: Inflammation in the left hip joint.
Intervention
The patient participated in physical therapy at an outpatient clinic twice weekly for 9 weeks. Each session lasted approximately 60-minutes and included interventions that addressed deficits revealed during the initial evaluation. Activities which focused on therapeutic exercise and neuromuscular reeducation were initiated to improve strength and motor control of the hip and trunk muscles. Functional activities such as squats to an elevated box, single limb stance, and stair negotiation were done to facilitate practical use of the lower extremities during daily tasks. Manual therapy was performed to address deficits of decreased left hip ROM.
Upon arrival to each session, symptoms were reassessed. Warm-up was performed on a recumbent bike, followed by manual techniques as needed to address any mobility deficits of the lower extremities. Manual techniques included: long axis distraction and lateral femoral glide of the left lower extremity to improve overall hip mobility; and left anterior femoral glide to improve hip extension. Other interventions included motor control and neuromuscular reeducation using endurance-based isometric exercises (5-10 second isometric contraction holds) with concentration on hip abductors, external rotators, and extensors. Functional limitations were addressed with activities including squats (with and without upper extremity support), single leg activities (both static and dynamic), stair negotiation, and gait training. See (Table 2) for details of the exercise program.
As the patient improved, interventions were progressed to further challenge muscular endurance, strength, and functional activities. Progressions included manual resistance or resistance bands targeting the gluteus medius to challenge strength and narrowing the base of support to challenge balance. All exercises and activities were monitored by a physical therapist or physical therapist assistant. Manual Therapy Neuromuscular Reeducation Functional Activities
Intervention Type
Intervention
Progression
Therapeutic Exercise
Recumbent bike x 10-15 minutes
Long axis distraction of L hip, grade III-IV (supine)
Lateral glide of L femur, grade III-IV (hook-lying)
Anterior glide of L femur, grade III-IV (prone)
Isometric hip abduction (hook-lying)
Standing isometric hip abduction at wall
Isometric glute and hamstring setting (hook-lying)
Prolonged holds (10-15 seconds) of bilateral LE bridging
Hip abduction/external rotation with 5-10 second holds (hooked side-lying clams)
Addition of resistance bands (level Iàlevel II)
Bilateral LE bridging with 5-10 second holds
Addition of resistance bands (level Iàlevel II)
Side planks modified to knees with 10-20 second hold
Addition of side-lying clamsà addition of resistance band
Squat to 36in. box with resistance band around distal thigh to combat genu valgus
Decreased to 24in. boxà further progressed for endurance with Tabata timer 1 min on/ 20 sec off x 5
Single leg stance on flat hard surface
Surface change to balance foam pad
Step up forward up/down with eccentric control on 4in. step
Increased to 6in. step (with and without upper extremity support)
Breakdown of gait mechanics with focus on heel strike through terminal stance
Slow, controlled ambulation throughout clinic
Outcomes
Outcome measures were range of motion, joint mobility, Slump testing, palpation, resisted muscle testing of the proximal hip, observational gait, Trendelenburg Sign, functional activities analysis, and LEFS. Each test was performed at initial evaluation and re-administered at 4 weeks and 8 weeks prior to discharge at week 9. The examination list and results are provided in (Table 1).
Throughout the episode of care, the patient demonstrated improvement in all measures. Passive and active ROM increased into left hip extension, as well as active motion into hip abduction. She received some resolution of the chemical irritation of the left sciatic nerve as evidenced by a negative Slump test. Better grades of MMT demonstrated improved strength of the left hip abductors and extensors. Improvement in motor control of the left hip abductor during sit to stand was evidenced by decreased active valgus during this activity. Greater left hip extension motion, coupled with improvement in hip abductor strength, resulted in increased left hip extension during mid to terminal stance and decreased magnitude of Trendelenburg sign, thereby enhancing the overall efficiency of her gait. The patient also had improved self-report of disability secondary to lower extremity dysfunction on LEFS (Table 1). LEFS score improved from an initial score of 30/80 to 55/80. A clinically significant difference is a 9-point improvement in this outcome measure.
Discussion
This case report described a differential diagnosis of a gluteus medius tear that was confirmed on diagnostic imaging. The patient in this case report was initially sent to physical therapy for an evaluation following a diagnosis of trochanteric bursitis. Without careful consideration of the subtle differences that distinguish gluteus medius tears from trochanteric bursitis, the patient may have been managed without consideration for the tear. Diagnostic imaging revealed a high-grade tear of the left gluteus medius at the myotendinous junction with only the distal posterior portion intact.
Gluteus medius tears are commonly misdiagnosed as greater trochanteric hip bursitis, yet examination results reveal subtle differences. Patients with gluteus medius tears will: 1) present with tenderness to palpation that will extend past the greater trochanter into the gluteus medius; 2) will have more significant pain during resisted testing; 3) will present with a positive Trendelenburg sign indicating a significant weakness of the gluteus medius [2, 5, 8]. These differences in are important to note when differentiating sources of posterior-lateral hip pain during the evaluation and examination due to similar presentations in potential diagnoses. For example, trochanteric bursitis also presents with pain upon palpation to the greater trochanter, but the pain does not extend into the gluteus muscle. Pain and weakness will also be exhibited with resisted testing, but less than what is present with a gluteus medius tear [5]. A T2-weighted MRI may be utilized to confirm diagnosis of a gluteus medius tear [15, 18, 19].
The indications for use of an MRI as a diagnostic tool include, but are not limited to, the diagnosis, exclusion, and grading of, “musculotendinous disorders and associated bursitis” [18]. McKinnis also includes the use of an MRI to evaluate the presence of unexplained hip or trochanteric pain. Given that this patient had left posterior-lateral thigh pain that persisted despite pharmacological intervention, an MRI was appropriate [18]. Increased signal intensity at the gluteus medius tendon in T2-weighted MRI is indicative of a tear [9, 19]. According to the American College of Radiology Appropriateness Criteria (ACR guidelines), individuals with chronic hip pain suspected of having an extra-articular, non-infectious, soft tissue abnormality should have an MRI without IV contrast performed, even following a negative or non-diagnostic radiograph [19]. In this case, the physician never ordered an x-ray, but instead went directly to an MRI when pharmacological intervention did not improve the patient’s symptoms.
Treatment interventions should include therapeutic exercise and neuromuscular re-education with a focus on strengthening the glutes and extensors, as well as the hip abductors and rotators in an effort to support the hip joint when the torn gluteus medius may not be capable. These exercises should include both open kinetic chain and closed kinetic chain exercises that incorporate functional activities. This is well substantiated in the evidence as seen in other studies such as Gowda, et al in 2014 [14].
In conclusion, tears of the gluteus medius are often misdiagnosed as trochanteric bursitis. Common findings between the diagnoses are posterior lateral thigh pain, poor hip strength, decreased and painful active range of motion. Differences are in the location of the pain, level of the pain (particularly with resistance testing), and degree of weakness of the hip abductors. It is important to perform a careful examination to determine these differences in clinical presentation that will lead to an accurate diagnosis and appropriate plan of care for our patients [18, 19].
References
- Thaunat M, Chatellard R, Noel E, Sonnery-Cottet B, Nove-Josserand L (2013) Endoscopic repair of partial-thickness undersurface tears of the gluteus medius tendon. OrthopTraumatol Surg Res 99: 853-857.
- Coulomb R, Essig J, Mares O, Asencio G, Kouyoumdjian P, et al. (2016) Clinical results of endoscopic treatment without repair for partial thickness gluteal tears. OrthopTraumatol Surg Res 102: 391-395.
- Nho SJ, Grzybowski JS, Bogunovic L, Kuhns BD, Matheret RC, et al. (2016) Diagnosis, Evaluation, and Endoscopic Repair of Partial Articular Gluteus Tendon Avulsion. Arthrosc Tech 5: e425-431.
- Speers CJ, Bhogal GS (2017) Greater trochanteric pain syndrome: a review of diagnosis and management in general practice. Br J Gen Pract 67: 479-480.
- Wilson JJ, Furukawa M (2014) Evaluation of the patient with hip pain. Am Fam Physician 89: 27-34.
- Lustenberger DP, Ng VY, Best TM, Ellis TJ (2011) Efficacy of treatment of trochanteric bursitis: a systematic review. Clin J Sport Med 21: 447-453.
- Chandrasekaran S, Vemula SP, Gui C, Suarez-Ahedo C, Lodhia P, Domb BG (2015) Clinical Features That Predict the Need for Operative Intervention in Gluteus Medius Tears. Orthop J Sports Med 3:
- Lindner D, Shohat N, Botser I, Agar G, Domb BG (2015) Clinical presentation and imaging results of patients with symptomatic gluteus medius tears. J Hip Preserv Surg 2: 310-315.
- Lachiewicz PF (2011) Abductor tendon tears of the hip: evaluation and management. J Am AcadOrthop Surg 19: 385-391.
- Ferreira G, Stieven F, Araujo F, Wiebusch W, Rosa C, et al. (2016) Neurodynamic treatment did not improve pain and disability at two weeks in patients with chronic nerve-related leg pain: a randomised trial. J Physiother 62: 197-202.
- Urban LM, MacNeil BJ (2015) Diagnostic Accuracy of the Slump Test for Identifying Neuropathic Pain in the Lower Limb. J Orthop Sports Phys Ther 45: 596-603.
- Cuthbert SC, Goodheart GJ (2007) on the reliability and validity of manual muscle testing: a literature review. ChiroprOsteopat. 15:4.
- Fan E, Ciesla ND, Truong AD, Bhoopathi V, Zeger SL, et al. (2010) Inter-rater reliability of manual muscle strength testing in ICU survivors and simulated patients. Intensive Care Med 36: 1038-1043.
- Gowda AL, Mease SJ, Donatelli R, Zelicof S (2014) Gluteus medius strengthening and the use of the Donatelli Drop Leg Test in the athlete. Phys Ther Sport 15: 15-19.
- Cvitanic O, Henzie G, Skezas N, Lyons J, Minter J (2004) MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus). AJR Am J Roentgenol 182: 137-143.
- Mehta SP, Fulton A, Quach C, Thistle M, Toledo C, et al. (2016) Measurement Properties of the Lower Extremity Functional Scale: A Systematic Review. J Orthop Sports Phys Ther 46: 200-216.
- Binkley JM, Stratford PW, Lott SA, Riddle DL (1999) The Lower Extremity Functional Scale (LEFS): Scale Development, Measurement Properties, and Clinical Application, J Phys Ther. 79:371–83
- McKinnis LN. (2014) Fundamentals of Musculoskeletal Imaging. 4th ed. Philadelphia: F.A. Davis Company.
- Radiology ACo. ACR appropriateness criteria: Chronic Hip Pain. Available at: https://acsearch.acr.org/docs/69425/Narrative/ Published 2016. Accessed February 24, 2018.