Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Custom Glenoid Implant in Total Shoulder Arthroplasty: Case Report of Two Patients
Jerome C. Murray, MD1*; Jonathan Braman, MD1; Alicia Harrison, MD1; Allison Rao, MD1
1Department of Orthopedic Surgery, University of Minnesota Medical School, Minneapolis, MN, USA
Received Date: May 24, 2024; Accepted Date: June 08, 2024; Published Date: June 16, 2024;
*Corresponding author: Jerome C. Murray, Department of Orthopedic Surgery, University of Minnesota Medical School, Minneapolis, MN- 55454, USA. Email: murr0526@umn.edu
Citation: Murray JC, Braman J, Harrison A, Rao A. Custom Glenoid Implant in Total Shoulder Arthroplasty: Case Report of 2 Patients. Adv Ortho and Sprts Med: AOASM-199
DOI: 10.37722/AOASM.2024202
Abstract
Introduction: Glenohumeral arthritis is typically treated with shoulder arthroplasty, however in younger patients with complex glenoid pathology this can become more challenging. Considerations surrounding surgical management strive to provide a functional, stable shoulder, while maintaining options for revision in the future. Custom glenoid implants have emerged as a promising option for patients in this challenging population, however there is a lack of literature surrounding their use for addressing glenoid bone loss for anatomic total shoulder arthroplasty. This case report highlights the course of treatment for 2 patients with severe glenoid bone deficiency and debilitating shoulder pain. A custom glenoid implant was used after careful consideration and review of available options. The use of a convertible custom glenoid implant for these patients allowed for improved function and decreased pain, while preserving options for treatment in the future.
Conclusion: Custom glenoid implants can be a useful tool for addressing significant and complex glenoid bone loss in younger patients.
Keywords: Arthroplasty, Custom implant, Glenoid, Shoulder, Total shoulder, Shoulder; Arthroplasty; Total shoulder arthroplasty; glenoid; custom implant
Introduction
Surgical treatment of glenohumeral arthritis in non-geriatric adult patients can be very challenging [1]. Patients often have underlying inflammatory conditions or rapidly progressive disease, leading to subsequent bone loss and deformity [2, 3]. If joint preserving options are not feasible, an ideal reconstructive procedure would balance the high functional demands of this patient population while preserving options for any future potential revision [4]. Anatomic total shoulder arthroplasty (TSA) for glenohumeral arthritis provides improved function, longevity, and options for later conversion to reverse shoulder arthroplasty (RTSA). However, management of significant glenoid bone loss or deformity can be challenging when considering a TSA as a treatment option [3]. Other treatment options include the use of prefabricated augmented components, bone grafting in either a primary or staged fashion, inlay components, or use of a primary reverse shoulder arthroplasty [4–7]. Although custom glenoid baseplates have become more common in RTSA, custom glenoid implants in anatomic total shoulder arthroplasty have lagged behind. This case report will discuss two patients with complex glenoid bone loss where a custom convertible glenoid component was used for anatomic total shoulder arthroplasty.
Case 1
Patient is a 50-year-old male with right shoulder pain. A year prior to his initial visit, he underwent right shoulder arthroscopic capsular resection, decompression with bony acromioplasty, and open biceps tenodesis. The pain persisted and prevented him from playing golf, caused him to avoid overhead activities, and began to interfere with his sleep. Initial examination of the patient’s right shoulder displayed tenderness around the bicipital groove, 85 degrees of active and passive forward elevation, 50 degrees of external rotation, and internal rotation to his lower back and glutes. Radiographs showed end stage glenohumeral osteoarthritis with severe posterior glenoid bone loss. Computed Tomography (CT) scan displayed complete loss of glenohumeral joint space, large subchondral cyst in the glenoid vault, 12 degree retroversion of the glenoid as well as remodeling of the humeral head (Figure 1). To adequately address the significant subchondral bone cyst in the vault with posterior glenoid bone loss, a custom implant was utilized.
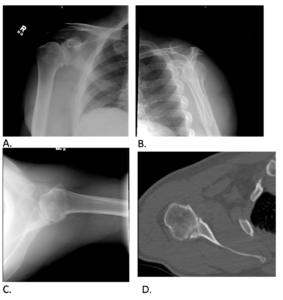
Figure 1: Grashey (A), Scapular Y (B), Axillary (C) view radiographs, Axillary CT (D) of the right shoulder.
Operative Plan
A custom implant was designed with use of Zimmer-Biomet (Zimmer-Biomet, Warsaw, IN, USA) Complete Shoulder Solution as it would address the lack of bone stock in the posterior glenoid. Time from ordering the implant to surgery was less than six months.
Surgery was performed in the beach chair position with preoperative interscalene blockade and general endotracheal anesthesia. A standard deltopectoral approach was used, with the addition of a lesser tuberosity osteotomy. The humeral head was cut in 30 degrees of retroversion and a press fit stem was sized to 15mm x 55mm. Glenoid exposure proceeded without difficulty after a circumferential labral and inferior capsular release. The custom guide was used to identify the center position of the glenoid. The provisional implant fit in this boss reamer, and, consequently, the definitive implant was opened and impacted over the guide pin. A center screw was placed followed by peripheral locking screws. A trial reduction with the implant trial demonstrated posterior translation of 30%, 60 degrees of external rotation at the side, 70 degrees of internal rotation and 90 degrees of abduction. A 52x18mm eccentric humeral head was selected and impacted, and intraoperative range of motion was found to be unchanged from the trial. Surgical time was 2 hours and 22 minutes, and estimated blood loss was 500 milliliters. Postoperatively the patient was placed in a sling for six weeks.
At 1 year follow up, physical examination displayed 160 degrees of forward elevation, 160 degrees of abduction, and 60 degrees of external rotation at the side. At 18 months postoperatively he began to experience shoulder pain radiating to the elbow, which limited his progression in physical therapy. During this visit his motion was noted to be 145 degrees of forward elevation and 50 degrees of external rotation. On exam, pain was elicited with any movement of the joint. Synovial biopsies were obtained arthroscopically a month later, two years from the sentinel shoulder arthroplasty. His cultures grew Cutibacterium acnes, and he subsequently required two stage revision with antibiotic spacer and later reimplantation. Once the infection was cleared, a pectoralis major transfer was done to address a deficient subscapularis tendon seen during arthroscopic biopsy. Physical exam at the 3 month follow-up visit from this procedure showed 165 degrees of forward elevation and apprehension with abduction. The patient also had 35 degrees of external rotation at the side and internal rotation to the back pocket. At the 1 year follow-up from his revision, the patient was able to return to more aggressive activities including golf and painting his house. At the 4 year post-operative visit, the patient was very satisfied with his shoulder surgery. Physical examination displayed 180 degrees of forward elevation, 180 degrees of abduction, 70 degrees of external rotation at the side and internal rotation to T10. Radiographs at this time showed appropriately fixed hardware with some anterior superior humeral subluxation (Figure 2). At six year follow up he reported a sense of squeaking in the shoulder but denied grinding. He was still able to play golf at 7 year follow up, and reported no issues. Physical examination displayed 170 degrees of active forward elevation, 150 degrees of abduction, painful external rotation to 20 degrees, as well as internal rotation to the hip. His subscapularis remained weak, but he had full strength of the supraspinatus and infraspinatus.
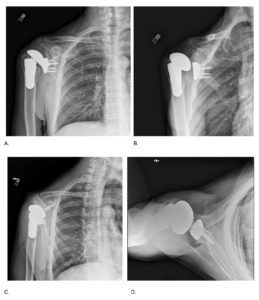
Figure 2: AP (A), Grashey (B), Scapular Y (C), and Axillary (D) view radiographs of the right shoulder 4-years post total shoulder arthroplasty.
Case 2
Patient is a 55-year-old right hand dominant male with over 30 years of bilateral shoulder pain, which was more severe in the left than right upon initial presentation. He had previously undergone an arthroscopic glenohumeral debridement of the right shoulder four years prior by a different surgeon that offered substantial pain relief. At the time of this visit, the patient was working in construction, but lifting had recently become impossible. Left shoulder replacement with standard implants was performed, and t tolerated this well, reporting satisfaction with the result. Following full recovery, the right shoulder became more symptomatic. Physical examination of the right shoulder at this time showed active forward flexion to 70 degrees, passive forward flexion to 105 degrees, external rotation to 40 degrees, and internal rotation to the back of the gluteus. Radiographs of the right shoulder showed significant end-stage degenerative glenohumeral arthritis with posterior subluxation of the humeral head and significant posterior glenoid wear and biconcavity. CT scan revealed severe degenerative changes of the glenohumeral joint with subchondral cyst formation, 40 degrees of retroversion, loss of glenoid bone stock, and posterior subluxation of the head, consistent with a Walch B2 glenoid (Figure 3). Due to the significant retroversion and posterior glenoid bone loss, a custom implant was designed to adequately address the posterior bone loss.
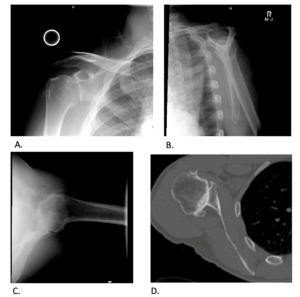
Figure 3: Grashey (A), Scapular Y (B), Axillary (C) view radiographs for the right shoulder. Axillary CT of the right shoulder (D).
Operative Plan
A custom implant was again designed with use of Zimmer-Biomet (Zimmer-Biomet, Warsaw, IN, USA) Biomet Comprehensive Convertible Glenoid as it would provide a large posterior augment, address the shallow bone stock, and provide a convertible option for revision in this patient (Figure 4). Time from ordering the implant to surgical implantation was less than six months.
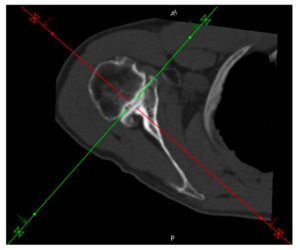
Figure 4: CT of the right shoulder used for preoperative planning.
Surgery was performed in similar fashion to the other cases in this report. Surgical time was 3 hours and estimated blood loss was 250 milliliters. Postoperatively, the patient was placed in an abduction sling for six weeks, allowed to perform palm forward Codman exercises immediately but no range of motion for two weeks. The patient was then progressed to pulley exercises. At 6 weeks postoperatively, range of motion was noted to be active forward flexion of 110 degrees, external rotation of 30 degrees, and internal rotation to 0 degrees. At one year follow up, the patient reported significant improvement in his right shoulder but less range of motion in comparison to the left shoulder. Physical examination revealed 90 degrees of active forward elevation and 120 degrees of passive forward elevation in the right shoulder. External rotation was 60 degrees and symmetric to the left with internal rotation to T9. He had full strength with belly press and internal rotation at the side, but weakness in resisted forward elevation. The left shoulder had full strength throughout. Radiographs obtained at this time showed well fixed implants with superior migration of the humerus (Figure 5). At 2 year follow up the patient experienced some grinding with movement, but expressed overall satisfaction with the result of his right shoulder surgery. Physical exam revealed 85 degrees of active forward elevation, 35 degrees of external rotation, and internal rotation to L1. At 3 year follow up, even with continued non-painful grinding with passive motion, he was happy with his shoulder. Physical examination revealed 80 degrees of active forward elevation, 30 degrees of active external rotation, and internal rotation to L1. Right shoulder x-rays obtained at this visit showed superior migration of the humerus compared to the glenoid, increased from prior year (Figure 6). At 5 year follow up, the patient was very satisfied with his shoulder, despite experiencing some limitations with range of motion. At this time, he could reach his mouth and groin with his right arm. He could achieve 30 degrees of active forward elevation, 15 degrees of external rotation at the side, and internal rotation to L1. Although he had no complaints, the conversation was shifted to the likelihood of a conversion to a reverse total shoulder arthroplasty. The risk of metallosis and subsequent component loosening was explained as these would complicate his chance of successful conversion. The patient ultimately declined to pursue the conversion because they are currently in no pain and are quite satisfied with their current shoulder function.
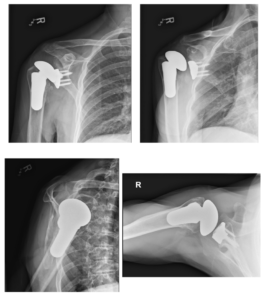
Figure 5: AP, Grashey, Scapular Y, and Axillary view radiographs of the right shoulder 1-year post total shoulder arthroplasty.
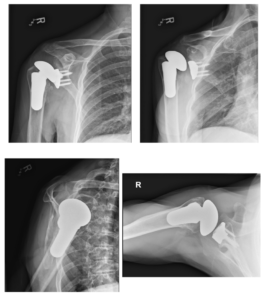
Figure 6: AP, Grashey, Scapular Y, and Axillary view radiographs of the right shoulder 3-year post total shoulder arthroplasty.
Discussion
Glenohumeral osteoarthritis is a common disease process that is often successfully treated with shoulder arthroplasty [2, 8]. However, management of bone loss, significant retroversion or deformity, and cyst formation can be difficult with standard design TSA [8–11]. As the demand increases in a younger population who often have more complex pathology due to trauma, instability, previous surgery, or inflammatory and systemic conditions, additional treatment options are becoming more necessary [1, 12]. There is a paucity of literature outlining the use of a custom implant for TSA to address challenging glenoid deformity, such as these two cases. This case report aimed to provide detailed examples surrounding the utilization of a custom glenoid implant in TSA to address glenoid retroversion and bone loss for glenohumeral arthritis. Both patients in this case series had complex pathology requiring significant correction of glenoid deformity.
Limited options exist for patients who wish to have a TSA but require correction of retroversion, bone loss, or need to address a shallow vault [3, 4, 11]. TSA remains a favorable option in younger patients due to improved function, patient reported outcomes, and options for later conversion to RTSA [13–16]. Another consideration for the use of TSA in this patient population is a lower revision rate compared to RTSA [14, 17]. Careful consideration must be taken by the surgeon when determining candidacy for use of a custom implant. Most importantly, as illustrated by these two patients, these complex cases are not without complication. Both cases presented in this report had evidence of subluxation on radiographs. While this is a less than desirable outcome following TSA with or without a custom glenoid component, these patients presented without clinical symptoms significantly impacting their function and subjectively rated the outcome of their surgery very highly. Numerous studies have found that younger patients are at higher risk of rotator cuff failure and conversion to reverse shoulder arthroplasty [14, 15, 19, 20]. Additionally, this patient population has been shown to have higher colonization, especially with Cutibacterium acnes and is at increased risk for infection, as infection rates in patients who have had prior surgery are higher 18.
As these cases demonstrate, a clear preoperative conversation with patients is critical. Patients must be aware that with severe deformity and increasing surgical complexity, the goals of surgery are to achieve a functional, stable shoulder while minimizing pain and preserving options for the future. Both the patients written about experienced significant improvement of pain, and one patient was able to return to playing golf. These examples demonstrate that rather than a primary reverse shoulder arthroplasty to manage significant glenoid deformity, a total shoulder arthroplasty with custom implants is a viable option to treat select complex cases and reserve more options for future treatment.
Conclusion
These two cases display that custom glenoid implants can be a useful tool to address severe glenoid bone loss in young patients in whom a total shoulder arthroplasty is a desirable treatment. A custom implant can be a useful tool in the armamentarium of options for shoulder surgeons treating challenging cases of glenoid version and bone loss. Future studies examining long-term outcomes will hopefully continue to demonstrate the success of these implants and preserved options for revision in the future.
References
- Saltzman BM, Leroux TS, Verma NN, Romeo AA. Glenohumeral Osteoarthritis in the Young Patient. Journal of the American Academy of Orthopaedic Surgeons. 2018;26(17):E361-E370. doi:10.5435/JAAOS-D-16-00657
- Ibounig T, Simons T, Launonen A, Paavola M. Glenohumeral osteoarthritis: an overview of etiology and diagnostics. Scandinavian Journal of Surgery. 2021;110(3):441-451. doi:10.1177/1457496920935018
- Porcellini G, Micheloni GM, Tarallo L, Paladini P, Merolla G, Catani F. Custom-made reverse shoulder arthroplasty for severe glenoid bone loss: review of the literature and our preliminary results. Journal of Orthopaedics and Traumatology. 2021;22(1). doi:10.1186/s10195-020-00564-6
- Bodendorfer BM, Loughran GJ, Looney AM, et al. Short-term outcomes of reverse shoulder arthroplasty using a custom baseplate for severe glenoid deficiency. J Shoulder Elbow Surg. 2021;30(5):1060-1067. doi:10.1016/j.jse.2020.08.002
- Paul RA, Maldonado-Rodriguez N, Docter S, et al. Glenoid bone grafting in primary reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2019;28(12):2447-2456. doi:10.1016/j.jse.2019.05.011
- Cvetanovich GL, Naylor AJ, O’Brien MC, Waterman BR, Garcia GH, Nicholson GP. Anatomic total shoulder arthroplasty with an inlay glenoid component: clinical outcomes and return to activity. J Shoulder Elbow Surg. 2020;29(6):1188-1196. doi:10.1016/j.jse.2019.10.003
- Priddy M, Zarezadeh A, Farmer KW, et al. Early results of augmented anatomic glenoid components. J Shoulder Elbow Surg. 2019;28(6):S138-S145. doi:10.1016/j.jse.2019.04.014
- Sears BW, Johnston PS, Ramsey ML, Williams GR. Glenoid bone loss in primary total shoulder arthroplasty: Evaluation and management. Journal of the American Academy of Orthopaedic Surgeons. 2012;20(9):604-613. doi:10.5435/JAAOS-20-09-604
- Stephens SP, Paisley KC, Jeng J, Dutta AK, Wirth MA. Shoulder arthroplasty in the presence of posterior glenoid bone loss. Journal of Bone and Joint Surgery – American Volume. 2015;97(3):251-259. doi:10.2106/JBJS.N.00566
- Hsu JE, Ricchetti ET, Huffman GR, Iannotti JP, Glaser DL. Addressing glenoid bone deficiency and asymmetric posterior erosion in shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(9):1298-1308. doi:10.1016/J.JSE.2013.04.014
- Ghoraishian M, Abboud JA, Romeo AA, Williams GR, Namdari S. Augmented glenoid implants in anatomic total shoulder arthroplasty: review of available implants and current literature. J Shoulder Elbow Surg. 2019;28(2):387-395. doi:10.1016/j.jse.2018.08.017
- Padegimas EM, Maltenfort M, Lazarus MD, Ramsey ML, Williams GR, Namdari S. Future Patient Demand for Shoulder Arthroplasty by Younger Patients: National Projections. Clin Orthop Relat Res. 2015;473(6):1860-1867. doi:10.1007/s11999-015-4231-z
- Drager J, Polce EM, Fu M, et al. Patients undergoing anatomic total shoulder arthroplasty achieve clinically significant outcomes faster than those undergoing reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30(11):2523-2532. doi:10.1016/j.jse.2021.02.015
- Dillon MT, Inacio MCS, Burke MF, Navarro RA, Yian EH. Shoulder arthroplasty in patients 59 years of age and younger. J Shoulder Elbow Surg. 2013;22(10):1338-1344. doi:10.1016/J.JSE.2013.01.029
- Bartelt R, Sperling JW, Schleck CD, Cofield RH. Shoulder arthroplasty in patients aged fifty-five years or younger with osteoarthritis. J Shoulder Elbow Surg. 2011;20(1):123-130. doi:10.1016/J.JSE.2010.05.006
- Singh Jagdev B, McGrath J, Cole A, Gomaa AR, Chong HH, Singh HP. Total shoulder arthroplasty vs. hemiarthroplasty in patients with primary glenohumeral arthritis with intact rotator cuff: meta-analysis using the ratio of means. J Shoulder Elbow Surg. 2022;31(12):2657-2670. doi:10.1016/J.JSE.2022.07.012
- Chammaa R, Uri O, Lambert S. Primary shoulder arthroplasty using a custom-made hip-inspired implant for the treatment of advanced glenohumeral arthritis in the presence of severe glenoid bone loss. J Shoulder Elbow Surg. 2017;26(1):101-107. doi:10.1016/j.jse.2016.05.027
- Wickman JR, Goltz DE, Levin JM, Lassiter T, Anakwenze OA, Klifto CS. Early aseptic reoperation after shoulder arthroplasty increases risk of subsequent prosthetic joint infection. JSES Int. 2021;5(6):1067-1071. doi:10.1016/j.jseint.2021.06.002
- Seok HG, Park JJ, Park SG. Risk Factors for Periprosthetic Joint Infection after Shoulder Arthroplasty: Systematic Review and Meta-Analysis. J Clin Med. 2022;11(14). doi:10.3390/jcm11144245
- Wagner ER, Houdek MT, Schleck CD, et al. The role age plays in the outcomes and complications of shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(9):1573-1580. doi:10.1016/J.JSE.2017.01.020