Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Acute Infrapatellar Fat Pad Injury in a Professional Football Player: A Case Report and Mechanism Analysis
Kassem El Houcheimi*, Nabih Berjaoui
1Nabih Berjaoui MBBS, BScs, Lebanon
Received Date: February 11, 2025; Accepted Date: February 21, 2025Published Date: February 28, 2025;
*Corresponding author: Kassem El Houcheimi, FACS, MBA, Orthopedic surgeon, Department of Orthopedics, Clemenceau Medical Center Dubai.
Citation: Houcheimi K E, Berjaoui N; Acute Infrapatellar Fat Pad Injury in a Professional Football Player: A Case Report and Mechanism Analysis. Adv Ortho and Sprts Med: AOASM-201
DOI: 10.37722/AOASM.2025101
Introduction
The infrapatellar fat pad (also known as Hoffa’s fat pad) is an intracapsular but extrasynovial structure located beneath the patella and patellar tendon. This fat pad plays a crucial role in knee biomechanics, acting as a cushion and facilitating smooth joint movement. While chronic damage to the infrapatellar fat pad due to repetitive impingement is well-documented, acute traumatic injuries, particularly in athletes, are exceedingly rare. Such injuries can result in inflammation, edema, and hemorrhage, leading to functional impairment. This case report highlights a unique instance of acute infrapatellar fat pad injury in a professional football player, emphasizing the diagnostic challenges, management strategies, and recovery outcomes.
Case Presentation
A 28-year-old male professional football player, with a height of 184 cm, weight of 76 kg, and body mass index (BMI) of 22.4 kg/m², presented with right knee pain following a non-contact hyperflexion injury during a league match. The injury occurred during the fourth minute of the second half when the player slipped while dribbling, causing his right knee to hyperflex beyond 140° with associated external rotation of the tibia. Video analysis confirmed the absence of direct collision and revealed the precise mechanism of injury. Despite initial on-field assessment by the medical team, the player was unable to continue the match and was substituted.
Upon visiting the emergency room, the patient reported moderate pain and inability to bear weight. Clinical examination revealed anterior knee tenderness, moderate swelling, and restricted range of motion (0° extension to 100° flexion). Ligament stability tests were negative, and there were no signs of joint effusion or significant bruising. Due to patient refusal, a plain X-ray was not performed. Magnetic resonance imaging (MRI) was subsequently conducted for further evaluation.
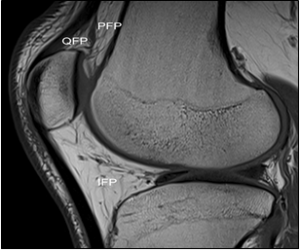
Fig. 1. T1-weighted sagittal magnetic resonance image of the knee shows the intracapsular but extrasynovial fat pads –infrapatellar fat pad (IPF), quadriceps fat pad (QFP), pre- femoral fat pad (PFP).
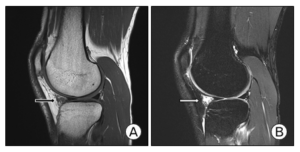
Fig 2: On magnetic resonance image (MRI) scan, low sig- nal intensity in the T1-weighted sagittal image (A) and high signal intensity in the T2-weighted sagittal image (B) were observed at the infrapatellar fat pad located in the anterior part of the anterior horn of the lateral meniscus (arrow). MRIs show fluid collection anteriorly from the proximal tibia extending to the anterior horns of the meniscus.
Mechanism of Injury
The injury mechanism involved a sudden hyperflexion of the knee coupled with external tibial rotation. This motion likely caused acute displacement and compression of the infrapatellar fat pad, resulting in tissue damage. Previous studies have highlighted the susceptibility of the infrapatellar fat pad to trauma during extreme knee movements due to its anatomical position and dynamic interactions with surrounding structures. In this case, the hyperflexion and external rotation mechanism were pivotal in causing acute inflammation and edema within the fat pad.
Diagnostic Evaluation
MRI findings revealed low signal intensity on T1-weighted images and high signal intensity on T2-weighted images within the infrapatellar fat pad, consistent with edema and acute inflammation. Importantly, no structural deformities, ligament injuries, meniscal tears, or other intra-articular abnormalities were observed. The absence of significant changes in the structural form of the fat pad helped rule out more severe injuries such as Hoffa’s syndrome or chronic impingement.
Management and Treatment
The player was managed conservatively with a focus on pain control and functional restoration. Nonsteroidal anti-inflammatory drugs (NSAIDs) were prescribed to manage inflammation, and partial weight-bearing with the use of crutches was recommended. The rehabilitation protocol included progressive range-of-motion exercises and gradual return to weight-bearing activities. By the end of the first week, the patient could walk unaided. Over the following weeks, supervised physical therapy sessions facilitated recovery, focusing on strengthening and proprioceptive training.
At three weeks post-injury, the player resumed light training without significant discomfort. By the sixth week, he had returned to competitive play, achieving full functional recovery. No residual symptoms or limitations were reported during a six-month follow-up period, although further imaging was declined by the patient.
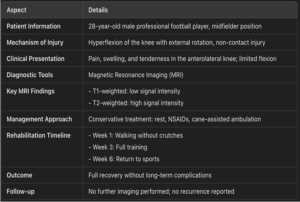
Table 1: Summary of Key Findings and Management of Infrapatellar Fat Pad Injury
Discussion
Acute infrapatellar fat pad injuries are rare, particularly in professional athletes. The clinical presentation often includes anterior knee pain, tenderness, and restricted range of motion. MRI remains the gold standard for diagnosis, enabling visualization of inflammatory changes and ruling out concurrent injuries. Conservative management is typically effective, with most patients achieving full recovery within 6–8 weeks. Surgical intervention is reserved for cases unresponsive to conservative measures or those involving structural deformities.
This case underscores the importance of understanding injury mechanisms in athletes. Video analysis of the match provided critical insights into the cause of the injury, highlighting the value of such tools in sports medicine. Moreover, this report adds to the limited literature on acute infrapatellar fat pad injuries, offering a framework for diagnosis and management.
Conclusion
This case demonstrates that acute infrapatellar fat pad injuries, while rare, should be considered in athletes presenting with anterior knee pain following hyperflexion trauma. Early diagnosis using MRI and appropriate conservative management can lead to successful outcomes, enabling athletes to return to their pre-injury performance levels. Further research is needed to better understand the long-term implications of such injuries and refine treatment protocols.
Reference
- Gallagher J, Tierney P, Murray P, O’Brien M. The infra- patellar fat pad: anatomy and clinical correlations. Knee Surg Sports Traumatol Arthrosc 2005;13:268-72.
- Dragoo JL, Johnson C, McConnell J. Evaluation and treatment of disorders of the infrapatellar fat pad. Sports Med 2012; 2:51-67.
- Yi SR, Im SH, Cho EH. Acute infrapatellar fat pad separation after contusion in the kneeling position. J Korean Orthop Assoc 2021;56:341-5