Publication Information
ISSN: 2688-0873
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Archives |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Acute Cholelithiasis Diagnostic and Therapeutic Approach: Retrospective Study of 54 Cases
Habib Elloumi*, Mouhamed Ben Slima
General Surgery Department B la Rabta Hospital
Received Date: November 23, 2022; Accepted Date: November 30, 2022; Published Date: December 06, 2022;
*Corresponding author: Habib Elloumi. Department of general surgery B la Rabta Hospital, Tunis 1007. Email: Habibledoc@gmail.com
Citation: Elloumi H, Slima M B (2022) Acute Cholelithiasis Diagnostic and Therapeutic Approach: Retrospective Study of 54 Cases. Jr Surg Opetech Anesthesia: JSOPA-117.
DOI: 10.37722/JSOTA.2022102
Abstract
Introduction
The Tokyo guide lines working group consensus conference 2018 validated diagnostic and severity criteria for acute cholangitis.
Background
To evaluate the epidemiological and clinical characteristics of our patients and to evaluate our diagnostic and therapeutic approach.
Methods
This is a descriptive retrospective study concerning 54 cases of acute cholangitis from January 2011 to December 2016 managed in B department of general surgery La Rabta Tunis.
Results
Our series includes 23 men and 31 women. The average age of our patients is 68.3 +/- 17.5 years. The Charcot triad was noted in 28 cases (51.85%). Abdominal ultrasound was performed on all of our patients, abdominal CT was performed in 12 cases and Biliary-MRI in 9 cases. Our series notes 16 grade I patients, 28 grade II patients and 10 grade III patients with acute cholangitis. Antibiotic therapy, general medical measures and resuscitation were provided to all of our patients. Cholecystectomy was performed in 39 cases. In 53 cases our patients had bile duct drainage including 36 cases (66.66%) of endoscopic drainage and 17 cases (31.48%) of surgical drainage. In our series, morbidity concerned 25 patients, i.e. (46.29%). Mortality was noted in our series in 6 cases, i.e. (11.11%).
Conclusion
Acute cholelithiasis is a pathology that affects the elderly in their sixties with a slight predominance of women. The availability of an endoscopy technical platform is essential in the care. The use of surgical drainage should only be performed in the lack of endoscopic treatment.
Keywords: Acute Pancreatitis; Angiocholitis Lithiasis; Antibiotic; Charcot’s Triad; Cholecystitis; Endoscopic Drainage; Hepatic Abscess; Surgical Drainage
Introduction
The occurrence of acute cholelithiasis has an incidence of 0.3% to 1.6% in subjects known to have cholelithiasis [1]. Most contemporary authors define acute cholangitis as a clinical syndrome combining one or all the elements of the Charcot triad in the presence of obstruction and biliary infection [2-4]. Biliary aetiology dominates over 28% to 70% of the causes [5-6].
Objectives
We aim to evaluate the epidemiological and clinical characteristics of our patients and to evaluate our diagnostic and therapeutic approach referring to the review of literature.
Materials and methods
This is a descriptive retrospective study of 54 cases acute cholelithiasis, ranging from January 2011 to December 2016. This study was conducted in the department of visceral and digestive surgery B, of the la Rabta hospital in Tunis. The observations included in our work are those of patients over 18 years admitted to our surgical department for the management of acute cholelithiasis. The diagnosis and the severity criteria were based on clinical biological and radiological parameters referring to the Tokyo guides lines recommendations of 2018 [7]. The diagnosis of cholecystitis was based on clinical, biological and radiologic matching with the diagnosis criteria of the Tokyo guide lines 2013[8]. All of our patients did get perfusion, antispasmodic, stomach protection, antibiotic and reanimation measures when it was needed according to the SFAR recommendation [9] and Tokyo guides lines recommendations [10]. The treatment was performed according to the decisions of the surgeons, surgically in several cases and when it was possible endoscopically and revised by the Tokyo guide lines recommendations of 2018 [7]. The data concerned epidemiological characteristics, Clinical status, radiological data, surgical data, endoscopic data, morbidity and Mortality particularities were saved on a SPSS.20 program for descriptive analyses.
Results -Interval: [34-96]
-peak: [80-90]
-Incidence: 9 cases/year -(23) men -Hyperlipidaemia:(25) -Blood hyper-pressure: (21) -Diabetes: (7) -chronic heart failure :(5) -chronic respiratory failure :(5) -laparoscopic cholecystectomy (11) –without organ failure (17) –with severity signs (11): -septic shock (6) -Heart failure: (1) -Respiratory failure (1) -Renal failure with haemostasis troubles (1) -Renal failure with pancreatitis grad D (1) Complicated diabetes with hepatic abscess (1) Truncated forms: (26) -Abdominal pain with fever: (15) -Isolated abdominal pain (3) -Fever and alteration of general condition (2) -Fever and jaundice (6) -cholecystitis (8) -Dilated bill duct with lithiasis (28). -Dilated bill duct without lithiasis (26) -Grad D pancreatitis (1) -cholecystectomy (4) -Non complicated gallbladder (6) -Cholecystitis (2) -Bill duct with stone (9) -Bill duct without stone (3) -Hepatic abscess (1) 4cm segment VII 3cm segment V -Bill duct with stone (9) -Cholecystitis (4)
Our series includes 23 men and 31 women with an incidence of 9 cases / years and a sex ratio of 0.72. The average age of our patients is 68.3 +/- 17.5 years with extremes from 34 to 96 years. The obesity and the dyslipidemia were noted in 19 and 25 cases, respectively. Type 2 diabetes and high blood pressure were marked in 7 and 21 cases, respectively. Heart and respiratory failure were noted in 5 cases. In more than 11 cases laparoscopic cholecystectomy was performed. The consultation time was 3.7 +/- 2.2 days from the onset of symptoms. Abdominal pain and fever were the most frequent functional signs with respectively 47 cases (88%) and 45 cases (87%). Jaundice was present in 34 cases (63%) Mental confusion was noted in 5 cases (9.23%) and haemodynamic instability was noted in 6 cases (11.11%). Charcot’s triad was noted in 28 cases (51.85%) and truncated forms were noted in more than 26 cases (48.15%). A hyperleukocytosis above 10,000 GB / ml was marked in more than 42 cases (77%) and a CRP above 10 U / ml was marked in all our patients. Cholestasis was noted in 47 cases (88%).Transaminases were superior to 1.5 the universal normal limite in 47 cases for (ASAT) (87.03%) and in 46 cases for (ALAT) (85.18%). A bilirubinemia was above 34 U / I in 34 cases (63%). Lipasemia was in 3 cases elevated 3 time above the lower limit. A thrombocytopenia was noted in 3 cases. Blood cultures were not performed due to lack of reagent. An abdominal ultrasound was performed on all our first-line patients; it noted in 35 cases (64.81%) a noncomplicated gallbladder lithiasis, a lithiasic cholecystitis in 8 cases (14.81%), a dilation of the bile ducts with lithiasis of the main bile duct in 28 cases (51.85%) and a dilation bile ducts without individualized stones in 26 cases (48.14%). Abdominal CT scan was performed in 12 cases (22.22%). This examination was performed in 3 cases for grading of acute pancreatitis, in 7 cases for stones of the main bile duct and in 2 cases following for a suspicion of tumour obstacle at the bilious-pancreatic junction. The CT scan revealed, 2 grade C pancreatitis, one grade D pancreatitis, 6 cases of gallbladder lithiasis, 2 cases of cholecystitis, dilation of the bile ducts in all our patients including 4 cases on a cholecystectomized patient and 1 case of hepatic abscess 4 cm at segment VII. MRI was performed in 9 cases (16.66%) in all cases looking for stones in the main bile duct. The examination revealed in 9 cases the presence of stones at the bile duct, a cholecystitis in 4 cases and in 1 case hepatic abscess of 3 cm in segment V. In 14 cases (25.92%) morphological explorations did not reveal any stones in the dilated bile ducts in 9 cases on lithiasic gall bladder, in 4 cases on acute cholecystitis and in 1 case on a cholecystectomized patient. Our series noted the presence of 14 cases of acute lithiasic cholecystitis [table1].
Age and incidence
Sex (cases)
Medical background (cases)
Clinical presentation (54 cases)
Ultrasound findings (54 cases)
Scanner findings (12 cases)
MRI findings (9 cases)
-Mean: 68,3+/17,5
-(31) women
– Obesity:(19)
Charcot syndrome:(28):
-Non complicated gall bladder lithiasis (35)
-Grad C pancreatitis (2)
-Hepatic abscess (1)
The re-evaluation of our cases by the diagnosis criteria of the Tokyo guidelines working group lines 2018 revealed that all our patient has combined A.2, B.2 and C1 criterion for acute cholelithiasis diagnosis [table 2].
Diagnostic criteria
N ( 54 )
%
A-1: Fever or chill > 38° C
47
87,03 %
A-2: Biological inflammatory syndrome: -Leucocytes < 4 or > 10G/L -CRP >10 mg/L
54
100% criterion A-2
B-1: Jaundice (bilirubinemia > 34µmmol/L)
34
62,96%
B-2 Abdominal liver function tests ( ASAT, ALAT, PAL, GGT > 1,5 the limit of normal)
54
100% criterion B2
C-1: Dilatation of the bill duct
54
100% criterion C1
C-2: Evidence of etiology on image suspected diagnosis
40
74,07%
Suspected diagnosis : Item A +B/C
0
0
Certain diagnosis : Item A +B+C
54
100%
According to Tokyo working group lines 2018 we noted 16 patients grade I, 28 patients grade II and 10 patients grade III of severity with acute cholangitis [table 3].
Criteria
Grade I: 16 cases
Grade II: 28 cases
Grade III: 10 cases
Fever >39 °C + bilirubinemia >85*mmol/L
–
4
–
Age >75 years old + Leucocytes >10G or <4G/L
–
19
–
Leucocytes >10G or <4G/L+bilirubinemia >85*mmol/L
–
5
–
-Hypoalbuminemia < 0,7 × LIN
-0
0
-0
Leucocytes >10G or <4G/L
11
–
–
Confusion
5: all in septic shock
Heart failure
1
Respiratory failure
1
Renal failure
1
Septic shock
6
Hemostasis disorder
1
Cholecystitis
4
6
4
Hepatic abscess
0
1 segment V (3 cm)
1 segment VII (4 cm)
Pancreatitis
1 : Grad C
1
2 : Grad C-Grad D
The time taken for medical treatment for patients is as follows: 3.5 day + / – 2.34 for grade I, 3.81 day + / – 2.07 for grade II and 4 day + / – 1.85 for grade III. All our patients had fluid intake according to their needs, analgesic and antispasmodic treatment, administration of vitamin K and monitoring of constants. Intensives care were applied to 10 cases in grade III. Antibiotic therapy in our series was administered upon admission as follows: For grade I patients: (Cephalosporin 3rd Generation + gentamicin + Metronidazole) in 15 cases and in 1 case under (C3G + Metronidazole) for a duration of 20, 12 + / – 3, 28 days. For grade II patients: (Cephalosporin 3rd Generation + gentamicin + Metronidazole) in 25 cases, (Amoxcillin-clavulanic. Acid) in 2 cases and 1 case under (Cephalosporin 3rd Generation + Metronidazole) for a duration of 19, 21 +/- 4.4 days. For grade III patients: (Cephalosporin 3rd Generation + gentamicin + Metronidazole) in 4 cases and under (Cephalosporin 3rd Generation + Metronidazole) in 6 cases for a duration of 14, 21 +/- 11, 38 days. Grade I patients underwent first-line surgical drainage in 10 cases (7cases of Kehr drainage; 3 cases of trans-cystic drain) (62.5%) with a delay of 5.2 +/- 1.52 days and endoscopic drainage in 6 cases (37.5%) with a delay of 5 +/- 1.41 days. Grade II patients underwent first-line surgical drainage in 5 cases (3 cases of Kehr drainage, 1 cases of trans-cystic drain, 1 case of biliary-digestive anastomosis) (17.85%) with a delay of 4.2 +/- 0.83 days and endoscopic drainage in 23 cases (82.5%) with a delay of 5.21 +/- 1.53 days. Grade III patients underwent first-line surgical drainage in 2 cases (2 cases of Kehr drainage) (20%) with a delay of 2 days and endoscopic drainage in 7 cases (70%) with a delay of 2.57 +/- 1.51 days, in 1 case the patient died before the drainage. Grade I patients underwent cholecystectomy in 14 cases, including 3 cases for acute cholecystitis with a delay of 6.4 +/- 1.41 days and 11 cases for gallbladder lithiasis. The grade II patients underwent cholecystectomy in 19 cases including 6 cases for acute cholecystitis with a delay of 8.33 J +/- 1.88 and 13 cases for gallbladder lithiasis. Grade III patients underwent cholecystectomy in 6 cases including 4 cases for acute cholecystitis with a delay of 5.99 J +/- 1.24 and 2 cases for gallbladder lithiasis. Cholecystectomy was not performed in 4 patients who were in septic shock of which 3 cases had gallbladder lithiasis and 1 case of cholecystitis died before treatment. The 3 cases of acute pancreatitis received general resuscitation measures and antibiotic therapy: in 2 cases under (Cephalosporin 3rd Generation + gentamicin + Metronidazol) for a duration of 28 days. In 2 cases a cholecystectomy and a biliary drainage have been performed in the same hospitalisation. In one case the patient died from organs failure. The two cases of abscess that responded to resuscitation measures had respectively endoscopic drainage on Day-2 and on Day-8 of management and cholecystectomy with trans-cystic drainage in one case at Day-33 and cholecystectomy coupled with the placement of a Kehr drain in a case at Day-12 [table 4]. -Grad II: 3.81 day +/- 2.07 -Grad III: 4 day +/- 1.85 -C3G + Metronidazole (1) -Duration of 20, 12 + / – 3, 28 days -Amoxicillin+clavulanic. Acid (2) -Cephalosporin 3rd Generation+ Metronidazole (1) -Duration of 19, 21 +/- 4.4 days -Cephalosporin 3rd Generation+ Metronidazole (6) -Duration of 14,21 +/- 11, 38 days -Grad I: 5.2 +/- 1.52 days -Grad II:4.2 +/- 0.83 days -Grad III: 2 days -Kehr drainage 7 cases -Trans-cystic drain 3 cases – Kehr drainage 3 cases. – Trans-cystic drain 1 case -Bili-digestive anastomosis 1 case. – Kehr drainage 2 cases. -Grad I: 5 +/- 1.41 days -Grad II: 5.21 +/- 1.53 days -Grad III:2.57 +/- 1.51 days (1 case is dead before treatment) -Non complicated gall bladder lithiasis (26) -Cholecystitis (13) -6.74 day +/- 1.46 Cholecystectomy -Grad I: 6.4 day +/- 1.41 -Grad II: 8.33 day +/- 1.88 -Grad III : 5.99 day +/-1.24 11 3 13 6 2 (3 were not performed, the patients died from septic shock) 4 (one was not performed, the patient died from septic shock) -Case 1: 7 day -Case 2: 3 day -Sphincterotomy with extraction of lithiasis. – Cephalosporin 3rd Generation + gentamicin + Metronidazole for 28 day. -Cholecystectomy the 12th day Sphincterotomy with extraction of lithiasis. – Cephalosporin 3rd Generation + gentamicin + Metronidazole for 28 day -Cholecystectomy the 33th day. (1 case is dead before treatment) -Case 1: 8 day -Case 2: 2 day -Sphincterotomy with extraction of lithiasis. – Cephalosporin 3rd Generation + gentamicin + Metronidazole for 15 day -Cholecystectomy the 12th day -Sphincterotomy with extraction of lithiasis – Cephalosporin 3rd Generation + Metronidazole for 22 day. -Cholecystectomy the 33th day
Therapeutic management
Delay
Gard I (16)
Grad II (28)
Gard III (10)
Antibiotic
-Grad I: 3.5 day +/- 2.34
-Cephalosporin 3rd Generation + gentamicin + Metronidazole: (15)
-Cephalosporin 3rd Generation + gentamicin + Metronidazole: (25)
-Cephalosporin 3rd Generation + gentamicin + Metronidazole: (4)
Surgical treatment
Biliary drainage
-Surgical drainage in 10 cases:
– Surgical drainage 5 cases:
– Surgical drainage 2 cases:
Endoscopic treatment
Biliary drainage
–Sphincterotomy with extraction of lithiasis 6 cases
–Sphincterotomy with extraction of lithiasis 23 cases
–Sphincterotomy with extraction of lithiasis 7 cases
Cholecystectomy:
Cholecystectomy
Pancreatitis (3)
Biliary drainage
Case 1:
Case 2:
Hepatic abscess (2)
Cholecystectomy
Case 1:
Case 2:
Patients of grade I present 3 cases of morbidity which followed surgical drainage (Kehr) with an average drainage time of 96 hours, we cite: 2 cases of residual lithiasis of which 1 case is associated with a renal failure and 1 case of nosocomial bronchopneumonia for a hospital stay of 19.67 +/- 4.5 days and 1 case followed endoscopic drainage carried out on day 7 of treatment resulting in a residual lithiasis for a duration of 22-day hospitalization. Patients of grade II present 5 cases of morbidity followed surgical drainage (Kehr) with an average drainage time of 96 hours, we cite: 2 cases of wound infections , 1 case of nosocomial bronchopneumonia, 1 case of biliary fistula and 1 case of sub-phrenic collection for an hospital stay of 19.67 +/- 2.88 days and 7 cases followed endoscopic drainage with an average delay of 96 hours, we cite: 3 cases of acute pancreatitis, 1 case of residual lithiasis, 1 case of cariogenic failure, 1 case of pulmonary embolism and 1 case of hyperomolar coma who died on day 10 of treatment for an average hospital stay of 19.75 + / – 3.88 days. The patients of grade III presented 9 cases of morbidity, including one case of septic shock died during conditioning and activation of resuscitation means on day-1, 2 cases of septic shock followed surgical drainage (Kehr) with an average drainage time of 24 -72 hours, and 2 cases of septic shock of which 1 case died on day 1 of treatment, 1case of pulmonary embolism, 1 case of residual lithiasis, 2 cases of renal failure including 1 case associated with respiratory distress who died on day 28 care followed endoscopic drainage with an average delay of 48 hours. Death concerned 6 patients including, 5 cases in grade III with septic shock and 1 case of hyperomolar coma associated to a renal failure in grade II. On a follow-up which took place over a period ranging from 3 years to 9 years with the follow-up of 48 surviving patients, we note the occurrence of 4 cases of eventration on the right subcostal, 1 case of cholangitis on inflammatory stenosis of the lower part common bile duct and a case of cholangitis on residual lithiasis that did have an endoscopic treatment previously [table 5]. -Grad I: 4 days. -Grad II:4.days -Grad III: 2-3 days -1 case of residual lithiasis. -1 case of residual lithiasis and renal failure. -1 case of nosocomial bronchopneumonia – 2 cases of wound infections – 1 case of nosocomial bronchopneumonia -1 case of biliary fistula -1 case of sub-phrenic collection . – 2 cases of septic shock the 2 cases died later –1 case died before treatment -Grad I: 7 days -Grad II: 4 days -Grad III: 2 days -1 case of residual lithiasis – 3 cases of acute pancreatitis – 1 case of residual lithiasis -1 case of cariogenic failure -1 case of pulmonary embolism -1 case of hyperomolar coma: Died later -2 cases of septic shock of which one case died. -1 case of pulmonary embolism, -1 case of residual lithiasis -1 cases of renal failure -1 cases of renal failure with respiratory distress 1 case died. – 1 case of cholangitis on an inflammatory stenosis of the bill duct treated endoscopically. -1 case of cholangitis on a residual lithiasis treated endoscopically.
Therapeutic management
Delay
Gard I (16)
Grad II (28)
Gard III (10)
Surgical treatment
Biliary drainage
-Surgical drainage in 3 cases:
– Surgical drainage 5 cases:
– Surgical drainage 2 cases:
Endoscopic treatment
Biliary drainage
-Sphincterotomy with extraction of lithiasis 1 cases:
-Sphincterotomy with extraction of lithiasis 7 cases:
-Sphincterotomy with extraction of lithiasis 7 cases:
Late Outcomes
-3 cases of eventration treated by Kehr drainage.
-1 case of eventration treated by Kehr drainage.
Discussion
Acute lithiasic cholangitis is a pathology that affects old subjects with an average age of 52 to 74 years [11]. This may be explained by the long course of lithiasis disease before it becomes symptomatic [1]. The female predominance could be explained by their superiority in having non complicated gallstone carriers and by the bile over saturation more marked in women. The large cases of obesity and dyslipidemia among our patients is harmonious with literature data where it’s established that pregnancy, obesity, weight loss, hypertriglyceridemia, treatment with oestrogens are likely to cause supersaturation of bile in cholesterol, thus constituting the lithiasis disease [12]. Cases of arterial hypertension, diabetes type 2, coronary artery disease, heart failure and renal failure were noted in our series, these morbidities are matching with the high age of our patients consulting for acute cholangitis; information on our patient’ comorbidities allowed us to assess their background and defects with a view to establish a diagnosis of severity and an appropriate treatment. The large delay of the consultation time in our series would be explained by the neglect of the symptomatology by the patients, by a difficult access to care for some of them or by an error in the diagnosis. The abdominal pain is the earliest and the most frequent sign, it is caused by the distension of the bile duct [2-4]. The fever comes in the second place in terms of frequency after abdominal pain followed by jaundice as an inconstant sign [2]. The examination reveals a tenderness or a defence of the epigastrium or the right hypochondrium [3] which is concordant to our results. The Charcot triad has a variable frequency from one author to another, from 22 to 72% [2]. The Haemodynamic failure is a consequence of the sepsis it varies according to the authors from 7 to 32% [2 -4]. In biological terms, in acute cholelithiasis, neutrophilic leukocytosis is found in one in 2 patients [12]. The hepatic assessment is disturbed in 90% of cases in cases of symptomatic bile duct lithiasis [12]. Markers of cytolysis are elevated in 80% of cases [11]. According to a meta-analysis made by Abboud and al, the abdominal ultrasound has a low sensitivity and low specificity to reveal stone in the principal bile duct that matches with our results, explained by the operative character depending on ultrasound, by the difficulty of exploring the bottom of the bile duct which could be hampered by digestive gases or by possible calculus migration [13]. Abdominal CT scan with or without injection is more sensitive and specific than abdominal ultrasound in the diagnosis of acute cholangitis regardless of its cause [14]. Biliary-MRI can individualize and locate stones in the bile duct [15], in our series the biliary-MRI allowed us to objectify stones in the main bile duct not objectified by abdominal ultrasound [figure1].
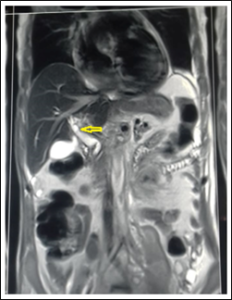
Figure 1: common bile duct lithiasis at the biliary convergence (MRI).
The limits of this examination are its unavailability in emergency as was often the case in our series [16]. The diagnosis of acute cholangitis is consensual by a multidisciplinary meeting of international experts held in Tokyo in 2007 which led to the development of a diagnostic score including biological and radiological criteria with a sensitivity of 80 to 83% [17]. This score was revised in 2013 and maintained in 2018 [1] [7]. The evolution of the acute cholangitis is full of complications including: septic shock that occurs in 4 to 32% [2], the renal failure which is due to septic status and to the toxicity of conjugated bilirubin [18] and The altered state of consciousness that occurs in 5 to 16% of cases [3][4]. The decompensation of tares can occur in acute cholangitis as a result of the sepsis [5]. The biliary acute pancreatitis may be caused by the migration of a stone and its entrapment in the Vater ampulla [12]. The occurs of a biliary hepatic abscess is due to implantation in the liver of pyelophlebitis via biliary and venous reflux [3][4]. Cholecystitis results from a persistent entrapment of a stone, it occurs in 20% of subjects with symptomatic gallstones [19] and in 10 to 20% of under diagnosed patients [20]. The positive diagnosis and that of the severity of acute cholecystitis and cholangitis is well defined by the Tokyo guide lines working group [1] [21]. Acute cholangitis is a medico-surgical emergency, management must be initiated without delay, it is based on three essential elements: Antibiotic treatment, resuscitation measures for organ failures and drainage of the principal bile duct [22] [23]. The antibiotic therapy is initially empirical and must be adapted to the results of biliary cultures and blood cultures for a therapy that targets microorganisms [24]. The Tokyo guides lines working group suggested an antibiotic therapy which matches with the grad of severity, it recommends a monotherapy for mild forms compared to moderate to severe forms, the combination of penicillin and a beta-lactamase inhibitor is recommended as first-line treatment; Piperacillin-Tazobactam is strongly recommended if Pseudomonas is suspected [10]. The Tokyo guides lines working group recommend a duration of antibiotic therapy of 4 to 7 days after the control of the source of infection, a duration of 7 to 10 days if the presence of a prosthesis and a duration of 2 weeks for enterococci and streptococci [10]. The biliary drainage in combination with targeted antibiotic therapy is a grade A recommendation of the Tokyo guide lines [23]. Drainage of the bile duct is a radical method of obstacle removal and it is a centrepiece in the management of cholelithiasis [25]. Several means have been described for the drainage of the bile ducts, to be mentioned: surgical drainage, whether by laparoscopic or right subcostal route, endoscopic drainage and percutaneous trans-hepatic drainage [22]. According to the Tokyo guide lines work group, the type of biliary drainage and its timing depend on the severity grade of the acute cholangitis. For grade I in most cases, medical treatment is sufficient, biliary drainage is not systematic, it is only indicated in the event of non-response to medical treatment [25]. Choledotomy and stone extraction or endoscopic drainage may also be performed [25]. For grade II patients, trans-papillary drainage is indicated and must be performed early, not exceeding 48 hours [22] [25]. In case of failure of stone extraction, a nasal-biliary drain should be placed, a bloated dilation is performed, and stone extraction and cholecystectomy will take place in a second step [25]. If less invasive techniques are unavailable, surgical drainage can be performed [26]. For grade III patients, resuscitation measures and empiric antibiotic therapy should be initiated [23]. Endoscopic or percutaneous drainage should take place within 24 hours [figure2] [22] [25].
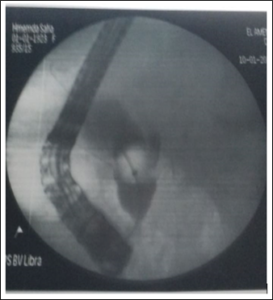
Figure 2: Extraction of a calculation from the bottom of the bile duct by an endoscopic treatment.
In our series, endoscopic drainage was performed in most cases as the first intention; however, surgical drainage was still performed despite its high morbidity and mortality due to the choice of certain surgeons in the department and / or due to the unavailability of endoscopic treatment. It should be noted that in our series we are far from the deadlines of the biliary drainage proposed by the Tokyo guides lines working group. This may be explained by the absence of an endoscopy department at the Rabta hospital, the routing of patients to the endoscopy units as well as the material necessary for the act of drainage depends on logistical means which are sometimes difficult to make available; It should be noted that in some situations, resuscitation measures and patient preparation for endoscopic or surgical drainage delay drainage. It’s recommanded to realize cholecystectomy when it’s possible to prevent posterior complications in the cases of acute cholelithiasis [27]. The cholecystectomy for the cases of cholecystitis in our work were not conform to the Tokyo guide lines recommendations for several reasons : first of all, we had to operate grade III cholecystitis in some cases because of the lack of percutaneous cholecystostomy skills and secondly, we did not respect the timing of cholecystectomy as refereed to its severity grade in the TG18 recommendations in a way that in most of the cases biliary drainage is done before the cholecystectomy which delay it [28]. The hepatic abscess can be managed in association to an adapted antibiotic therapy by trans-hepatic drainage or surgical drainage in the case of fail of the percutaneous drainage or in the presence of a voluminous abscess [29], in our cases percutaneous drainage was deemed unnecessary as the abscesses were small, poorly collected and well controlled with medical treatment. In the event of biliary pancreatitis, endoscopic treatment by sphincterotomy and unobstructed bile duct is a definite indication according to most authors regardless of the severity [30]. In the literature, the incidence of morbidity is in the order of 12 to 34% for open surgery [31-32] and 3 to 14% for endoscopic drainage [33-34]. The morbidity is higher in our results than in the literature because of the use of surgical drainage, the critical status of some grade III patients, the nonadapted antibiotic therapy and the late timing of the drainage of the bile duct; that are morbidity factors in the literature [35] [36]. Nonspecific complications after biliary drainage have been widely described in the literature; they include decompensation of organs and / or defects, nosocomial infections and thromboembolic complications [37] [38]. The pancreatitis is the most frequent complication of the endoscopic treatment, as we did report in our work, it may be due to injections in pancreatic duct [39]. It’s reported that the incidence of residual lithiasis is nearly the same in surgical and endoscopic works [40], we have to notice that we did had more residual lithiasis after endoscopic drainage. The occur of sub-phrenic collection and biliary fistula like we did note in our work are described as surgical complication [41] [42]. Multiple factors of poor prognosis relating to the management of acute cholangitis have been described in the literature, including the presence of organ failure, the use of mechanical ventilation and vasoactive drugs, age at- beyond 75 years, the presence of comorbidities, thrombocytopenia, hyperbilirubinemia, the delay in the introduction of antibiotic therapy and that of biliary drainage, which may explicate the cases of mortality in our work [35] [36]. Recurrent lithiasis are described in the literature with a prevalence of 5.3% for the endoscopic series [33] [38] and a prevalence of 2 to 14% for the surgical series [40]. Our series includes 2 case of acute cholangitis after endoscopic treatment as late complication in the first case that was a stenosis of the bile duct it could be due to oddian stenosis or loss of oddian function [43] and in the second case due to a recurrent lithiasis [33] [38]. The occurs of an eventration is described in the literature, many risk factors are involved such as age, male sex, high BMI, technical factors, factors of increased abdominal pressure and by infection of the walls, most patients that had a late eventration did have those risk factors [44].
Conclusion
Acute cholelithiasis is a pathology that affects people in their sixties with a slight predominance of women. Abdominal pain and fever are the most common clinical signs; Charcot’s triad is noted in 1 in 2 cases. Ultrasonography, abdominal computed tomography and Biliary-MRI are essential for the diagnosis of acute cholangitis. The positive diagnostic criteria and severity of the Tokyo working group 2018 guidelines are easily applicable and allow the patient’s prognosis to be assessed and the organization of better care in effect. Endoscopic drainage carrying out a sphincterotomy and stone extraction coupled with an appropriate antibiotic therapy must be performed without delay depending on the grade of severity. Collaboration with the bacteriology laboratory, blood culture and biliary culture is important in the management. The availability of a local endoscopy technical platform is essential in the management of acute cholelithiasis. Surgical drainage of the main bile duct should be avoided for severe forms.
Competing interests: The authors declare no competing interest.
Authors’ contributions: All the authors participated in the conception of the manuscript; Habib Elloumi wrote the manuscript and Mohamed Ben Slima critically revised the successive versions. All authors have read and agreed to the final version of this manuscript.
Acknowledgements: This research was made possible through the support and work of the archive staff of surgical B department of the Rabta hospital.
References
- Kiriyama S, Takada T, Strasberg SM, Solomkin JS , MayumiT, Pitt HA et al. TG13 guide lines for diagnosis and severity grading of acute cholangitis (withvideos). J Hepato-Biliary-Pancreat Sci 2013; 20:24-34.
- Csendes A, Diaz JC, Burdiles P, Maluenda F, Morales E. Riskfactors and classification of acute suppurative cholangitis. Br JSurg .1992; 79:655-8.
- Boey JH, Way LW. Acute cholangitis. Ann Surg . 1980;191(3):264-70.
- O’Connor MJ, Schwartz MJ, McQuarrie DJ et Sumner HW. Acute bacterial cholangitis: an analysis of clinical manifestation. Arch Surg. 1982; 117:437-441.
- Kimura Y, Takada T, Kawarada Y,Nimura Y,Hirata K,Sekimoto M et al. Definitions, patho-physiology, and epidemiology of acute cholangitis andcholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg.2007; 14:15-26.
- Gomi H, Takada T, Hwang T-L, AkazawaK, Mori R, Endo I et al. Updated compre-hensive epidemiology, microbiology and outcomes among patients with acute cholangitis. JJ Hepato-Biliary-Pancreat Sci.2017; 24:310-8.
- Yokoe M, Hata J, Hata J, Strasberg SM, Asbun HJ, Takada T, Wakabayash G et al.Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (withvideos). J Hepato-Biliary-Pancreat Sci.2018; 25:41-54.
- Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T,Gomi H, et al. New diagnostic criteria and severity assessmentof acute cholecystitis in revised Tokyo guidelines. J Hepatobiliary Pancreat Sci. 2012; 19:578-85.
- Quenot JP, Milési C , Cravoisy A, Capellier G, Mimoz O, Fourcade O and al.Intrahospital transport of critically ill patients (excluding newborns) recommendations of the Société de Réanimation de Langue Française (SRLF), the Société Française d’Anesthésie et de Réanimation (SFAR), and the Société Française de Médecine d’Urgence (SFMU).Quenot et al. Annals of Intensive Care 2012 ; 2:1.
- Gomi H, SolomkinJS, Schlossberg D, Okamoto K ,Takada T, Steven M et al. Tokyo Guidelines 2018: antimicrobial therapy for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 2018; 25:3-16.
- Ennabli K, Jemni M. Etude analytique de 80 cas d’angiocholite lithiasique. J Chir 1984; 121:187-94.
- Pariente A. Lithiase biliaire. Encycl Méd Chir (Elsevier, Paris), AKOS Encyclopédie Pratique de Médecin.1998; 1:1-4.
- Abboud PA, Malet P, Berlin JA , Staroscik R, Michael, Cabana M et al. Predictors of common bile duct stones prior to cholecystectomy: a metaanalysis. Gastrointest Endosc. 1996; 44:450-7.
- Kim SW, Shin HC, Kim HC, HONG M, KIM I Y. Diagnostic performance of multi-detector CT for acute cholangitis: evaluation of a CT scoringmethod. Br J Radiol.2012; 85:770-7.
- Singh A, Mann HS, Thukral CL, Singh NR. Diagnostic accuracy of mrcp as compared to ultrasound/ct in patients with obstructivejaundice. J Clin Diagn Res. 2014;8 :103-7.
- Dalton SJ, Balupuri S, Guest J. Routine magnetic resonance cholangiopancreatography and intra-operative cholangiogram in the evaluation of common bile duct stones. Ann R Coll Surg Engl. 2005; 87:469-70.
- Wada K, Takada T, Kawarada Y, Nimura Y, Miura F, Yoshida F et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007; 14:52-8.
- Dawson JL. Jaundice, Septic Shock, and Acute Renal Failure. Am J Surg .1968; 115 (4):516-18.
- Ansaloni L, Pisano M, Coccolini F, Peitzmann AB, Fingerhut A, Catena F et al. 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg.2016; 11, 25.
- Strasberg SM. Acute calcolous cholecystitis. N Engl J Med. 2008; 358:2804-11.
- Kiriyama S, Takada T, Hwang TL, Akazawa H, Miura F, Gomi H. Clinical application and verification of the TG13 diagnostic and severity grading criteria for acute cholangitis: An international multicenter observational study. J Hepatobiliary Pancreat Sci. 2017; 24:329-337.
- Sokal a, A. Sauvanetb, B. Fantina,c, V. de Lastoursa Angiocholites : diagnostic et prise en charge Journal de Chirurgie Viscérale (2019) 156, 552-563.
- Miura, T. Takada, Y. Kawarada Y, Nimura Y, Wada K, Hirota M et al. Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg.2007; 14:27-34.
- Reuken PA, Torres D,Baier M,Löffler B, Lübbert C,Lippmann N et al. Risk factors for multi-drug resistant pathogens and failure of empiric first-line therapy in acute cholangitis. PLoS One. 2017; 12:1-12.
- Mukai S, Itoi T, Baron TH, TakadaT, StrasbergSM, Pitt HA et al. Indications and techniques of biliary drainage for acute cholangitis in updated Tokyo Guide-lines 2018. J Hepato-Biliary-Pancreat Sci.2017; 24:537-549.
- Saltzstein EC, Peacock JB, Mercer LC. Early operation for acute biliary tract stone disease. Surgery. 1983; 94:704-8.
- Boerma D, Rauws E, KeulemansY, Janssen I, Bolwerk C, Timmer R. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. THE LANCET. 2002; 360(9335):761-765.
- Yamashita Y, Takada T, Kawarada Y, Nimura Y, Hirota M, Miura F, et al. Surgical treatment of patients with acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007; 14:91-7.
- Chichea L, Dargèreb S, Le Pennecc V, Dufaya C, Alkofera B. Abcès à pyogènes du foie. Diagnostic et prise en charge Pyogenic-liver abscess: Diagnosis and management. Gastroentérologie Clinique et Biologique.2008. 32:1077-1091.
- Neoptolemos JP, London NJM, Carr-Locke DL. Assessement of main pancreatic duct integrity by endoscopic retrograde pancréatographie in patients with acute pancreatitis. Br J Surg .1993; 80:94-9.
- Moreaux J. Traditional surgical management of common bile duct stones: a prospective studyduring a 20-year experience. Am J Surg. 1995; 169(2) :220-6.
- Hacker KA, Schultz CC, Helling TS. Choledochotomy for calculous disease in the elderly. Am J Surg. 1990; 160:610-613.
- Sugiyama M, Atomi Y. The benefi ts of endoscopic nasobiliary drainage without sphincterotomy for acute cholangitis. Am JGastroenterol .1998; 93:2065-8.
- Tranter SE, Thomson MH. Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br JSurg. 2002 ; 89 :1495-04.
- Shimada H, Nakagawara G, Kobayashi M, Tsuchiya S, Kudo T, Morita S. Pathogenesis and clinical features of acute cholangitis accompanied by shock. Jpn J Surg .1984;14:269-77.
- Andrew DJ, Johnson SE. Acute suppurative cholangitis, a medical and surgical emergency. A review of 10 years. Am J Gastroenterol 1970; 54:141–54.PMID: 5458220.
- Moreaux J. Traditional surgical management of common bile duct stones: a prospective studyduring a 20-year experience. Am J Surg. 1995; 169:220-6.
- Bourgeois N, Jeanmart J, Costamagna G,Delhaye M, Ansay J,Cremer M. L’angiocholite aiguë: Une indication particulière de ľendoscopie agressive précoce. Acta Endosc. 1986; 16:195-203.
- Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. Guidelines on the management of common bile duct stones (CBDS). Gut.2008; 5:1004-21.
- Thompson JE, Tompkins RK, Longmire WP Jr. Factors in management of acute cholangitis. Ann Surg. 1982; 195:137-45.
- Gillatt DA, May RE, Kennedy R, Longstaff Complications of T-tube drainage of the common bile duct. Ann Royal CollSurgEngl. 1985; 67:370-371. PMCID: PMC2498080.
- Maghsoudi H, Garadaghi A, Jafary GA. Biliary peritonitis requiring reoperation after removal of T-tubes from the common bile duct. Am J Surg 2005;190(3):4303.
- Mallery JS, Baron TH, Dominitz JA, Eisen GM, Faigel DO. Complications of ERCP. Gastrointest Endosc. 2003;57(6):633-8. doi: 10.1053/ge.2003.v57.amge030576633.
- Pavlidis TE, Galatianos IN, Papaziogas BT, Lasaridis CN, Atmatzidis KS, Makris JG et al. Complete dehiscence of the abdominal wound and incriminating factor. Eur S-Surg. 2001; 167;351-355.