Publication Information
ISSN: 2688-0873
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Archives |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
A Test to Evaluate the Mobility of Trochanter over Acetabulum during Performing Artificial Hip Replacement
Le Phuc*
Senior Consultant surgeon of Saigon International Traumatology Orthopaedics Hospital, HoChiMinh City, Vietnam
Received Date: August 20, 2020; Accepted Date: August 31, 2020; Published date: September 09, 2020;
*Corresponding Author: Le Phuc, Senior Consultant surgeon of Saigon International Traumatology Orthopaedics Hospital, HoChiMinh City, Vietnam. Email: leanhuyen108@gmail.com
Citation: Phuc L (2020) A Test to Evaluate the Mobility of Trochanter over Acetabulum during Performing Artificial Hip Replacement. Jour of Surg, Opera Tech and Anes: JSOTA-112.
Abstract
Most hips for arthroplasty are stiff due to chronic inflammation of surrounding structures. To perform the Artificial Hip Replacement, surgeon must release the soft tissue around the hip if necessary. To decide release or not, we use a test to evaluate the mobility of trochanter over the acetabulum.
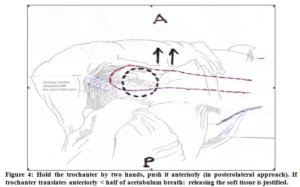
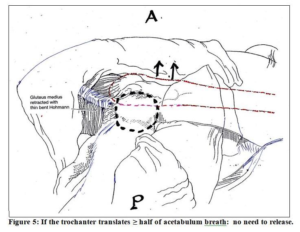
The test performed during operation. After skin and fascia incision, removal of femoral head let the hip completely free (no retractor, bone elevator, hook, etc. in surgical field). Hip and Knee (of the operated limb) in neutral position. Hold the trochanter by two hands, push it anteriorly (in posterolateral approach); push it posteriorly (in anterior approach). If the trochanter translates anteriorly (or posteriorly) less than half of acetabulum breath: soft tissue release is justified. If trochanter translation is more than half of acetabulum breath: no need to release. Balancing well soft tissue around the hip, we have a good or excellent Hip Arthroplasty, not too tight, not too loose. That is the beneficial application of the test.
Keywords: A Test to Evaluate; Acetabulum; Half of Acetabulum Breath; Hemi or Total Hip Arthroplasty; Mobility of Trochanter; Release of Soft Tissue
Introduction
Anatomical structures around the hip includes capsule (anterior, posterior, lateral and medial), ligaments, tendons and muscles. When hip deteriorates to the extent of needing artificial joint, these structures usually become contracture. To perform an arthroplasty, the hip must be loose enough for acetabular exposure, and obtain a functional artificial hip. Figure 1. If no release or not sufficient release, the head of prosthesis risks of inability to be placed in the acetabulum.
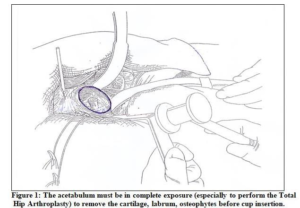 Figure 2 & 3. As a result, releasing the soft tissue around the hip is necessary for majority of cases. To decide the release procedures are justified or not, a test is proposed for practical usage.
Figure 2 & 3. As a result, releasing the soft tissue around the hip is necessary for majority of cases. To decide the release procedures are justified or not, a test is proposed for practical usage.


Test description
Objective of the test: to evaluate the mobility of trochanter over the acetabulum, if trochanter is mobile sufficiently, no need to release. The test performed during operation. After skin & fascia incision & removal of femoral head, let the hip completely free (no retractor, bone elevator, hook & other instruments in surgical field). Hip & Knee (of the operated limb) in neutral position (usually slightly flexed). Hold the trochanter by two hands, push it anteriorly (in poster lateral approach); push it posteriorly (in anterior approach). If the trochanter translates anteriorly (or posteriorly) less than half of acetabulum breathes: soft tissue release is justified. If trochanter translation is more than half of acetabulum breath: no need to release. Well balancing soft tissue around the hip, a functional artificial joint is achieved, not too tight, neither too loose. Figure 4 & 5.
Discussion
In the Hip Replacement Surgery (hemi or total arthroplasty), very important is to get an artificial joint not too tight, neither too loose [1, 2, 7]. Too tight joint risks of being difficult or impossible to relocate and / or dislocate during operation. Postoperatively, the hip will be not mobile enough, whose range of motion is limited. Inside the artificial joint, the constraints between head and polyethylene cup ( in total hip joint) or between head and true acetabulum of patient (in hemiarthroplasty ) remarkablely high result in rapide wear of the cup, or deterioration of acetabular cartilage and bone [3, 10].Then the survivorship of artificial joint will be not as long as expectation [4]. Whereas, a loose artificial hip joint risks of being easily dislocated. Postoperative dislocation of the artificial hip joint is a severe complication which requires in many cases reoperations, and in some cases patient must accept disability [4, 5, 6]. So not too tight, neither too loose is the golden standard of artificial hip joint [1, 2].
Most hips which are candidates for arthroplasty are stiff because the surrounding structures (capsule, synovia, ligaments, tendons & muscles etc.) for long time in chronic inflammatory processes. So, releasing the soft tissue around the hip is necessary for majority of cases. However, release is not justified for all patients. If too much releasing, the hip becomes too loose, result in easiness to be postoperatively dislocated [8, 9]. To help surgeon to decide what hip needs liberation surgery, the test as above description is proposed for practical application. Right indication for releasing the surrounding structures of hip, with well balancing the soft tissue, surgeon can get a functional artificial hip joint which is not too tight neither too loose, the golden standard of hip arthroplasty.
Conclusion
The hip arthroplasty (hemi or total) evaluated good or excellent if it is mobile smoothly (not too tight) and not easy to dislocate (not too loose). Hip disorders which deteriorated to the extent of needing the artificial joints are in majority of cases in the condition of contractures for which the surgery of releasing the soft tissue around hip is justified. The test to evaluate the mobility of trochanter over the acetabulum enables the surgeon to decide whether the liberation surgery is correctly indicated. The test should be used for all cases of hip arthroplasty for well balancing the soft tissue and consequently a functional artificial hip joint achieved.
Funding: No funding or grant support was received for this work.
Conflict of Interest: No financial disclosures
References
- Calandrucio RA (1987) Campbell’s Operative Orthopaedics. The C.V.Mosby Company 7th edition 1213-1501.
- Charnley J (1961) Arthroplasty of the hip: a new operation. Lancet 277:1129-1132.
- Charnley J, Halley DK (1975) Rate of wear in total hip replacement. Clin Orthop 112:170-179.
- Dobbs HS (1980) survivorship of total hip replacement. JBJ Surg 62-B:168-173.
- Dunn HK, Hess WE (1976) Total hip reconstruction in chronically dislocated hip. JBJ Surg 58:838-845.
- Etienne A, Cubic Z, Charnley J (1978) Postoperative dislocation after Charnley low-friction arthroplasty. Clin Orthop 132:19-23.
- Giliberty RP, et al (1978) A retrospective study of the bipolar hip endoprosthesis. Orthop Rev 7:27-31.
- Heppenstall RB (1978) Dislocation following total hip replacement. Orthop Trans. 2: 237.
- Lewinnek GE, et al (1978) Dislocation after total hip arthroplasty. JBJ Surg 60A: 217.
- Rose RM, Radin EL (1982) Wear of polyethylene in the total hip prosthesis. Clin Orthop 170:107.
- Volz RG, Wilson RJ (1977) Factors affecting the mechnical stability of the cemented acetabular component in total hip replacement JBJ Surg. 59-A 501.