Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Assessment of Jump Type and Leg Dominance on Time to Stabilization (TTS) for Division III Collegiate Athletes: An Exploratory Study
Andrew S. Bartlett1*, Brittney Mazzone2
1Nazareth College of Rochester, 4245 East Avenue Rochester, NY 14618-3790, USA
2San Diego State University, 5500 Campanile Dr, San Diego, CA 92182, USA
Received Date: January 15, 2022; Accepted Date: February 02, 2022; Published Date: February 10, 2022
*Corresponding author: Andrew S. Bartlett, Nazareth College of Rochester, 4245 East Avenue Rochester, NY 14618-3790, USA. Email: abartle1@naz.edu
Citation: Bartlett AS, Mazzone B (2022) Assessment of Jump Type and Leg Dominance on Time to Stabilization (TTS) for Division III Collegiate Athletes: An Exploratory Study. Adv Ortho and Sprts Med: AOASM-159.
DOI: 10.37722/AOASM.2022011
Abstract
Objectives: To assess time to stabilization (TTS) on jump type and leg dominance in Division III collegiate athletes.
Design: Exploratory study.
Setting: Division III College.
Participants: 21 NCAA Division III collegiate athletes competing in soccer, basketball, lacrosse, volleyball, and basketball.
Main Outcome Measure: TTS was calculated as the time from landing to when the vertical ground reaction force remained ±5% of each individual’s body weight following a dynamic jump protocol. A single force plate to capture four conditions (1) forward, dominant limb, (2) forward, non-dominant limb, (3) lateral, dominant limb, (4) lateral, non-dominant limb.
Results: Twenty-one participants (female=81%; age (mean ± SD) = 19.8 ± 1.2 years. TTS (mean ± SD): forward dominant leg = 0.88 ± 0.27 seconds; forward non-dominant leg = 0.86 ± 0.27 seconds; lateral dominant leg 1.04 ± 0.30 seconds; lateral non-dominant leg= 1.0 ± 0.36 seconds. The main effect of jump direction showed a statistically significant difference between forward and lateral jump (p = 0.01). Leg dominance did not show a statistically significant difference between dominant versus non-dominant leg (p = 0.63). There was not a statistically significant interaction between jump direction and leg dominance (p = 0.89).
Conclusion: Following a dynamic jump protocol, Division III athletes demonstrated worse dynamic postural stability in the lateral direction, as compared to the forward direction. Leg dominance did not have an influence on dynamic postural stability in either the forward or lateral direction, suggesting that one leg may not be more prone to injury.
Ethical statement: All participants consented to participate in this research study, which was approved by the Nazareth College Human Subjects Review Committee.
Highlights
- Time to stabilization (TTS) is an objective measure of dynamic postural stability.
- In Division III athletes, TTS is worse during lateral maneuvers than forward.
- Limb dominance does not influence TTS during forward and lateral jump protocols.
Keywords: Dynamic postural stability, Time to stabilization, Athletes, Injury
Introduction
Approximately 100,000 anterior cruciate ligament (ACL) ruptures occur annually in collegiate sports each academic year [1], with lifetime societal costs within the United States approximating to $38,000 per individual, including the cost of surgery, rehabilitation, and lost time from work [2]. Noncontact sports, such as running, skiing, and dance, have the lowest incidence rate of ACL injury (0.25/10,000 athlete exposures [AE]); whereas fixed-object high impact rotational landing sports, such as gymnastics, and contact sports, including basketball and soccer, have the highest incidence rates of ACL injuries (2.62/10,000 AEs, 1.51/10,000 AEs; respectively) [3]. Most ACL injuries (70%) occur from a noncontact mechanism such as landing from a jump [1, 4]. Complications resulting from an ACL injury may include, but are not limited to, disability, functional limitations, meniscal damage, and posttraumatic osteoarthritis [5-7]. Despite possible improvements from surgical ACL reconstruction, there is a high risk of posttraumatic degenerative joint disease and a decrease in functional outcomes [6, 8].
Numerous risk factors for ACL injuries have been identified including anatomic, genetic, hormonal, occupational, biomechanics, and neuromuscular abnormalities [9]. More specifically, increased frontal plane loads at the knee [10] and dynamic knee valgus collapse during cutting or one-legged jump landings have been identified as risk factors for noncontact ACL injuries [11, 12]. Neuromuscular factors such as decreased strength in core, hip abductors, hamstrings, are also considered risk factors for ACL injuries [4]. Impaired neuromuscular control at the knee is responsible for functional deficits including decreased strength, extended reaction times of the quadriceps and hamstrings, and decreased static and dynamic postural stability [13]. Individuals who have sustained an ACL injury demonstrate decreased static and dynamic postural stability [14-18]. However, static postural stability measures have been reported as insensitive and less functional, whereas dynamic postural stability tests are recommended [19, 20], as they more closely resemble athletic performance and the dynamic movements (landing, cutting, or deceleration) related to ACL injuries [14].
Landing from a jump requires dynamic postural stability, an ability to maintain a static state over an individual’s base of support following a dynamic movement [21]. Moreover, an increase in neuromuscular control is needed to maintain dynamic stability and has been recommended for ACL preventative programs [4, 21, 22]. There has been recent focus on time to stabilization (TTS) to assess dynamic postural stability [23-27]. TTS is a quantitative measure of dynamic postural stability used to assess an individual’s ability to transition from dynamic movements to static equilibrium inside their base of support [28]. Impaired dynamic postural stability, as demonstrated by slower TTS, has been demonstrated in individuals with ankle instability [27, 29], recreational athletes with a history of concussion (Lynall et al., 2020), and collegiate athletes post ACL reconstruction [8, 25, 26]. However, limited research has been conducted using TTS to assess the risk of a first time ACL injury [23].
DuPrey et al.(2016) [23] demonstrated that the TTS was significantly slower for a backward jump in Division I athletes who suffered an ACL injury compared to those without a history of an injury, suggesting that pre-injury TTS may be a risk factor for noncontact ACL injuries. Understanding TTS in collegiate athletes without a history of an ACL injury may help in the design of a clinically relevant screening tool aimed toward injury prevention. Furthermore, expanding on previous research by examining pre-injury TTS in Division III athletes, which to the best of our knowledge has not been examined, may provide further evidence on the significance of using dynamic postural training within a prevention program. The overall aim of this study was to evaluate pre-injury dynamic postural stability, as measured by TTS, in Division III collegiate athletes using a multiplanar jump protocol. Secondarily, we evaluated differences in dynamic postural stability by leg dominance.
Materials and Methods
This was an exploratory study. All participants provided their signed informed consent prior to participation and the study was approved by the college’s Human Subjects Review Committee. Between May 2018 and March 2019, participants from both women’s and men have selected NCAA Division III collegiate sports teams were recruited by sending a flyer to the coaches describing the purpose of the study. Selected teams included: lacrosse, soccer, basketball, and volleyball since these sports have shown to have a high rate of ACL injuries among their athletes [3]. Coaches from these teams described the purpose of the study and informed any athletes that were interested to contact the principal investigator of this study. Additionally, an email was sent to all athletes within these sports describing the study and informing them to contact the principal investigator for any further questions or to enroll. Interested and potential participants were preliminary screened by the principal investigator to ensure inclusion and exclusion criteria were met. Inclusion criteria included being either a freshman, sophomore, or junior Division III athlete in lacrosse, soccer, basketball, or volleyball. Senior athletes were not included in the study as they would no longer be participating in collegiate sports during the planned one-year follow up, which will not be reported in this analysis. Participants were excluded from the study if they had an existing neurological condition, diagnosis of chronic ankle instability, previous ankle fracture within six months of recruitment, or any knee ligament or meniscal injury within two years of recruitment. Of the 22 participants screened, all 22 met the inclusion criteria (17 women, 5 men). Height, weight, and leg length (anterior inferior iliac spine to the ipsilateral malleoli) were recorded by a single examiner.
Self-Reported Outcomes
After signing an informed consent form, participants completed an intake screening including the International Knee Documentation Committee Short Form (IKDC) [30]. The IKDC is a self-reported measure of knee function for several knee injuries including patellofemoral pain, osteoarthritis, and ligamentous and meniscal injuries [31]. The form consists of 10 questions divided into three categories: symptoms, sports activities, and knee function. Item responses are on a Likert Scale (0-10), with a maximum total score of 100 points. Higher numbers represent a higher level of function [32]. The IKDC is valid (construct validity r=.51, p< 0.0001) and reliable (internal consistency=0.88) [30].
Jump Testing Protocol
Prior to jump testing, participants completed a 10-minute warm-up, which has been recommended elsewhere [29, 33]. The warm-up consisted of five minutes on a stationary bike on low resistance and five minutes of dynamic lower extremity exercises. Following the warm-up, participants were provided a five-minute rest to minimize fatigue. A multidirectional, single legged jump protocol was used to assess dynamic postural stability, as previously used in other studies [24]. Participants performed a step, step, hop jump landing where they took two comfortable steps prior to jumping over a 15 cm hurdle with their test leg and landing in the middle of the force platform on their test leg (Figure 1A). Lateral jumps required the participant to shuffle two steps then hop with the leg closest to the force platform over the 5 cm hurdle and land single legged with the test leg in the middle of the force platform (Figure 1B).
Participants were provided a demonstration for each jumping direction by a single examiner and were allowed five practice trials for each jump, in order to become familiar with the testing procedure. Following the practice jumping trials, a random generator was used to determine the order of the jumps (direction [forward/lateral] and leg dominance [dominant/non-dominant) and to minimize a learning effect. Leg dominance was determined by participants self-reporting their dominant leg while participating in their sporting event. Each directional jump (forward/lateral) was completed for both the dominant and the non-dominant lower extremity for three successful trials, totaling 12 jumps. Participants were provided with a two-minute rest between jump trials to minimize fatigue [34]. Participants were instructed to land single legged in the middle of the force plate with their eyes forward, both hands on their hips, and an attempt to maintain motionless (stabilize) for five seconds. Jumps were discarded for any of the following reasons: did not use proper step protocol, did not land or take off on the correct side, did not land fully on the force plate, took double hops on the force plate, touched opposite foot to the force plate prior to the five-second stabilization period, stepped off the force plate prior to the five-second stabilization period, did not clear hurdle, excessive use of arms to maintain balance. All landings were on a single force plate (Bertec Corporation, Columbus, OH). Kinetic data were collected for a five-second duration at a sampling rate of 100 Hz. Participants performed each jump barefoot to avoid stability assistance from their shoes [29].

Figure 1: Jump Testing Protocol. (A.) Forward Jump, (B.) Lateral Jump.
Caption: Black indicates test limb. Arrow indicates direction the person is facing. Numbers are the order of steps, with [1] indicating the start. (A.) [1] Participant starts with both feet together, [2] 1 step with non-test limb, [3] 1 step with test limb, [4] test limb performs hop over 15 cm box landing in a single legged stance on the force plate. (B.) [1]Participant starts with both feet together, [2] participant takes a shuffling step with test limb, [3] participant takes a shuffling step with non-test limb to bring feet together, [4] participant takes shuffling step with test limb [5] participant hops over 5 cm hurdle with test limb landing in a single legged stance on the force plate.
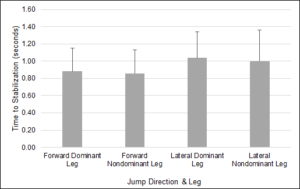
Figure 2: Time to Stabilization.
Dynamic Postural Control Measurement
TTS was used to assess dynamic postural control [25, 26, 27] and was quantified based on previous methodology [35]. Specifically, TTS is equal to the time the vertical ground reaction force (GRF) reaches and stays within ±5% of the participants body weight after landing on a force plate [23, 35]. Increased TTS (slower time to stabilize) represents decreased or worse dynamic postural controland has shown to be reliable during landing activities (ICC=.65-.79) [19].
Statistical Analysis
Statistics were calculated using IBM SPSS 2017 Version 25. Descriptive statistics were used to describe the sample (age, body mass index [BMI], IKDC score, and sport). A two-way repeated measures ANOVA was utilized to determine the effect of jump type (forward and lateral) and leg dominance (dominant and non-dominant). The normality of distributions and outliers were verified using the Shapiro-Wilk and studentized test respectively. Additionally, main effects of the two within- subjects’ factors were examined. Descriptive analysis of means and standard deviations were performed to characterize the sample, jump type, and leg (dominant/non-dominant). The level of significance was set at p<0.05 for all tests.
Results
Twenty-one Division III participants had complete outcome data and were included in the analysis. One participant was missing multiple TTS data on both the forward and lateral jumps, thus was excluded from data analysis. Participants were, on average, 19.8 ± 1.2 years old with a BMI of 24.4 ± 3.7 kg/m2; 81% were women. Average IKDC score was 96.7 ± 5.8 points out of 100 points (Table 1). Participants were from four different sports: lacrosse (n=9), soccer (n=6), volleyball (n=2), basketball (n=4) (Table 2). The mean ± standard deviation (SD) for TTS for the four different type of jumps were forward with dominant leg (0.88 ± 0.27 seconds); forward with non-dominant leg (0.86 ± 0.27 seconds); lateral with dominant leg (1.04 ± 0.30 seconds); lateral with non-dominant leg (1.0 ± 0.36 seconds) (Figure 2).
Table 1
Female (n=17)
Males (n=4)
Age (years)
19.7 ± 1.2
20.0 ± 1.0
International Knee Documentation Committee Short Form (points)
96.4 ± 6.2
98.9 ± 1.6
Body Mass Index (kg/m2)
24.3 ± 3.88
24.8 ± 2.77
Participant characteristics (mean ± 1 standard deviation)
Sport type by gender (n)
Female (n=17)
Males (n=4)
Lacrosse
9
Soccer
5
1
Volleyball
2
Basketball
1
3
Analysis of the studentized residuals showed that the data was minimally skewed, as assessed by the Shapiro-Wilk test of normality and no outliers, as assessed by no studentized residuals greater than ±3 standard deviations. The main effect of jump type showed a statistically significant difference between forward and lateral jumps, F(1,20)=6.83, p=.01. The main effect of leg dominance did not show a statistically significant difference between dominant vs. non-dominant leg, F(1,20)=0.247, p= 0.63. There was not a statistically significant interaction between jump type and leg dominance F(1,20)= 0.019, p= 0.89.
Discussion
When using a dynamic jumping protocol [23, 24], healthy Division III collegiate athletes took a statistically longer time to stabilize single-legged after performing a lateral jump as compared to a forward jump. Our results support that landing from a medial to lateral direction is more challenging; more closely resembles an athletic movement, and requires both frontal and transverse plane neuromuscular control [36]. This is clinically important considering injuries are more likely to result from a medial-lateral component in a landing [11, 44]. Our results are similar to [24] who also found that, a lateral jump type had significantly longer TTS than a frontal jump type in healthy active participants (non-athletes). Similarly, although not statistically significant, DuPrey et al.(2016) [23] reported slower TTS in lateral jump landings as compared to forward jump landings in Division I athletes who sustained an ACL injury over a 4-year period compared to athletes who did not sustain an ACL injury. Furthermore, using a drop landing protocol, a slower TTS has been reported in the medial-lateral direction as compared to the frontal direction [37]. In contrast to our findings, Liu et al.(2016) did not find any significant difference in TTS when comparing forward and lateral hops in Division I collegiate athletes with either healthy, coping with unstable ankles, or unstable ankles.
There are several possible reasons for why our results indicated a significant difference in TTS related to jump type as compared to other studies [23, 27, 29]. but not all (Liu & Heise, 2013) [24]. One reason may be a variation in the jump protocol. In contrast to studies which required patients to take “two comfortable steps” when performing a lateral directional jump [23, 24], include a vertical component in their jump protocol (Liu et al., 2016), or perform a single-legged drop jump [27], we had our participants assume an athletic stance and shuffle two steps prior to jumping in the lateral direction off either their dominant or non-dominant leg. The intent of this variation was to replicate a movement used in athletic competition. The resulting increased speed used prior to performing a lateral jump as compared to a forward jump may account for the significant difference in TTS. Best to our knowledge, the impact of speed in performing a jump protocol and its relation to TTS has not been researched. An additional factor in the differing study results is not all studies [23, 24, 27, 41] officially screened for impaired knee function, which has been shown to effect dynamic postural stability [13]. Similar to others, we used the IKDC to help ensure knee function was not impaired [26].
In utilizing a similar dynamic jump protocol for healthy collegiate athletes, mean values for TTS for both forward and lateral jump directions were similar to others [23, 24]. However, when utilizing a different jump protocol, differences exist for average TTS in both forward and lateral jump directions [26, 29]. Furthermore, differences exist in the literature in regards to calculating TTS [19, 34]. This may suggest that when using the same jumping protocol, calculations of TTS normative data could be compiled to help better understand athletes’ TTS. Thus, jumping protocols should be standardized to compare results across studies. This could be clinically significant when performing initial screening as correlations exist between TTS and ACL risk [23]. Moreover, in cases where an athlete sustains an ACL injury, TTS normative data may play a crucial role in the athlete’s return to sport and decrease the prevalent risk of reinjury.
Results from our study also demonstrated no significant difference in TTS between participants’ dominant and non-dominant legs. These results indicate that self-reported leg dominance did not affect participants’ ability to stabilize on a single limb after performing a dynamic jumping protocol. Our research concurs with others who reported no bilateral differences on dynamic postural stability [33, 34. In contrast to other studies that utilized alternative forms of jump landing protocols, the results of this study adds to the limited literature on TTS and leg dominance by reporting no differences in TTS and leg preference following a dynamic jump protocol in Division III athletes [39, 40]. The lack of significant findings related to leg dominance may be due to the heterogeneity of sport type. Our study included athletes who played lacrosse, volleyball, and basketball, which are primarily upper extremity focused, and soccer, which is primarily lower extremity focused. It is possible that lacrosse, volleyball, and basketball players may be ambidextrous in leg dominance, whereas soccer plays may have a distinct dominant side.
Limitations
Participants in our study had healthy knees as determined by a mean IKDC score of 96.7 ± 5.8 points. These results are similar to Patterson et al. (2013) [26] who reported a mean IKDC score of 99.1 ± 3.7 points in healthy control participants. However, because the IKDC is a self-reported measure, it is plausible that our participants may have had impaired knee function. Moreover, impaired dynamic postural stability, as demonstrated by slower TTS, has been demonstrated in individuals with ankle instability [27, 29]. We aimed to exclude participants with previous ankle impairments by identifying diagnoses of chronic ankle instability or previous ankle fractures within six months of recruitment. As this was also self-reported it is conceivable that participants had ankle instability which could have affected their TTS. Assessing knee and ankle stability in our participants could have helped alleviate these limitations; however, conscious of the participants’ time, we chose to have them self-report as they were balancing both academics and athletics at the time of the study. Additionally, not formally assessing knee and/or ankle stability is consistent with previous studies [23, 24, 26].
Opportunities for Future Research
Future research should utilize a standardized jumping protocol to be able to compare TTS across articles and populations. Moreover, normative data can be compiled and utilized for prevention and return to sport programs. This would be clinically significant since there has been an increase in ACL injuries despite prevention programs [41-44]. Additionally, TTS as it relates to different sports at the collegiate level (Division I, II, and III) should be researched to determine if differences exist. This information will further our understanding and possible utilization of TTS in prevention and return to sport programs. Lastly, future research should have a follow-up component to determine if slower TTS is related to lower extremity injuries such as ACL injuries, as described in DuPrey et al (2016) [23].
Conclusions
Poor dynamic postural stability is a known risk factor for ACL injuries in athletes [14-18]. TTS, a measure of dynamic stability, a fairly simple measure that could be implemented as a screen tool and part of an ACL prevention plan or return to sport program. Following a dynamic jump protocol, Division III athletes demonstrated worse dynamic postural stability in the lateral direction, as compared to the forward direction. Leg dominance did not have an influence on dynamic postural stability in either the forward or lateral direction, suggesting that one leg may not be more prone to injury. To the best to our knowledge, this is the first study examining TTS in Division III athletes. There was no difference in TTS related to leg dominance.
Appendix
- TTS- Forward and Lateral Jumps for Dominant and Non-Dominant Legs
- TTS = Time to Stabilization; M= male; F= female.
Participant ID
Sex
Sport
TTS (seconds)
Forward
Lateral
Dominant Leg
Non-Dominant Leg
Dominant Leg
Non-Dominant Leg
1
F
Soccer
1.18
1.1
1.07
1
2
F
Soccer
0.81
0.93
0.93
0.78
3
F
Soccer
0.88
0.63
1.19
1.09
4
F
Volleyball
0.65
0.67
0.94
0.75
5
F
Lacrosse
0.71
0.64
1.1
1.51
6
M
Basketball
0.91
1.41
0.86
0.49
7
M
Soccer
0.71
0.96
0.87
1.35
8
F
Lacrosse
1.22
0.98
1.96
1.14
9
F
Volleyball
1.12
0.72
1.1
1.16
10
F
Soccer
0.68
0.53
0.61
0.55
11
F
Soccer
0.91
0.82
1.04
1.07
12
M
Basketball
0.53
0.74
1.39
1.1
13
M
Basketball
1.03
1.58
1.02
2.04
14
F
Lacrosse
0.68
0.85
0.94
0.77
15
F
Lacrosse
0.87
0.61
1.36
0.68
16
F
Lacrosse
0.67
0.94
0.82
0.99
17
F
Lacrosse
0.65
0.58
0.86
0.68
18
F
Lacrosse
0.83
0.92
0.61
0.75
19
F
Lacrosse
0.94
0.71
1.02
1.18
20
F
Lacrosse
0.81
0.62
0.66
0.69
21
F
Basketball
1.06
1.76
1.26
1.47
Conflict of Interest: The authors certify they have no affiliations with or financial involvement with any organization or entity with a direct financial interest in the subject matter or materials discussed in this article.
Declaration of interest: The authors declare there are no conflicts of interest.
Ethical approval: The study protocol was approved by the human subjects committee at Nazareth College. Before data collection, all participants reviewed and signed an informed consent.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data Availability Statement: The authors confirm that all subject summary data is provided in the supplemental material.
References
- Dragoo JL, Braun HJ, Durham JL, Chen MR, Harris AH (2012) Incidence and risk factors for injuries to the anterior cruciate ligament in national collegiate athletic association football: Data from the 2004-2005 through 2008-2009 national collegiate athletic association injury surveillance system. American Journal of Sports Medicine 40: 990-995.
- Mather RC, Koenig L, Kocher MS, Dall TM, Gallo P, et al. (2013) Societal and economic impact of anterior cruciate ligament tears. Journal of Bone and Joint Surgery 5: 1751-1759.
- Montalvo AM, Schneider DK, Webster KE, Yut L, Galloway MT, et al. (2019) Anterior cruciate ligament injury risk in sport: A systematic review and meta-analysis of injury incidence by sex and sport classification. Journal of Athletic Training 54: 472-482.
- Pfeifer CE, Beattie PF, Sacko RS, Hand A (2018) Risk factors associated with non-contact anterior cruciate ligament injury: A systematic review. International Journal of Sports Physical Therapy 13: 575-585.
- Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis & Rheumatology 50: 3145-3152.
- Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, et al. (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: A prospective study with 10 to 15 years of follow-up. American Journal of Sports Medicine 38: 2201-2210.
- Whittaker JL, Woodhouse LJ, Nettel-Aguirre A, Emery CA (2015) Outcomes associated with early post-traumatic osteoarthritis and other negative health consequences 3-10 years following knee joint injury in youth sport. Osteoarthritis and Cartilage 23: 1122-1129.
- Webster KA, Gribble PA (2010) Time to stabilization of anterior cruciate ligament-reconstructed versus healthy knees in national collegiate athletic association division i female athletes. Journal of Athletic Training 45: 580-585.
- Smith HC, Vacek P, Johnson RJ, Slauterbeck JR, Hashemi J, Shultz S, Beynnon BD (2012) Risk factors for anterior cruciate ligament injury: A review of the literature-part 2: Hormonal, genetic, cognitive function, previous injury, and extrinsic risk factors. Sports Health 4: 155-161.
- Hewett TE, Myer GD, Ford KR, Heidt RS, Colosimo AJ, et al. (2005) Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. American Journal of Sports Medicine 33: 492-501.
- Koga H, Nakamae A, Shima Y, Iwasa J, Myklebust G, et al. (2010) Mechanisms for noncontact anterior cruciate ligament injuries: Knee joint kinematics in 10 injury situations from female team handball and basketball. American Journal of Sports Medicine 38: 2218-2225.
- Sugimoto D, Alentorn-Geli E, Mendiguchia J, Samuelsson K, Karlsson J, (2015) Biomechanical and neuromuscular characteristics of male athletes: Implications for the development of anterior cruciate ligament injury prevention programs. Sports Medicine 45: 809-822.
- Zech A, Hubscher M, Vogt L, Banzer W, Hansel F, Pfeifer K (2009) Neuromuscular training for rehabilitation of sports injuries: A systematic review. Medicine & Science in Sports & Exercise 41: 1831-1841.
- Heinert B, Willett K, Kernozek TW (2018) Influence of anterior cruciate ligament reconstruction on dynamic postural control. International Journal of Sports Physical Therapy 13: 432-440.
- Hurd WJ, Axe MJ, Snyder-Mackler L (2008) Influence of age, gender, and injury mechanism on the development of dynamic knee stability after acute acl rupture. Journal of Orthopaedic & Sports Physical Therapy 38: 36-41.
- Lee JH, Han SB, Park JH, Choi JH, Suh DK, Jang KM (2019) Impaired neuromuscular control up to postoperative 1 year in operated and nonoperated knees after anterior cruciate ligament reconstruction. Medicine 98: e15124.
- Lee JH, Lee DH, Park JH, Suh DW, Kim E, et al. (2020) Poorer dynamic postural stability in patients with anterior cruciate ligament rupture combined with lateral meniscus tear than in those with medial meniscus tear. Knee Surgery & Related Research 32: 8.
- Staples JR, Schafer KA, Smith MV, Motley J, Halstead M, et al. (2020) Decreased postural control in patients undergoing anterior cruciate ligament reconstruction compared to healthy controls. Journal of Sport Rehabilitation 29: 920-925.
- Ross SE, Guskiewicz KM, Yu B (2005) Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. Journal of Athletic Training 40: 298-304.
- Sell TC (2012) An examination, correlation, and comparison of static and dynamic measures of postural stability in healthy, physically active adults. Physical Therapy in Sport 13: 80-86.
- Colby SM, Hintermeister RA, Torry MR, Steadman JR (1999) Lower limb stability with acl impairment. Journal of Orthopaedic & Sports Physical Therapy 29: 444-451.
- Sadoghi P, von Keudell A, Vavken P (2012) Effectiveness of anterior cruciate ligament injury prevention training programs. Journal of Bone and Joint Surgery 94: 769-776.
- DuPrey KM, Liu K, Cronholm PF, Reisman AS, Collina SJ, et al. (2016) Baseline time to stabilization identifies anterior cruciate ligament rupture risk in collegiate athletes. American Journal of Sports Medicine 44: 1487-1491.
- Liu K, Heise GD (2013) The effect of jump-landing directions on dynamic stability. Journal of Applied Biomechanics 29: 634-638.
- Niemeyer P, Niederer D, Giesche F, Janko M, Frank J, et al. (2019) Unanticipated jump-landing after anterior cruciate ligament reconstruction: Does unanticipated jump-landing testing deliver additional return to sport information to traditional jump performance tests? Clinical Biomechanics 70: 72-79.
- Patterson MR, Delahunt E (2013) A diagonal landing task to assess dynamic postural stability in acl reconstructed females. Knee 20: 532-536.
- Wright CJ, Arnold BL, Ross SE (2016) Altered kinematics and time to stabilization during drop-jump landings in individuals with or without functional ankle instability. Journal of Athletic Training 51: 5-15.
- Hirokawa S, Solomonow M, Luo Z, Lu Y, D’Ambrosia R (1991) Muscular co-contraction and control of knee stability. Journal of Electromyography and Kinesiology 1: 199-208.
- Liu K, Dierkes C, Blair L (2016) A new jump-landing protocol identifies differences in healthy, coper, and unstable ankles in collegiate athletes. Sports Biomechanics 15: 245-254.
- Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, et al. (2007) Reliability and validity of the international knee documentation committee (ikdc) subjective knee form. Joint Bone Spine 74: 594-599.
- Irrgang JJ, Anderson AF (2002) Development and validation of health-related quality of life measures for the knee. Clinical Orthopaedics and Related Research (402), 95-109.
- Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyre P, et al. (2006). Responsiveness of the international knee documentation committee subjective knee form. American Journal of Sports Medicine, 34: 1567-1573.
- Clarke F, Koutedakis Y, Wilson M, Wyon M (2020) Bilateral differences in dancers’ dynamic postural stability during jump landings. Journal of Dance Medicine & Science 24: 183-189.
- Wikstrom EA, Tillman MD, Smith AN, Borsa PA (2005) A new force-plate technology measure of dynamic postural stability: The dynamic postural stability index. Journal of Athletic Training 40: 305-309.
- McKinley P, Pedotti A (1992) Motor strategies in landing from a jump: The role of skill in task execution. Experimental Brain Research 90: 427-440.
- Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh, JH, Borsa PA (2007) Dynamic postural stability deficits in subjects with self-reported ankle instability. Medicine & Science in Sports & Exercise 39: 397-402.
- Krkeljas Z (2018) Comparison of jump-landing protocols with biodex balance system as measures of dynamic postural stability in athletes. Sports Biomechanics 17: 371-382.
- Lynall RC, Campbell KR, Mauntel TC, Blackburn JT, Mihalik JP (2020) Single-legged hop and single-legged squat balance performance in recreational athletes with a history of concussion. Journal of Athletic Training 55: 488-493.
- Boo HC, Howe TS, Koh JS (2020) Effect of leg dominance on early functional outcomes and return to sports after anterior cruciate ligament reconstruction. Journal of Orthopaedic Surgery 2: 2309499019896232.
- Mokhtarzadeh H, Ewing K, Janssen I, Yeow CH, Brown N, et al. (2017) The effect of leg dominance and landing height on acl loading among female athletes. J Biomech 60: 181-187.
- Ajuied A, Wong F, Smith C, Norris M, Earnshaw P, at el. (2014). Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: A systematic review and meta-analysis. American Journal of Sports Medicine 42: 2242-2252.
- Padua DA, DiStefano LJ, Hewett TE, Garrett WE, Marshall SW, et al. (2018) National athletic trainers’ association position statement: Prevention of anterior cruciate ligament injury. Journal of Athletic Training 53: 5-19.
- Quatman CE, Quatman-Yates CC, Hewett TE (2010) A ‘plane’ explanation of anterior cruciate ligament injury mechanisms: A systematic review. Sports Medicine 40: 729-746.
- Wikstrom EA, Tillman MD, Kline KJ, Borsa PA (2006) Gender and limb differences in dynamic postural stability during landing. Clinical Journal of Sport Medicine 16: 311-315.