Publication Information
ISSN: 2688-0873
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Archives |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Combined Approach for Incarcerated Intraparietal Spiegel Hernia
– A Safer Way to Do It
Sorin Cimpean*, Ion Surdeanu, Isaline Shumacker, Jordan Marcelis, Abdelilah Mehdi
Digestive Surgery Department, Saint Pierre University Hospital, Brussels, Belgium
Received Date: January 11, 2022; Accepted Date: January 19, 2022; Published Date: January 24, 2022
*Corresponding author: Sorin Cimpean, Iris Hospitals South, Brussels, Belgium. Email: sorin.campean_md@yahoo.com
Citation: Cimpean S, Surdeanu I, Shumacker I, Marcelis J, Mehdi A (2022) Combined Approach for Incarcerated Intraparietal Spiegel Hernia – A Safer Way to Do It. Jr Surg Opetech Anesthesia: JSOPA-115.
DOI: 10.37722/JSOTA.2022101
Abstract
Spiegel hernia is a rare type of parietal hernia with high risk of incarceration due to the small size of the hernia neck. The clinical diagnostic can be difficult especially when in interstitial hernia. In case of suspicion of incarceration an abdominal CT scan is the exam of choice. We present here a case of a intraparietal incarcerated Spiegel hernia. We propose for this type of hernia a combined laparoscopy/laparotomy approach.
Background
A Spiegel hernia is a rare hernia with a reported incidence of 0.12–2% of all abdominal wall hernias. The risk factors for the apparition of this type of hernia are the same with the parietal hernias as increased intraabdominalpressure from chronic conditions, congenital connective tissue disorders or acquired as in aging and smoking [1]. This hernia develop through a defect in the Spigelian fascia which is the part of the transversus abdominis aponeurosis lateral to the rectus muscle, often at the level of the arcuate line, where the fascia is widest and weakest [2]. We report a case of a patient who presented an incarcerated left Spiegel hernia with small bowel in the hernia sac. The approach was combined and consisted in exploratory laparoscopy followed by mini-laparotomy with small bowel liberation and parietal closure and laparoscopic mesh placement.
Case Presentation
A 49 years old patient presented at Emergency Unit with intense abdominal pain in the left side of the abdomen. The patient presented abdominal pain in this region in the last week with spontaneous resolution, but in the last 6 hours the pain increase in intensity. The bowel transit was present for the stools but not for gas. No vomiting was reported but the nausea was present at the moment of admission. The clinical exam found a distended abdomen with general sensibility but no signs of acute abdomen. In the left flank the sensibility was more important but no mass was palpable.
The medical history revealed an appendectomy by laparoscopy. At the admission the parameters were: Systolic blood pressure: 140 mmHg, Heart rate: 74 /min, T°: 37.0 °C, SaO2: 98 %. The laboratory count revealed WBC (white blood cells): 12.33 x10^3/μL(range between 4.00-10.00), CRP(C-reactive protein): 4.61 mg/L (range<5.00).
The abdominal CT scan revealed a mechanical occlusive syndrome on a Spiegel’s parietal hernia in the left iliac flank with incarceration of a small bowel loop. The incarcerated loop was placed in intraparietal (interstitial) position (Figure 1). A surgery in emergency surgery was indicated.
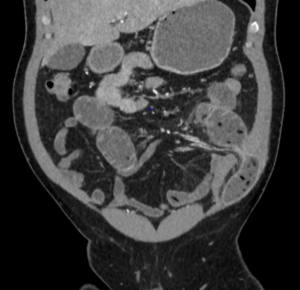
Figure 1: Spiegel’s parietal hernia with small bowel content and underlying occlusive syndrome.
Operative Technique
Due to the important size of the herniated loop and the long interstitial trajectory we decided to perform a combined laparotomy/laparoscopy approach. One trocar of 10mm was placed by open laparoscopy technique in the right flank and 2 trocars of 5 mm were placed in the right hypochondria and iliac fossa. The position of the hernia neck was established and a 5 cm laparotomy at the level of the hernia was performed (Figure 2, 3). The bowel presented multiple intra-saccular adhesions. A liberation of the adhesions was performed and the completely liberated bowel loop was reintegrated into the abdomen. The parietal defect was closed in 2 plans. Under laparoscopy a dual mesh type was placed and secured with multiples resorbable tracks (Figure 4). The patient’s postoperative evolution was uneventful and the patient was discharged at the 3rd postoperative day with restored oral alimentation and intestinal transit.
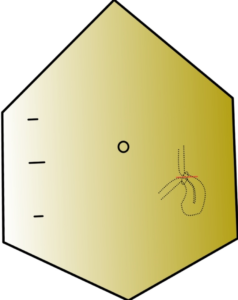
Figure 2: Trocars positioning and positioning of the mini-laparotomy incision.

Figure 3: Preoperative image with the mini-laparotomy.
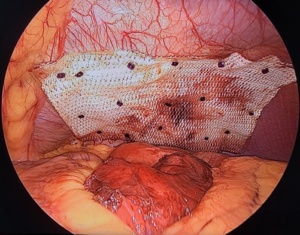
Figure 4: Laparoscopic image who reveals the mesh positioning.
Discussions
Spigelian hernias occur through a defect in the Spigelian fascia. This is the aponeurosis of the transverse abdominal muscle, and is found on the lateral border of the rectus abdominis muscle extending from the ninth costal cartilage to the public tubercle [3, 4]. This aponeurotic structure is comprised of the fusion of the transversus aponeurosis and the posterior leaf of the internal oblique aponeurosis [5]. Spiegel hernias characteristically contain narrow sac necks (0.5–2 cm) who predispose to incarceration once the small bowel, the colon or the omentum slides. The reported incidence of incarceration is between 24% – 27% and strangulation at 2% – 14%. (12, 5) 11.8 % of the patients with Spiegel hernia present simultaneously other types of parietal hernia [6]. The most common symptoms are pain and the presence of a mass. Only 50% of Spigelian hernias are diagnosed preoperatively by palpation. The clinical examination and the direct diagnostic are often difficult due to the presence of the abdominal fat and the external oblique aponeurosis [7]. There are two types of Spiegel hernia. The interparietal type hernia (interstitial, intramuscular, or intramural type) is situated below the external oblique aponeurosis and the sac is located between musculoaponeurotic layers of the anterior abdominal wall. The sac identification at the clinical examination can be challenging. The subcutaneous type of Spigelian hernia penetrates the external oblique aponeurosis and is easy to palpate at the clinical examination [8]. In term of imagery, the parietal ultrasonography is accessible and accurate in revealing the defects in the Spigelian fascia. The abdominal CT scan gives more complete information on the contents of the sac than ultrasound and allows a better characterisation of the intraabdominal content, especially when signs of peritoneal irritation are present. Still, false negative findings can occur in 32% of patients, due to the unusual disposition of this type of hernia [9]. In most of the cases this type of hernia is asymptomatic (nine out of ten cases), but the risk of strangulation is high, requiring systematic surgical treatment [10]. Different surgical approaches are described in the literature: by laparotomy, by raphy or pre-peritoneal or pre-fascial prosthetic plasty; laparoscopic, raphy or intraperitoneal, trans-abdomino-preperitoneal or extra-peritoneal prosthetic plasty [11, 12].
Justification of the Approach
We believe that this combined approach is safer in case if intraparietal Spiegel hernia, especially when an important bowel segment is incarcerated. The identification of hernia in case of obese patients or in case of interstitial herniamight not conclusive preoperatively by palpation. Laparoscopic approach allows the identification of the hernia neck and a complete exploration of the abdominal cavity. By laparoscopy the surgeon can check if the mobilisation of the herniated bowel can be performed with no risk of damaging the bowel. If this mobilisation is difficult, even after performing a kelotomy, due to the intrasaccular adhesions, a mini-laparotomy can be performed. This laparotomy is guided by the laparoscopic vision and can help significantly in mobilisation of the incarcerated bowel and decrease the risk of bowel lesions. The laparoscopy can help in minimise the size of the laparotomy and choose the best site for incision. Traction on the bowel during laparoscopy, especially in case of incarcerated, fragile bowel wall can increase the risk of bleeding from the meso vessels of iatrogenic perforation. Usually a bowel perforation in this context imposes a segmental resection that cannot be justified if the combined approach offers a safer solution. More, a perforation will limit the indications for intraabdominal of intraparietal mesh placement.
Conclusion
The diagnostic of an incarcerated interstitial Spiegel hernia needs a high index of suspicion. In case of incarceration, due to the small hernia neck and intrasaccular adhesions, the combined approach can minimise the risk of bowel injury and allows a convenient parietal closure with mesh reinforcement.
References
- Page D, Hendahewa R (2020) An incarcerated Spigelian hernia with the appendix in the sac passing though all layers of the abdominal wall: an unusual cause for chronic right iliac fossa pain. Journal of Surgical Case Reports 2020(6):rjaa099.
- Cesaro E, Rocco C, Rosano N, Ferrandino G, Marra E, et al. (2021) “Bulb-like” sign: Small bowel closed loop obstruction in incarcerated Spigelian hernia. Radiology Case Reports mars 16: 520‑523
- Ramones MT, Beech D (2010) Incarcerated Spigelian Hernia: A Rare Cause of Mechanical Small-Bowel Obstruction. Journal of the National Medical Association. août 102: 731‑733
- Lavin A, Gupta A, Lopez-Viego M, Buicko JL (2020) Incarcerated Spigelian Hernias: A Rare Cause of a High-grade Small Bowel Obstruction. Cureus 12: e7397.
- Leone PJ, Girotra M (2020) Incarcerated Spigelian Hernia. Clinical Gastroenterology and Hepatology. mars 18: e34.
- Bastidas JG, Khan AR, LeBlanc KA (2010) Spigelian Hernia as a Cause of Small Bowel Obstruction: Southern Medical Journal. juin 103: 567‑599
- Reinke C, Resnick A (2010) Incarcerated appendix in a Spigelian hernia. Journal of Surgical Case Reports. 2010(10): 3.
- Karadimos D, Kp J (2019) Laparoscopic mesh repair of an incarcerated Spigelian hernia causing small bowel obstruction. Aal of SurgerNZ Journy. 90. 10.1111/ans.15094.
- Azar SF, Jamadar DA, Wasnik AP, O’Rourke RW, Caoili EM, et al. (2021) MDCT imaging in Spigelian hernia, clinical, and surgical implications. Clinical Imaging 74: 131‑138.
- Anilir E, Buyuker F, Tosun S, Alimoglu O (2019) Incarcerated Spigelian hernia: A rare cause of abdominal wall tender mass. North Clin Istanb 7: 74-77.
- Zuvela M, Milicevic M, Galun D, Djuric-Stefanovic A, Bulajic P, et al. (2013) Spigelian hernia repair as a day-case procedure. Hernia. août 17: 483‑486
- Moszkowicz D, Paye F, Balladur P, Lefevre JH (2012) Une cause rare d’occlusion aiguë du grêle : la hernie de Spiegel étranglée. Description d’un cas et revue de la littérature. Morphologie 96: 12‑15.