Publication Information
ISSN 2691-8803
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2019
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
CNS Repair in a girl with a Spinal Cord Injury
Giselher Schalow*
(NGOR: Non-Government-Organized-Research), Switzerland
Received Date: January 26, 2021; Accepted Date: February 02, 2021; Published Date: February 11, 2021
*Corresponding author: Giselher Schalow, (NGOR: Non-Government-Organized-Research), Dr.med.habil. Dr.rer.nat. Dipl.Ing. Untere Kirchmatte 6, CH-6207 Nottwil, Switzerland. Email: g_schalow@hotmail.com
Citation: Schalow G (2021) CNS Repair in a girl with a Spinal Cord Injury. Adv Pub Health Com Trop Med: APCTM-121.
DOI:10.37722/APHCTM.2021101
(http://doi.org/10.37722/APHCTM.2021101)
Summary
By medical malpractice, the 5.5-years-old Nefeli suffered an incomplete spinal cord injury at Th10/11 levels. At an age of 9, through 4 years of Coordination Dynamics Therapy, she re-learned walking, running, jumping and became continent again. At an age of 14, an orthopedic surgeon made the family believe that the walking performance could substantially be improved by a leg operation. Against the strong advice of the Author ‘to avoid the operation’, because such operations in spinal cord injury reduce the plasticity, necessary for repair, the parents decided for the operation. Till 6 weeks after the operation, the patient could not move the legs anymore because of extreme flexor spasticity, rigor and cramps. 3.5 months after the operation, including 8 weeks of intensive Coordination Dynamics Therapy with the Author, she could move the legs a bit again, but could not walk freely.6 months after the operation, she became able to walk a bit with orthoses and after 8 months she re-learned to walk a bit without orthoses. Through the operation, the patient lost approximately 2 years of movement-based learning therapy. It will be analyzed in detail that the orthopedic surgeon operated without sufficient knowledge in human repair-neurophysiology, necessary especially in spinal cord injury. The operation-induced extreme flexor spasticity made the standing and upright movements impossible. Only the Author was able, through administering Coordination Dynamics Therapy, to slowly reduce the extreme flexor spasticity and to make the spinal cord injury patient Nefeli walk again.
Keywords: Coordination Dynamics Therapy; Electrophysiology; Human Repair-Neurophysiology; Oscillatory Firing; Phase and Frequency Coordination; Single-Nerve Fiber Action Potentials; Spinal Cord Injury Repair; Surface EMG
Introduction
It is known for something like 70 years that the plasticity of the nervous system is highest if no operation is performed in nervous system-injured patients. Especially in critical patients, like the Spinal Cord Injury (SCI) patient Nefeli, in whom only approximately 30% of the spinal cord was remained, operations are contra-indicated. A four-year CDT made her walking, running, jumping and continent [1]. Through movement-based learning, the Central Nervous System (CNS) just succeeded to generate everyday functions again. Because of the limited variability of the injured CNS (SCI), the movement performance was not optimal.
Through an operation of tendons and bones, the inputs, from the different receptors of the periphery to the CNS, will change and reduce. The achieved movement performance will be ruined. Only tremendous movement-based learning therapy for years could compensate for such an operation. But patients, who have trained already for years, are worn out to train further for years. Only few patients have the mental discipline to train at limits for years as Wilma Rudolf. She got poliomyelitis and could win gold medals in running in 1956.
Further, during puberty, patients with CNS injury loose functions due to the puberty-induced changes of the CNS. Only intensive therapy can compensate for these changes. Therefore, the timing of the operation was also wrong, because the patient Nefeli was already in the phase of puberty. The surgeon disregarded that the patient Nefeli had a critical incomplete SCI (approximately 30% of the cord were left) and was in the phase of puberty. He seemed not to know that CNS plasticity reduces with an operation.
But where is such miss-knowledge coming from? In patients with no CNS injury, the plasticity is enormous. Every operation-induced change in the periphery is compensated for, especially through movement-based learning, by the complexity of the CNS, mainly located in the brain. After an operation, in minutes to hours, the human brain learns to generate physiologic movements again. Poliomyelitis patients relearned in minutes, when tendons were transposed. Surprisingly few trials were required for poliomyelitis patients to use transposed tendons successfully [2]. Animals on the other hand have a less complex CNS with less variability and plasticity. Approximately 75 years ago, Sperry transposed the nerve supplies of flexor and extensor muscles in rats [3] and monkeys [4]: the monkey relearned the task after some time; the rat did not.
Nearly all patients with an SCI have different kinds of spasticity according to the injury. Due to the injury, the CNS is not able anymore to generate certain automatisms in a physiologic way. These patterns become pathologic and are called spasticity or spastic patterns. Of interest here are especially the extensor and the flexor spasticity of the legs. The extensor spasticity seems to originate from the anti-gravity muscle activation pattern and the flexor spasticity of the legs from the protection automatisms.
When stepping on a sharp stone, the leg is lifted automatically to protect the foot against injury. The protection automatism of hand and fingers is well-known. When touching with fingers a hot plate, the hand is moved quickly away, before it is realized that the plate was very hot, which means, before the brain (thalamus) realized that there is danger to the fingers. The protection automatism is organized at the spinal cord level for being fast. The conduction time of the painful information, from pain receptors to reach the brain, would be too long for protection. Hands or feet would have been already damaged.
It has been shown that Coordination Dynamics Therapy (CDT) can improve or repair Central Nervous System (CNS) functioning after stroke [5], traumatic brain injury [6, 7], spinal cord injury [1, 8-11], cerebellar injury [12], cerebral palsy [13], hypoxic brain injury [14], in Parkinson’s disease [15], spina bifida (myelomeningocele) [16] and scoliosis [17]. Speech had been induced and improved in a patient with severe cerebral palsy [18].A permanent coma patient could be brought out-of-coma and relearned to speak [19] and cancer grows could be inhibited through CDT [20, 21]. Cardio-vascular performance could be improved. There is indication that the general health can be improved via CDT to live longer with a better quality of life.
Method
With the development of new electrophysiologic recording methods [22] (Figure 1), it became possible to analyze CNS functioning at the single-neuron level under rather natural conditions. With the single-nerve fiber action potential recording method, single-nerve fiber action potentials can be recorded from sacral nerve roots, running in and out of the spinal cord and CNS functions can be analyzed. By comparing CNS functioning in brain-dead humans (where the spinal cord is functioning rather physiologically) and patients with spinal cord injury, injury-induced changes of CNS functioning can be measured and partly repaired. Mainly the phase and frequency coordination [23] of neuron firing becomes impaired following injury. This impaired coordination among neuron firing can efficiently be repaired through exercising on the special CDT device (Figure 2).

Figure 1: Schematic layout of the methods used to study the self-organization and repair of neuronal networks of the human CNS. A. Single-nerve fiber action potential (AP) recording method to measure with wire electrodes simultaneously from a set of single afferent (AP phase upward) and efferent (AP phase downward) nerve fibers to analyze the simultaneous impulse traffic running in and out of the spinal cord. B. Morphometry of nerve roots and nerves to identify groups of nerve fibers. C, D. By performing surface electromyography (sEMG) with up to 4 electrode pairs (2 indifferent electrodes, 1 earth electrode; pre-amplification x1000, 4-channel oscilloscope) the changes of motor programs were measured (C). When recording from appropriate patients, natural activation patterns of several single-motor units were obtained (D) and coordination between motor unit firing could be studied. E. Coordination between arms and leg movements was quantified by the single integrative parameter, arrhythmicity of turning (df/dt or df/dt/f; f = frequency) during exercising on a special coordination dynamics therapy device. (Figure made by the Author).

Figure 2: Training of neck, trunk and pelvis control, besides the training of arm and leg movements, of a patient with SCI (Th10) during exercising trunk rotational movements on the special CDT device in the lying position. Due to the coordination changes of arms and legs between pace and trot gait all vertebra segments are trained. During exercising coordinated arm, leg and trunk movements, the coordinated firing of neurons and sub-neural networks are improved. This special CDT device for measuring and therapy (int.pat.) is produced by the firm: Giger Engineering, Martin Giger dipl.Ing.ETH/SIA, Herrenweg 1, 4500 Solothurn, Switzerland, www.g-medicals.ch.
The special CDT device has three important properties. First, the patient performs coordinated arm, leg and trunk movements when exercising on it. The training of integrative patterns take care of that the pathologic organization cannot escape from repair by shifting to another part of the CNS and the whole CNS, including the injured parts, is reorganized so that other CNS parts can take function over through plasticity. Second, the device is extremely exact, so that the endplate potentials in the neural networks (approximately 5ms long) overlap, to improve the efficiency of organization. In spinal cord injury, for example, the transmission over the injury site is increased. Third, the coordination between arm and leg movements changes from pace to trot gait, imposed by the device. The intermediate coordination patterns between pace and trot gait are difficult to generate for the CNS networks. If the patients CNS learned to generate these intermediate patterns, imposed by the device, then the networks have learned to function better in the deep complexity of CNS organization. The neural networks are repaired in the deep complexity of CNS organization. The patient’s nervous system learned by turning from the device, to function more physiologic through improving especially the phase and frequency coordination of neuron firing. This phase and frequency coordination can be measured by the single-nerve fiber action potential recording method invasively and by single-motor unit surface electromyography on-invasively (Figure 1) [24].
Since through the damage of the spinal cord or brain also nervous tissue is lost, certain movement shave to be trained so that other parts of the CNS can take function over through plasticity. Efficient training patterns are the automatisms creeping, crawling, up-righting, walking, sky-walking (Figure 3C) and running. The jumping on springboard (Figure 3B) improves especially the functioning of premotor spinal oscillators [25], activating the muscle fibers. Also the balance has to be trained (Figure 3A) during pattern performance.
Further, through learning transfer [26] other CNS functions improve which cannot be trained or are difficult to train. Urinary bladder functions, for example, can be repaired especially when exercising on the special CDT device and jumping on springboard (Figure 3) [18]. Only those functions can be trained which the patient is able to train with or without support.

Figure 3: A. SCI patient Nefeli during exercising on a special CDT device on a ball at the beach, to train apart from phase and frequency coordination also balance. B. By the Author supported jumping on springboard in antiphase. C. Nefeli during sky-walking. To achieve a large stride length, the Author is supporting the feet to avoid the slipping of the feet from the pedals.
Results
Improvement of Walking and Continence following Spinal Cord Injury
In the 5.5-years-old Nefeli a neuroblastoma was found to grow from the Th10 ganglion. With the surgery to remove the cancer, she suffered an incomplete SCI at Th10/11 levels by medical malpractice (Figures 4-6). An 8-months-rehabilitation in Switzerland brought only little progress. Most of the repair was probably due to spontaneous recovery. When Nefeli started school, she was incontinent and could not walk. Assistance helped her to manage at school (Figure 7B).
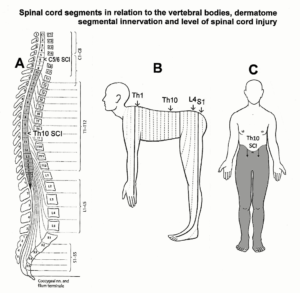
Figure 4: A. Spinal cord segments and their relation to the vertebral bodies. Note the Ascensus of the spinal cord, giving rise to the long cauda equina nerve roots. B. Approximate segmental innervations of the skin. C. Below the SCI level there is loss of sensitivity and loss of connectivity to muscle and other organs. (Duus’, Topical Diagnosis in Neurology, M Baehr, M Frotscher, Thieme, 2005).
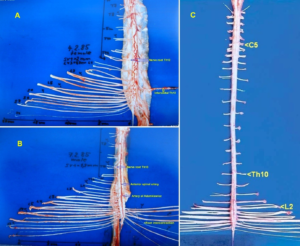
Figure 5: Human spinal cord from dorsal (A) and ventral (B, C). Intumescentia cervicalis and lumbosacralis are visible in C. The caudal ventral roots are thinner than the dorsal roots. The passage of the artery spinalis magna (Artery of Adamkiewicz) and the anterior spinal artery are indicated. The C5, Th10 and L2 roots and the intercostal nerve Th12 are indicated. Dissections by the Author.
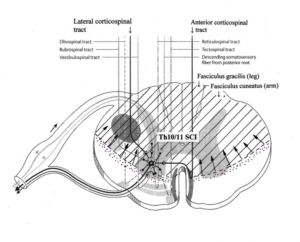
Figure 6: Spinal cord cross section with indicated approximate injury (cross-hatched) and loss of interneuron (dotted area) of the patient Nefeli. Synapses of descending motor tracts onto anterior horn neurons are shown.

Figure 7: A. The 5.5-year-old Nefeli after suffering an incomplete SCI at Th10 by medical malpractice. B. Nefeli after eight months of conventional children rehabilitation in Switzerland (Affoltern). Sticks and orthosis were needed. C, D. Ten-year-old patient Nefeli after six months of CDT. At school she can walk again and can write at the white board.
At an age of 9, Nefeli started CDT with the Author. Spasmolytic drug and urinary bladder medications were stopped. Following four years of CDT, Nefeli became continent and she learned to walk again (Figure 7D) with some balance problems. She learned to creep and crawl. Even a bit of running and jumping became possible. At an age of 13 years, Nefeli learned a bit to ride a normal two-wheel bicycle (Figure 8) [1].

Figure 8: The SCI patient Nefeli just after learning to ride a normal bicycle at an age of 12.5 years (A). She manages also to ride curves (slalom) (B). She still has problems to keep the feet on the pedals, but when she slips from pedals, she has no problems to keep the balance (C). Note that she has to concentrate very much to keep the feet on the pedals (A), seven years after the SCI injury.
With increasing age, the scoliosis got worse, because one or two intercostals were cut when removing the neuroblastoma. But scoliosis can be reduced, when exercising on the special CDT device in the lying position with trunk rotation (Figure 1) [17]. Because the orthopedic gave the instruction that Nefeli should not move too much, because the scoliosis will increase, Nefeli trained very little and the CNS repair did not progress any more. At an age of 14 a rod was implanted to keep the spine straighter. This operation was probably justified, even though not all training possibilities were used so far.
The orthopedic promised Nefeli and the parents that an operational correction of the legs will improve her walking performance strongly, not knowing that in such a critical incomplete SCIan operation is contraindicated (Introduction), because the plasticity will reduce and her movements will get worse. Against the strong advice of the Author to avoid surgery, an operation of both feet bones was performed (Figure 9) and a tendon of the left leg elongated.

Figure 9: Performed foot operation, which threw the spinal cord injury patient Nefeli two years of movement-based learning therapy backwards. A transposed piece of bone cannot be seen. The seemingly simple operation had tremendous consequences for the patients CNS functioning and her everyday life.
In the next section, the reduction of movement functions following the operation will be tackled in detail. To say it clearly, one cannot improve CNS functioning through operations and also not by administering drugs. Movement-based learning is the only causal therapy.
Dramatic loss of Repaired CNS functions due to the Orthopedic Operation
After the bone operation of the feet (Figure 9) and a tendon elongation of the left leg, the patient had the legs in plaster up to the knees and should stretch and flexes the legs according to the instructions of the surgeon. But a few days after the operation, slowly the stretching became more difficult till the patient was unable to stretch the legs. Extreme strong flexor spasticity, cramps and rigor had appeared and the patient had not sufficient volitional power anymore to stretch the legs. Nefeli struggled with the farther for 10 days, because he thought that she was able to move the legs by herself, according to the information of the surgeon. The patient Nefeli had to stay in bed and had to be carried to the toilet because she could not move the legs anymore. They were always in an extreme flexed position (Figure 10).

Figure 10: Six weeks after the operation, the SCI patient cannot move the legs anymore, because of extreme flexor spasticity, which developed one to two weeks after the operation.
When the Author saw her the first time, 6 weeks after the operation, she was in bed and could not move the legs (Figure 10). The legs were always in an extreme flexed position. When it became possible with tricks to extend the legs a bit (Figure 11A), they went immediately into the flexed position when touched (Figure 11B), independently where the legs were touched. When trying to put her on the feet, the feet flexed (Figure 11C), so that a standing was impossible. This flexor spasticity could also be seen when holding her with the arms. Figure 12B shows the physiological positioning of the legs of the healthy sister. Before the second operation, after three years of CDT, Nefeli had some extensor spasticity (Figure 12A), which helped her to stand straight. After the second operation, the legs were clearly in a strong flexed position (Figure 12C).

Figure 11: When it became possible by some tricks to get the legs somehow stretched (A) and one touched the legs, they went immediately into flexor spasticity position (B). When the Author tried to put the SCI patient onto the legs for standing, the legs flexed immediately (C).

Figure 12: The extreme flexor spasticity of the SCI patient was also visible when holding her. The physiologic holding position can be seen when the Author was holding the patient’s sister (B). Before the second operation, the patient’s legs were more stretched because of the mild extensor spasticity (A), which can be helpful for standing and walking. After the second operation, the legs were strongly flexed, due to the extreme flexor spasticity (C).
The question was now, how can the by the operation damaged CNS repaired, to make the patient move again. Wherever touching the legs, they went by strong flexor spasticity into the flexed position. No movement training seemed to be possible. The Author tried with the patient many movement possibilities, which could be used for training to reduce the extreme flexor spasticity. Luckily, they found a movement. When putting on the orthoses (Figure 13A), the flexor spasticity was not that strong, probably because the input was more general and unspecific. A bit of turning on the special CDT device in the sitting position became possible (Figure 13B). Even though that sitting position was unphysiological and not good for the scoliosis, the patient trained in that position. With ongoing training, the flexor spasticity reduced. Following two months of therapy, Nefeli became able to exercise also a bit in the lying position which was aphysiologic pattern for her (Figure 13C). At the beginning, this turning in the lying position was not possible, because Nefeli did not have sufficient power to train against spasticity and rigor. Touching the legs for support made it harder for her to turn. Also, at the beginning it was nearly impossible for the Author to fix her legs in the lying position, because the legs were too stiff. The Author and also the patient could not understand why the turning in the sitting position became possible and why not in the lying position.
 Figure 13: To be able to exercise on the special CDT device, the SCI patient Nefeli had to wear orthoses up to the knees. The for the back healthy lying position (C) was only possible 3 months after the operation because of spasticity and rigidity.
Figure 13: To be able to exercise on the special CDT device, the SCI patient Nefeli had to wear orthoses up to the knees. The for the back healthy lying position (C) was only possible 3 months after the operation because of spasticity and rigidity.
The Author had also no idea how he could have treated the patient without the special CDT device. Anyhow, training became possible, spasticity reduced and leg movements became slowly possible again. Spasmolytic drugs for 5 days were tried by the surgeon without success. Apart from the side effects, spasmolytic drugs are not helpful in incomplete SCI, because they do not only reduce the spasticity, but also reduce the remained volitional muscle power.
Repair Achieved 3.5 Months after the Operation through 2 Months of CDT
The spinal cord injury was the result of a mistake during the first operation. When removing the cancer starting from the Th10 ganglion, the hemostasis was wrongly performed in the way that blood went into the spinal canal and caused during 3 days through pressure an incomplete spinal cord injury. The pain of the crying child after the operation was ignored by the operating team. When the SCI manifested itself, after 3 days, in the way that the patient could not stand anymore and became incontinent, the parents just took Nefeli to another hospital.
Different movement performances will now be compared before and after the second (feet) operation to see the results of the feet operation, to show how much repair was destroyed by the second operation.
Walking
Before the second operation, 9 years after the first operation, the patient Nefeli was able to walk with and without crutches (Figure 14A, B) up to 1000m;3.5 months after the second operation she could walk only with crutches up to 10m (Figure 14C).She needed shoes and the arms were just strong enough to keep her up.

Figure 14: The walking performance of the SCI patient before (A, B) and 3 months after the second operation (C).
Running, jumping and getting up from the Floor
Before the second operation Nefeli could run and jump a bit (Figure 15A, B) and could get up from the floor (Figure 15C) without support (Figure 16). After the operation she could not get up from the floor anymore without support and could not run and jump anymore.

Figure 15: Before the second operation the SCI patient Nefeli was able to run and jump a bit (A, B) and she enjoyed it very much. She was very relaxed and happy afterwards (C).
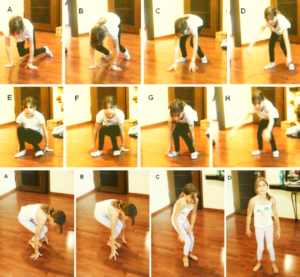
Figure 16: Before the second operation, the spinal cord injury patient Nefeli was able to get up from the floor in two ways. Even when having balance problems during getting up, she managed well (lower A-D). When really falling, there was no risk of damage, because all protection mechanisms walked well. After the operation she could only get up from the floor with substantial support.
Staying Straight
Before the second operation, Nefeli could nearly stay straight (Figure 17A, B); 3.5 months after the operation she could only stay less straight (Figure 17C, D).

Figure 17: Free standing of the SCI patient before the second operation (A, B) and after (C, D). In spite of pushing herself up with crutches (D), the flexion of the legs was stronger than before the operation.
Foot arch
Before the operation, the right foot had no arch if full body weight was on it (Figure 18A), which could not be repaired so far. Such foot arch repair needs long-time training on the forefoot. After the operation, the right foot arch was not much better (Figure 18D) and could not trained sufficiently anymore because of the necessary orthoses. Before the operation no orthoses were needed and the foot arch could be trained.
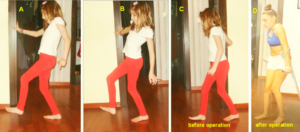
Figure 18: Bar foot walking of the patient Nefeli with a spinal cord injury before the second operation (A-C). Three months after the operation she could not walk freely any more (D).
A physiologic foot arch is important; otherwise pain may occur later during walking. The patients left foot had a physiologic arch (Figure 18B). The right foot arch was lost when putting weight on it (Figure 18A). The foot arch muscles (Figure 19) could not be activated sufficient strong by her because of the SCI. On the long term, the foot bones may rearrange (Figure 20). But a training on the forefoot can repair the foot arch in cerebral palsy and probably also in incomplete SCI.
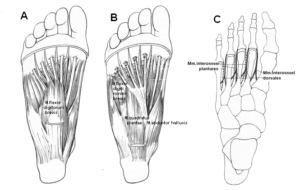
Figure 19: Superficial (A) and deep (B) plantar muscles of the foot to support the arch of the foot. C. Mm. interossei plantares and dorsalis. (Pocket Atlas of Human Anatomy, W Dauber, Thieme, 1976, 2007).
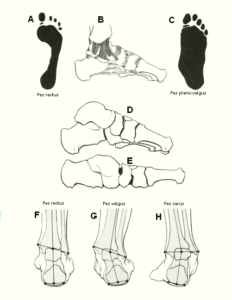
Figure 20: A. Healthy foot print (pes rectus). B. Foot ligaments. C. Pes plano-valgus. D. Bones of the healthy foot arch from medial. E. Broken foot arch from medial. (Taschenatlas der Anatomie, Bewegungsapparat, Kahle W, Leonhardt H, Platzer W, Thieme, 1975).
Walking on Sky Walker and Training Symmetries
Before the second operation, Nefeli could walk on the sky walker easily (Figure 21A). When exercising with crossed arms or legs, even the right-left symmetry via the corpus callosum could be trained (Figure 21B, C). Also, some stretching was possible on the sky walker (Figure 22A). After the second operation, the right leg went into the flexed position due to flexor spasticity (Figure 22B). After 3.5 months, a bit of exercising on the sky walker became possible if Nefeli was wearing shoes and the feet were fixed.

Figure 21: Different movement patterns on the sky-walker. A. trot gait. B, C. Combinations of pace and trot gait to activate commissural fibers (Figure 23D).
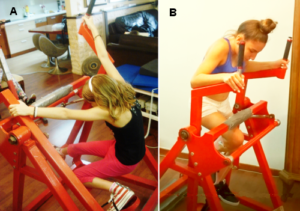
Figure 22: A. Sky-walker used for stretching in the ten-year-old Nefeli with a spinal cord injury (before the second operation). B. Two months after the second operation, the 14-year-old Nefeli tried to sky-walk, but the right leg went immediately into the extreme flexor spasticity pattern.
In CNS injuries, malformations, degenerations and brain cancer operations, the improvement of right-left symmetries is important. It can be trained on the sky walker (Figure 21), on the special CDT device (Figure 23C) and on the floor (Figure 23A, B). The corpus callosum and other right-left connecting tracts (Figure 23D) allow that functions of one hemisphere to be partly taken over by the other hemisphere through plasticity, especially for children under 10 years. Scoliosis can also be improved through such movements. Till3.5 months after the second operation, these movements could not be trained anymore. The scoliosis became worse (Figure 13A, B) in spite of a fixation of the spine by a rod.
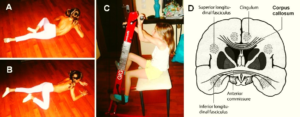
Figure 23: A, B. Ten-year-old patient with an incomplete SCI at the Th10 level during creeping. Note, because of the severe scoliosis, the creeping is not symmetrical. The rotation to the left is limited because of the scoliosis. C. Training of right-left symmetry via the corpus callosum (D) when exercising on the special CDT device with crossed arms. (D, Duus’, Topical Diagnosis in Neurology, M Baehr, M Frotscher, Thieme, 2005).
Repair Achieved 6 Months after the Second Operation
Six months after the operation, there was some improvement in CNS functioning. The patient relearned a bit to walk without support when using orthoses (Figure 24). But the performance of the walking was not better than before the operation. Nefeli still had to swing the legs during walking (Figure 24B, C). For the walking without orthoses, she needed substantial support (Figure 25A, B). The dorsal flexion of the right big toe was strong (Figure 25C). Spasticity of toes hinder to put on shoes.

Figure 24: Free walking of the 14-year-old Nefeli after the second operation when wearing shoes. She is still swinging the right leg because of no proper walking performance (B, C). The balance during walking did not improve; it got worse.
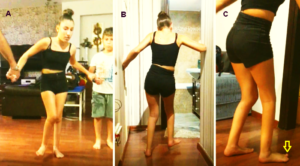
Figure 25:14-year-old Nefeli after the second operation. She was able to walk bar foot only with strong support (A, B). The right big toe was strongly dorsal flexed during walking.
Before the operation, the patient could walk with and without shoes (Figure 18A-C) with some balance problems. Relaxed walking of long distances, she managed easily when touching another person and getting in this way additional stability support.
Six months after the second operation, the balance problem had not improved. It was worse. When walking without shoes, there was a risk of foot damage when falling; especially the right ‘bad’ foot was at danger. Before the operation there was no risk when falling. Altogether, the walking after the second operation was by far not as good as before the operation.
No Substantial Further Walking Improvement 8 Months after the Operation
The walking performance did not improve much till eight months after the operation. Luckily, urinary bladder functioning did not get worse with the second operation.
The surgeon had promised Nefeli and her parents a much better performance of the walking after the operation, which did not take place. The surgeon only raised false hope and made her movement performance worse.
Discussion
Comparison between an Operation and a Movement-Based Learning Therapy in CNS Injury or Malformation
It has been shown that the SCI patient Nefeli lost something like two years of movement-based learning therapy (CDT) through an operation of the feet. This loss of repair of the CNS was mainly due to the missing knowledge of that orthopedic surgeon inhuman repair-neurophysiology. Damage or disturbances of the nervous system, including the vegetative divisions, have to be attacked through movement-based learning and not through an operation. Of course, if the patient has not the mental discipline to train, then a drug therapy or an operation is the only choice. Patients and parents complain that they are not informed by physicians about other treatments.
A question is now, how would the repair of Nefeli been, if she would not have been operated. Some kind of comparison is given here, even though there are differences between the repair in SCI and cerebral palsy.
Nefeli trained often together with the cerebral palsy girl Sophie who had an atrophy of the cerebellum and pons. At the beginning of CDT, Sophie could not stand and walk (Figure 26A, B), was incontinent and had no protection automatisms. When falling, she would hurt herself because of missing protection automatisms, located mainly in the cerebellum. With training, the functioning of the cerebellum improved and she learned the protection automatisms. Now standing and walking could be trained, because the danger of damage was over, since the protection automatisms worked now in her. Through 4 years of CDT, Sophie learned to stand freely and walk without falling (Figure 26C). She became continent and her higher mental functions improved.

Figure 26: A, B. At the beginning of coordination dynamics therapy, the cerebral palsy girl Sophie could not stand and walk and was incontinent. C. After 4 years of CDT she could train together with Nefeli the walking in interpersonal coordination.
Also Sophie had no foot arches and surgeons said that she will get pain in the future because of the missing foot arches. When the parents saw the operation results of Nefeli, they decided against an operation and used CDT for further progress. For building up a foot arch, Sophie trained walking on the forefoot and climbing staircases in the right way. Via the forefoot the patient has to feel the edges of the staircases for proper climbing. The building up of foot arches may take a few years of training, but the malformed CNS is not injured by an additional operation. Anyway, Sophie has to learn to walk better and to run and has to climb the staircases in the physiologic way for safety.
Five months after the feet operation, Nefeli could just walk a bit with orthosis and needed support when moving to the WC at home (Figure 27A), whereas the not feet operated Sophie learned in the meantime the running (Figure 27B, C, D). Nefeli and her parents were getting depressed when seeing the improvement in Sophie and the loss of repair in Nefeli.

Figure 27: A. The SCI patient Nefeli needed after the feet operation again support when going at home to the WC. B-D. The cerebral palsy girl learned in the meantime the running. Note from the expression of the face of Sophie, how hard she is fighting to run. She liked the running, even though being very hard.
It is the duty of surgeons not just to see only their own operational repair strategy. They have to tell patients and parents about alternatives. Such behavior of some surgeons ruins the reputation of medicine.
CDT is a Healthy Non-Invasive Neurotherapy with Nearly No Alternatives
Figure 28 and Figure 29show that when exercising on a special CDT device, nearly the whole brain (CNS, Figure 28A) is activated for repair. If one includes coordinated speech in the movement training by giving coordinated instructions ‘right-left’ or ‘one-two-three’, the efficiency of repair can further be increased. Even cognitive visual input can be included to enhance the repair.
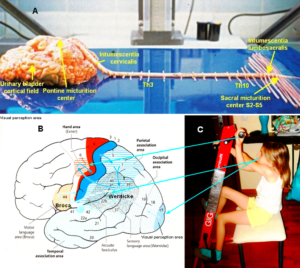
Figure 28: A: Unfixed human CNS dissected by the Author. Lumbosacral and cervical enlargements of the spinal cord (intumescentia lumbosacralis and cervicalis) are indicated. The S1 root is the last thick nerve root. The urinary bladder cortical field is inside and cannot to be seen. Such a dissection of the human CNS is not simple. To take the brain out during an autopsy in the Pathology department is standard. Following 50 to 100 cadaver dissection, the Author was quite experienced to remove the spinal cord. But to remove the brain in connection with the spinal cord from a cadaver is difficult, if one does not want to damage the outside of the cadaver too much, so that relations of the dead loved person can say in peace goodbye. B, C. Efficient coordination dynamics therapy through including the coordination of vision, speech and coordinated arm and leg movements (C) for brain and spinal cord injury repair. Especially the multimodal association areas (B), in the deep complexity of CNS organization, are activated for repair. This neurotherapy is also efficient for a language repair of the Wernicke area of the brain cancer patients. (B; Duus’, Topical Diagnosis in Neurology, M Baehr, M Frotscher, Thieme, 2005).

Figure 29: Relative sizes of cortical representations of different parts of the body which are activated when exercising on special CDT devices in coordination with instructions. Nearly the whole somatosensory (A) and motor cortical fields (B) are activated. When moving only the legs, as in case of a fitness bicycle, the activated areas are relatively small. Note, the cortical representation of the urinary bladder is close to the representation of the toes, and during jumping the forefoot and the toes are activated. The patient Nefeli in ‘C’ suffered a spinal cord injury during a cancer removal by medical malpractice and had also the urinary bladder to be repaired. (A, B; Duus’, Topical Diagnosis in Neurology, M Baehr, M Frotscher, Thieme, 2005; from Penfield W and Rasmussen T, New York, 1950).
Progress in Human CNS Repair Achieved through Basic Medical Research which is not Organized Worldwide
The progress in human CNS repair was achieved through basic medical research. Based on a new recording method (the single-nerve fiber action potential recording method, Figure 1A), a classification scheme of human peripheral nerve fibers [28] could be developed. Through measuring at the single-neuron level the impulse traffic of identified neurons which runs into and out of the spinal cord, premotor spinal oscillators could be found and the important ‘phase and frequency coordination’ [23]among neuron firings for the self-organization of human neural networks measured (Figure 30). Out of the difference between physiologic and pathologic functioning, a neural repair method, the CDT, was developed with which it became possible to repair the injured or malformed human CNS or improve its functioning in the healthy case. Since the nervous system is involved in nearly all body functions, the general health of humans can be improved to live longer with a better quality of life by 10 to 20 years.
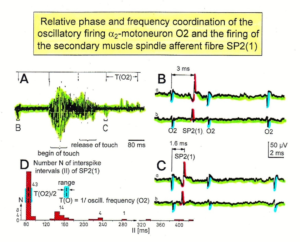
Figure 30: Time relation between the occurrence of the action potentials (APs) of oscillatory firing a2-motoneuron O2 and the firing of the secondary muscle spindle afferent fiber SP2(1). Brain-dead human HT6. S4 dorsal root recording. A. Overall view of the used sweep piece; only trace “a” shown. Four oscillation cycle periods of motoneuron O2 are indicated (T (O2)). The APs of the impulse trains can be recognized only partly, because of the slow time base and poor digitalization. One impulse train (dashed arrow) is lost in the touch stimulated activity, which consists of a touch (large overall activity) and a release part (lower overall amplitude). B, C. Sweep pieces from A, time stretched. In B, motoneuron impulse train APs are marked O2, spindle afferent APs are marked SP2 (1). Note that the APs of the spindle afferent fiber are not time-locked to the first AP of the impulse train of the rhythmically firing motoneuron (relative phase coordination). Digitalization four times better than in A, but still rather poor, as can be seen from the low amplitudes of the motoneuron APs on trace “b” in C. D. Occurrence of interspike intervals of the secondary muscle spindle afferent fiber SP2(1). The numbers give the amount of IIs in each distribution peak. The oscillation period of motoneuron O2 (and the range of variation) and the half period are indicated by short dashed lines. Note that the IIs of fiber SP2 (1) are very similar to the oscillation period (or the half of it) of a2-motoneuron O2 (relative frequency coordination).
The treatment of the patients Nefeli and Sophie can be followed up on a video film with the heading ‘From brain repair to Covid-19 treatment via Coordination Dynamics Therapy’ [27].
No Sign of Long-Term Treatment of Covid-19 Infections around the World and the Lack of Basic Medical (Human) Research
It has been published that more has to be done than just to develop a vaccine against covid-19 viruses [21, 27, 28]. The vaccine efficiency will be much less than 100% and the side effects of the drugs will only be known in the future. The side effect of the pain killer Contergan was that babies were born only with fingers instead of arms. Sometimes Contergan adults come to conferences or exhibitions to warn of drug side effects.
For a long-term treatment of covid-19 infections, especially the functions of the lung have to be improved to partly protect against covid-19 and other infections. The lung is the first protective shield against infections (Figure 31). Already 15% of the covid-19 infections are due to environmental pollution. Forests have to be planted around the world for improving the breathing air. Pollution and wrong ionization of the breathing air change the pH value of the surfactant of the lung from 5 in the direction of 6 and ruins the first protective shield against covid-19 infections (Figure 31) with the consequence that the immune system of the surfactant is not working anymore and that the surfactant becomes crackly to allow viruses to penetrate the lung epithelia (Figure 31D). Ventilation systems must offer breathing air with negative ionization to keep the pH at 5. Fresh clean air with the natural negative ionization is the best for breathing. Climatization systems are the breading places for viruses and bacteria. To stop a climatization system is insufficient; also the outlets have to be covered to stop viruses and bacteria to come out.

Figure 31: Physiologic and pathologic pulmonary epithelial functions to impede virus and bacterial infections. When living in a healthy surrounding (A) and exercising (E, F), the lung epithelia is in a healthy condition (C) and can partially protect against infections to a certain extent; the surfactant has a pH of 5 and is liquid so that macrophages can move about and engulf viruses, bacteria and particulates. The lung protection shield against infections is working. When living in a polluted surrounding with wrong air ionization (B), the surfactant gets a wrong pH value (pH value = 6) and becomes more rigid so that macrophages cannot move easily about and attack and engulf viruses and bacteria (D). Viruses can also invade the body through cracks. The pulmonary surfactant cannot protect any more against infections. Viruses and bacteria get into the body. Critical patients may die (G).
Today (25.1.2021) a well-known libraryin Berlin (‘Staatsbibliothek Unter den Linden’) was re-opened with repair costs of approximately 500 million US Dollar. The climatization system supplies in the future the students with noise, viruses and bacteria, which are breaded in the ventilation/climatization system, and will bring them to the students via the circulating air.
The air, associated with the surrounding of schools, is of importance. Plenty of trees have to be planted around schools to improve the breathing air for pupils at school. Exercising or training at the seaside (Figure 3A) or in the forest (Figure 31A) is healthy.
Generally, the hygiene has to be improved. Handles and hand rails have to be, for example, made of brass which is bacteriostatic. Also viruses will have problems to survive on clean brass. In Germany and Switzerland, the Author has not seen any yellow-looking handles so far. For cleaning the hands, soap is best because the soap ruins the lipid membrane of viruses so that they cannot attach to cells anymore and washing the hands with soap does not ruin the healthy bacteria of the skin for protection. Whereas disinfections kill pathologic and healthy microbes of the skin. Specific knowledge seems not to be of interest to the world society. Research progress is ignored.
Apart from the lockdowns, nothing seriously has been done so far to stop infections on the long-term. Patients suffer or die because they are afraid to go to physicians. The Author cannot look sufficiently for his patients, because they are afraid to see him or the lockdown is blocking the consultation. His patient with the brain tumor (oligodendroglioma WHO III) is at high risk to die, because the Author cannot supervise him for an optimal therapy to inhibit cancer regrowing [21]. Supervising the patient Nefeli via telephone is also not working. She needs direct training with the Author.
The lack of qualified human (medical) research for a few decades, apart from statistics and a few exceptions, is one reason for the covid-19 pandemic. The pandemic is therefore self-made. Only qualified medical research opens new possibilities of treatment.
The restrictions of basic human rights are ethically only justified, if the mistakes of medical research in the past are uncovered and investments in infrastructure and the implementation of the clinical research, apart from statistic, are executed. Biological research is no substitute for human research. With respect to spinal cord injury, for example, in goldfish the spinal cord is regenerating spontaneously following injury.
References
- Schalow G (2019) Regeneration of the human spinal cord via coordination dynamics therapy. Peertechz Publications, 97 pp. eBook.
- Weiss P, Brown PF (1941) Electromyographic study on recoordination of leg movements in poliomyolitis patients with transposed tendons. Proceedings of the Society for Exper. Biology and Medicine 48: 384-387.
- Sperry RW (1945) The problem of central nervous reorganosation after nerve regeneration and muscle transposition. Quart. Rev. Biol 20: 311-369.
- Sperry RW (1947) Effect of crossing nerves to antagonistic limb muscles in the monkey. Arch. Neurol. Psychiat. Chicago 58: 452-473.
- Schalow G (2002) Stroke recovery induced by coordination dynamic therapy and quantified by the coordination dynamic recording method. Electromyogr. Clin. Neurophysiol 42: 85-104.
- Schalow G (2002) Improvement after traumatic brain injury achieved by coordination dynamic therapy. Electromyogr. Clin. Neurophysiol 42: 195-203.
- Schalow G, Jaigma P (2006) Improvement in severe traumatic brain injury induced by coordination dynamics therapy in comparison to physiologic CNS development. Electromyogr. Clin. Neurophysiol 46: 195-209.
- Schalow G (2002) Recovery from spinal cord injury achieved by 3 months of coordination dynamic therapy. Electromyogr. Clin. Neurophysiol 42: 367-376.
- Schalow G (2003) Partial cure of spinal cord injury achieved by 6 to 13 months of coordination dynamic therapy. Electromyogr. Clin. Neurophysiol 43: 281-292.
- Schalow G, Jaigma P, Belle VK (2009) Near-total functional recovery achieved in partial spinal cord injury (50% injury) after 3 years of coordination dynamics therapy. Electromyogr. Clin. Neurophysiol 49: 67-91.
- Schalow G (2010) Cure of urinary bladder functions in severe (95%) motoric complete cervical spinal cord injury in human. Electromyogr. Clin. Neurophysiol 50: 155-179.
- Schalow G (2006) Cerebellar injury improvement achieved by coordination dynamics therapy. Electromyogr. Clin. Neurophysiol 46: 433-439.
- Schalow G, Jaigma P (2005) Cerebral palsy improvement achieved by coordination dynamics therapy. Electromyogr. Clin. Neurophysiol 45: 433-445.
- Schalow G (2006) Hypoxic brain injury improvement induced by coordination dynamics therapy in comparison to CNS development. Electromyogr. Clin. Neurophysiol 46: 171-183.
- Schalow G, Pääsuke M, Ereline J, Gapeyeva H (2004) Improvement in Parkinson’s disease patients achieved by coordination dynamics therapy. Electromyogr. Clin. Neurophysiol 44: 67-73.
- Schalow G, Nyffeler T (2001) Koordinationsdynamik-Therapie: Myelomeningozele (Spina bifida). Physiotherapie.
- Schalow G, Nyffeler T (2000) Koordinatiosdynamik-Therapie: Skoliose. Physiotherapy.
- Schalow G (2013) Human Neurophysiology: Development and Repair of the Human Central Nervous System. Nova Science Publishers, Inc, Hauppauge NY, USA, 734 pp.
- Schalow G (2019) Permanent coma patient re-learned to speak via Coordination Dynamics Therapy. Arch. Clin. Med. Case Rep 3: 33-50.
- Schalow G (2017) Breast cancer growth inhibition via Coordination Dynamics Therapy. In: “Horizons in Cancer Research. Volume 68”. Editor: Hiroto S. Watanabe. Nova Science Publishers, Inc, Hauppauge NY, USA, pp. 125-151.
- Schalow G (2020) Anaplastic oligodendroglioma WHO III brain cancer-patient recovered following operation, radiation and chemotherapy through Coordination Dynamics Therapy, which is also a Covid-19 treatment without ventilator. Int. J. Med. Clin. Imaging 5: 165-210.
- Schalow G, Lang G (1987) Recording of Single Unit Potentials in Human Spinal Nerve Roots: a New Diagnostic Tool. Acta Neurochir. 86: 25-29.
- Schalow G (2005) Phase and frequency coordination between neuron firing as an integrative mechanism of human CNS self-organization. Electromyogr. Clin. Neurophysiol 45: 369-383.
- Schalow G (2006) Surface EMG- and coordination dynamics measurements-assisted cerebellar diagnosis in a patient with cerebellar injury. Electromyogr. Neurophysiol. 46: 371-384.
- Schalow G (1993) Spinal oscillators in man under normal and pathologic conditions. Clin. Neurophysiol 33: 409-426.
- Schalow G (2010) Scientific basis for learning transfer from movements to urinary bladder functions for bladder repair in patients with spinal cord injury. Electromyogr. Clin. Neurophysiol 50: 339-395.
- Schalow G (2020) From brain repair to Covid-19 treatment via Coordination Dynamics Therapy. (Video film contains therapy movements of patients’ recent publications). Video conference August 19, 2020. (Download from coordination-dynamics-therapy.com).
- Schalow G (2020) Classification and Identification of Human Peripheral Nerve Fibers by Conduction Velocity, Nerve Fiber Diameter and Natural Firing Patterns with Consequences for CNS Repair and Covid-19 Infection Treatment. Int. J. Med. Clin. Imaging 5: 231-314.