Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
An isolated technique involving the transfer of the flexor hallucis longus tendon for elderly individuals with chronic insertional Achilles tendon disorders: A retrospective study utilizing validated ankle scoring systems
Kassem El Houcheimi*, Nabih Berjaoui
1Nabih Berjaoui MBBS, BScs, Lebanon
Received Date: February 11, 2025; Accepted Date: February 21, 2025Published Date: February 28, 2025;
*Corresponding author: Kassem El Houcheimi, FACS, MBA, Orthopedic surgeon, Department of Orthopedics, Clemenceau Medical Center Dubai.
Citation: Houcheimi K E, Berjaoui N; An isolated technique involving the transfer of the flexor hallucis longus tendon for elderly individuals with chronic insertional Achilles tendon disorders: A retrospective study utilizing validated ankle scoring systems. Adv Ortho and Sprts Med: AOASM-202
DOI: 10.37722/AOASM.2025102
Abstract
This study aimed to demonstrate the reliability of augmentation and reconstruction of chronic Achilles tendon pathologies using the flexor hallucis longus tendon with a single interference screw in elderly Asian patients. A single center case series was performed, with patient satisfaction and outcomes measured using visual acuity scores, Foot and Ankle Disability Index, and American Orthopaedic Foot & Ankle Society scores. Results showed a mean age of 55 years, all ankle scores improved at 2 year follow-up, and overall patient satisfaction was 100%. No complications or re-rupture were observed during the study period. The study concludes that chronic insertional Achilles tendinopathy treatment with FHL tendon transfer has reliable and good outcomes, but a larger sample size and longer follow-up would be beneficial.
Introduction
Achilles tendonopathy and rupture can impede movement and cause chronic pain and swelling. This condition can limit the ability to squat and stand on tiptoe and can interfere with daily life 1,2. The significant space between the muscles can make it difficult to decompress the muscle and reattach the muscle to the calcaneus during surgery 3. Flexor pollicis longus tendon replacement has been reported to have good results 4. The flexor hallucis longus is the second strongest plantar flexor of the ankle and is a good muscle whose proximity to the Achilles tendon allows for easy contraction and visible involvement, thus transmitting forces along a similar pathway to the Achilles tendon 5,6. The passage of the flexor hallucis longus brevis tendon to the level of the joint at the origin of the fibrous bone has been well documented and was used in this study1,6. There is no change in pressure at the first metatarsophalangeal joint after flexor hallucis longus tendon transfer for the treatment of Achilles tendinopathy or rupture7,8. In adults, the pathology may be traumatic, inflammatory or degenerative, but the exact pathology is still poorly understood9. The use of flexor hallucis tendon replacement was first demonstrated by Hansen et al in 1991 in a case report in which more than 50% of the Achilles tendon was removed10.
Materials and methods
A retrospective study was conducted in a single center to analyze patients with chronic insertional Achilles tendon pathologies that were non-responsive to conservative treatment for more than four months. Twelve patients were initially identified, but only six met the strict criteria of being above 50 years of age with at least 24 months follow-up and having Chronic Achilles tendon pathology that did not respond to conservative treatment for twelve weeks. A chronic Achilles tendon rupture was defined as a rupture or diagnostic delay of more than six weeks. Four patients had Haglund’s deformity without rupture, and two had a chronic insertional rupture with a pre-existing Haglund’s deformity.
The surgical technique used was a single incision technique, with patients placed in a prone position and a tourniquet applied to the proximal thigh. A longitudinal midline incision was made, and the ends of the Achilles tendon were debrided, removing any degenerative thickened fibers and torn ends. The Haglund deformity was removed by micro saw and completed in a bevelled manner to ensure smooth calcaneus tuberosity without sharp bony prominences. Deep retrocalcaneal tissue was debrided to allow easy visualisation of the tendon, and deep compartment fascia was released to allow the muscle belly of the flexor hallucis to migrate posteriorly.
A calcaneal tunnel was made in the midline around 1-1.5cm anterior to the origin of the insertion of the native Achilles tendon, and the proximal tendon was dissected to allow better excursion as it passed through the tunnel. The debrided Achilles tendon was repaired independently, and if necessary, a two row bone anchor suture was used to secure the tendon in position.
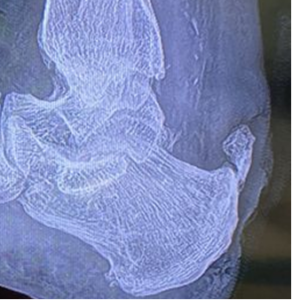
Figure 1. Pre operative radiograph showing a patient with chronic insertional Achilles tendinopathy with large irregular ossification seen within the distal Achilles tendon.

Figure 2. Post operative lateral radiograph shows the smooth superior surface of the calcaneus following Haglund excision and bio-interference screw tunnel exiting in front of the calcaneal tuberosity inferiorly.

Figure 3. Intraoperative photos demonstrating (A) – Identification of flexor hallucis longus tendon deep to the Achilles tendon in a lateral to medial direction. (B) Use of a whipstitch at the terminal end of the flexor hallucis longus tendon to allow easy passage through the calcaneal tunnel. (C) Insertion of the bio interference screw. * Note the approximation of the muscle belly up to the entrance of the calcaneal tunnel to ensure proper tensioning of the tendon. (D) The ankle position is checked intraoperatively. The desired ankle position is comparable to the contralateral resting equinus position of the ankle.
Post Operative Rehabilitation & Protocol
Post-operatively, patients were placed on a rigid below knee equinus plantar slab, which was changed to a thermoplastic splint after wound inspection. They were then changed to an ankle walker boot with a wedge, and physiotherapy was initiated. At four weeks, the wedge was removed, and the ankle was moved to neutral position, allowing full weight bearing. At eight weeks, boots were removed, and active range of motion exercises were initiated to prevent tendon adhesions. From the sixth to twelfth week, active range of motion beyond neutral was encouraged. Passive range of motion was advised only after three months postoperatively.
| Time frame | 4 weeks | Next 4 weeks | Next 4 weeks | After 3rd month | |
| Ankle position | Plantar flexion gravity equinus | Immediately move to neutral and maintain until 8th week
|
Off cast/boot | ||
| Weight bearing | From 2nd week
|
onwards(walker)
|
|||
| Active ROM (up to neutral) | From 2ndweek up to 6th week | ||||
| Active ROM (dorsiflexion beyond neutral) | From 6th week | Till 12th week | |||
| Passive ROM (dorsiflexion beyond neutral) | Allow | ||||
Table 1 – Table illustrating our rehabilitation protocol in our centre for patients following flexor hallucis longus tendon transfer.
Materials & Methods
The study involved 12 patients with chronic insertional Achilles tendinitis who underwent surgery between September 2021 and August 2022. Only 6 patients were included in the study, as the rest did not meet the criteria or were lost to follow up. The patients were male and female, with a mean age of 55 years. Four patients had pre-existing diabetes mellitus and one had hypertension with ischaemic heart disease. Only one patient was a smoker. The average patient weight was 78.16kg. Four patients had Haglund’s deformity without rupture, and two had chronic insertional rupture with a pre-existing Haglund’s deformity. The study was approved by the hospital’s ethics committee and conducted in accordance with the Declaration of Helsinki 1964.
Results
The study involved 12 patients with chronic insertional Achilles tendinitis who underwent surgery between September 2021 and August 2022. Only 6 patients were included in the study, as the rest did not meet the criteria or were lost to follow up. The patients were male and female, with a mean age of 55 years. Four patients had pre-existing diabetes mellitus and one had hypertension with ischaemic heart disease. Only one patient was a smoker. The average patient weight was 78.16kg. Four patients had Haglund’s deformity without rupture, and two had chronic insertional rupture with a pre-existing Haglund’s deformity. The study was approved by the hospital’s ethics committee and conducted in accordance with the Declaration of Helsinki 1964.
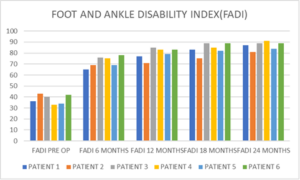
Figure 4. Simple bar chart showing the improvement progress of each patient over time.
The American Orthopedic Foot and Ankle Scale (AOFAS) showed significant improvement in ankle function postoperatively, similar to the Foot and Ankle Disability Index. The initial mean preoperative score was 57, with the most significant improvement occurring in the first six months. After six monthly assessments, the final mean AOFAS scores were 87, indicating moderate improvement in ankle function over the following 18 months.
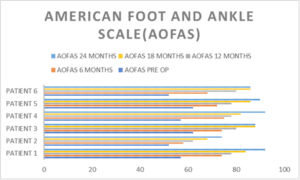
Figure 5. Representation of the AOFAS scores at 6 monthly intervals show peak improvement in scores in the first 6 months following surgery with gradual improvement in scores over the following 18 months.
Visual Analogue Scale
Visual Analogue scale was used to quantify each patients pain preoperatively and overall improvement in pain at 24 months post operatively. There is significant improvement in scores with majority of patients having minimal to moderate pain only at six months following surgery. Most patients have relatively no pain or minimal pain at 1 year with no further worsening of symptoms during the study period as shown in Figure 6.
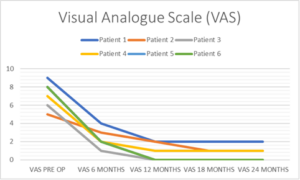
Figure 6. Rapid improvement of symptoms within 6 months of surgery and almost complete resolution of insertional heel pain within a year following surgery.
Range of motion
Range of motion of the ankle was clinically examined and evaluated on follow up. Physiotherapy as part of the accelerated rehabilitation showed good range of motion in all our patients as shown in Figure 7.
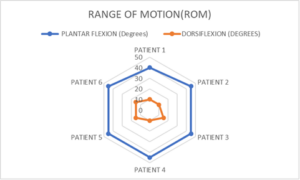
Figure 7. Scatter plot shows the individual patients ankle range of motion following surgery at 24 months.
Complications
They were no major complications observed in our study. They were no complaints of weakness of the great toe during this short term study. However, a longer case study may show a different outcome if any. No major complications such as wound breakdown or deep vein thrombosis or re-rupture was observed in our study however with a small sample size, this may need to be evaluated further in a larger series.
Discussion
Chronic insertional Achilles tendinopathy and ruptures are common foot and ankle pathologies, with the optimal surgical treatment for elderly patients being challenging due to degeneration of the insertion of the Achilles tendon. The treatment of choice depends on the size of the gap following tendon debridement, such as end-to-end repair, V-Y advancement, and tendon transfers. Tendon transfers such as flexor hallucis longus tendon transfers, flexor digitorum longus tendon transfers, peroneus brevis tendon transfers, and free gracilis tendon grafts have been described.
The flexor hallucis longus tendon has length, strength, and durability, acting synergistically with the Achilles tendon for plantar flexion during gait. The proximity of the vascularized muscle belly of the flexor hallucis tendon to the injured Achilles tendon may result in its repair and reintegration over time. This study demonstrated that single incision and short tendon harvest of the flexor hallucis longus tendon and fixation with a bone interference screw can be performed with a small skin incision with relatively low morbidity, especially in elderly patients with co-morbidities where bone quality and wound healing are a potential issue.
The study showed significant improved FADI and AOFAS scores in the first six months following surgery and continued gradual improvement up to 24 months post-operatively. The visual analogue scale also showed marked improvement with minimal pain and discomfort within a year of surgery. However, concerns about flexor hallucis longus tendon transfer may cause weakness of plantar flexion of the hallux, especially in younger, more active sportsmen but not in daily living activities. In elderly patients with keen early functional recovery, flexor hallucis longus tendon transfer may be an appropriate method of treatment.
Conclusion
Single incision with a short harvest flexor hallucis tendon transfer is a safe and reliable procedure for elderly patients with co-morbidities allowing good functional outcome, early return to activities of daily living and validation of the outcome with good ankle scores. However, further studies with larger sample study size with and longer follow-up duration will be more beneficial.
References
- C. Hong et al. Anatomic Basis for Minimally Invasive Flexor Hallucis Longus Transfer in Chronic Achilles Tendon Rupture The Journal of Foot & Ankle Surgery 57 (2018) 938–941
- Nestorson J, Movin T, Moller M, Karlsson J. Function after Achilles tendon rupture in the elderly:25 patients older than 65 years followed for 3 years. Acta Orthop Scand 71:64–68, 2000
- Maffulli N, Ajis A, Longo UG, Denaro V. Chronic rupture of tendo Achillis. Foot Ankle Clin N Am 12:583–596, 2007. Padanilam TG. Chronic Achilles tendon ruptures. Foot Ankle Clin 14:711–728,
- Wapner KL, Pavlock GS, Hecht PJ, Naselli F, Walther R. Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot Ankle 14:443–449,1993
- Silver RL, de la Garza J, Rang M. The myth of muscle balance: a study of relative strengths and excursions of normal muscles about the foot and ankle. J Bone Joint Surg Br 67:432–437, 1985
- Young A, Redfern DJ. Simple method of local harvest and fixation of FHL in Achilles tendon reconstruction: technique tip. Foot Ankle Int 29:1148–1150, 2008
- Coull R, Flavin R, Stephens MM. Flexor hallucis longus transfer: evaluation of postoperative morbidity. Foot Ankle Int 2003;24(12):931–4.
- Irwin TA. Current concepts review: insertional Achilles tendinopathy. Foot Ankle Int 2010;31(10):933–9.
- Hansen ST. Trauma to the heel cord. In: Jahss MH, ed. Disorders of the Foot and Ankle. Vol 2. Philadelphia, PA: W B Saunders; 1991:2357.
- Maffulli N, Longo UG, Kadakia A, Spiezia F. Achilles tendinopathy [published online April 18,2019]. Foot Ankle Surg. Doi:10.1016/j.fas2019.03.009
- Lee J, Williams C, Lowrey C, Gould G, Markert R, Laughlin R : Flexor Hallucis Longus tendon Transfer Fixation – A biomechanical analysis of the effects of a terminal whipstitch and bone tunnel length; Foot Ankle Surg Vol10/no.1 : DOI: 10.1177/1938640016666917
- Martin RL, Burdett RG, Irrgang JJ. Development of the Foot and Ankle Disability Index (FADI) [abstract] J Orthop Sports Phy Ther: 1999;29:A32-33
- Mahajan RH, Dalal RB. Flexor hallucis longus tendon transfer for reconstruction of chronically ruptured Achilles tendons. J Orthop Surg 2009;17(August (2)):194–8.
- Hahn F, Meyer P, Maiwald C, Zanetti M, Vienne P. Treatment of chronic Achilles tendinopathy and ruptures with flexor hallucis tendon transfer: clinical outcome and MRI findings. Foot Ankle Int 2008
- Mann RA, Holmes GB Jr, Seale KS, et al. Chronic rupture of the Achilles tendon: a new technique of repair. J Bone Joint Surg Am. 1991;73:214–219
- Myerson MS. Achilles tendon ruptures. Instr Course Lect. 1999;48:219–230
- Maffulli N, Spiezia F, Testa V, et al. Free gracilis tendon graft for reconstruction of chronic tears of the Achilles tendon.J Bone Joint Surg Am. 2012;94:906–910
- Mann RA, Holmes GB Jr, Seale KS, et al. Chronic rupture of the Achilles tendon: a new technique of repair. J Bone Joint Surg Am. 1991;73:214–219
- Wegrzyn J, Luciani JF, Philippot R, Brunet-Guedj E, Moyen B, Besse JL. Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int Orthop 2010;34(December (8)):1187–92.
- Yeoman TF, Brown MJ, Pillai A. Early post-operative results of neglected tendo Achilles rupture reconstruction using short flexor hallucis longus tendon transfer: a prospective review. Foot (Edinb) 2012;22(September (3)):219–23.
- Oksanen MM, Haapasalo HH, Elo PP, Laine HJ: Hypertrophy of the flexor hallicus longus muscle after tendon transfer in patients with chronic Achilles tendon rupture. Foot and Ankle Surgery 20(2014)253-257
- Hahn F, Meyer P, Maiwald C, Zanetti M, Vienne P. Treatment of chronic Achilles tendinopathy and ruptures with flexor hallucis tendon transfer: clinical outcome and MRI findings. Foot Ankle Int 2008.
- Abdellatif NM, Batista JP: Outcomes of Percutaneous Achilles repair compared with endoscopic flexor hallucis longus tendon transfer to treat Achilles tendon rupture; Foot & Ankle International 2022, Vol. 43(9) 1174-1184
- Yassin M, Gupta V, Martins A; Patient reported outcomes and satisfaction following single incision flexor hallucis longus (FHL) augmentation for chronic Achilles tendon pathologies: Journal of Clinical Orthopaedics and Trauma 23 (2021) 101650
- Koh D, Lim J, Chen JY, Singh R, Koo K; Flexor Hallucis longus tendon transfer versus turndown flaps augmented with flexor hallucis longus transfer in the repair of chronic achilles tendon rupture. Foot and Ankle Surg 25(2019)221-225
- Singh MS, Harna B, Singh S, Vishwakarma : Evaluation of Flexor Hallucis tendon transfer in chronic insertional Achilles tendinopathy in 50-year old population using validated ankles score. The Foot 54(2023)101969
- Hunt KJ, Cohen BE, Davis WH, Anderson RB, Jones CP. Surgical treatment of insertional Achilles tendinopathy with or without flexor hallucis longus tendon transfer: a prospective, randomized study. Foot Ankle Int 2015;36(9):998–1005.
- Maffulli N, Ziello S, Maisto G, Migliorini, Oliva F; Local tendon transfers for chronic ruptures of the Achilles tendon : A systematic review; J. Clin. Med 2023, 12 707.