Publication Information
ISSN 2691-8803
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2019
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
Knowledge and Attitudes of Mental Health Professionals towards Oral Care of Patients in Zimbabwe
Timothy Chifamba1*, Cleopatra Matanhire-Zihanzu1, Constance Viki1, Anesu Chinoperekwei2, Chido Rwafa2, Patience Monde1, Tatenda Vaidah Muzaeni1, Lous Nyasha Dhoro3, David Saunyama4
1Zimbabwe Dental Association, Harare, Zimbabwe
2Zimbabwe College of Psychiatrists, Harare, Zimbabwe
3Private Biostatistician, Harare, Zimbabwe
4Private Researcher, Harare, Zimbabwe
Received Date: August 12, 2022; Accepted Date: August 17, 2022; Published Date: August 23, 2022;
*Corresponding author: Timothy Chifamba. Oral Health for Mental Health Project, Zimbabwe Dental Association, Address: 17 Tweed Road, Eastlea, Harare, Zimbabwe, Telephone: +263 78 542 6701. Email: tchifg@gmail.com
Citation: Chifamba T, Matanhire-Zihanzu C, Viki C, Chinoperekwei A, Rwafa A, et al. (2022) Knowledge and Attitudes of Mental Health Professionals Towards Oral Care of Patients in Zimbabwe. Adv Pub Health Com Trop Med: APCTM-158.
DOI: 10.37722/APHCTM.2022401
Abstract
Objective
This study aimed to assess the oral healthcare knowledge, attitudes, and practices among mental health professionals in Zimbabwe. There are numerous dental conditions associated with mental health conditions. It is, therefore, necessary to assess if mental health professionals are prepared to adequately manage and refer such cases where indicated.
Methods
This was a descriptive cross-sectional study using convenience sampling to collect data using an online questionnaire administered to mental health professionals from the ten provinces of Zimbabwe. The target sample size was 82. Responses to each of the items in the knowledge and attitudes section were graded on a scale of 0 to 3. Descriptive statistics were performed. Composite scores were computed for knowledge and attitudes with the highest possible score for knowledge being 27 and the highest possible score for attitudes being 12. Open-ended responses in the knowledge section were manually analyzed and used to supplement findings from the closed-ended sections.
Results
There were 71 respondents. 60.6% were females, the average (mean) age was 38.78, and the highest reported (mode) working experience was one year.
The overall composite score for knowledge was 14.37 out of 27 (53.2%) and the overall composite score for attitudes was 7.66 out of 12 (63.3%).
The open-ended section addressing practices revealed that only 1.4% of the respondents had received formal oral healthcare-related training. The rest of the respondents indicated they had no training or did not answer this question. Most respondents are not confident in handling oral health complications and several do not know the appropriate referral pathway. There were suggestions for further training and an increased interdisciplinary approach where oral health professionals work alongside mental health professionals.
Conclusion
While the knowledge and attitudes regarding oral care are average amongst Zimbabwean mental health professionals, the practices remain below ideal. There is a need for increased training and a multidisciplinary approach. The formulation of a manual for oral care of mental health patients in the Zimbabwean context is also recommended.
Keywords: Health Promotion; Interdisciplinary Approach; Mental Health Professionals; Oral Health
Introduction
A bi-directional relationship exists between mental health and oral health. Dental care rendered by Oral Health Professionals is associated with raised anxiety and fear [1-3]. On the other hand, individuals with mental health conditions are at increased risk for negative oral health outcomes [4-8]. Globally, the prevalence of mental health conditions has risen sharply [9]. Globally there are thirteen mental health workers per 100,000 people whilst in low- to middle-income countries, this falls to two per 100,000 people [10]. The Mental health needs in the African Region are significant, 70% of suicides occur in low- to middle-income countries and yet a severe shortage of professional mental health workers persists [11]. As of 2020, 13 registered psychiatrists were practising in Zimbabwe, thus resulting in a doctor-population ratio of 0.1 per 1000. The mental nurse-to-population ratio stood at 1.3 nurses per 1000. As a result, mental health professionals are overworked as they are few and yet have to cater to a population of 15 million Zimbabweans [12].
The Strategic Plan for Mental Health Services in Zimbabwe calls for a multi-disciplinary, inter-sectoral approach to solving the challenges faced by persons living with mental health conditions [13]. This is in harmony with the sustainable development goals 3,4 and 10 which promote good health, human dignity and equality for all persons inclusive of persons with mental, intellectual, and psychosocial disabilities, and the reduction of inequality [14]. Oral health disease and mental health conditions lead to reduced quality of life in patients [15,16]. Ideally, dental and mental professionals should readily recognize, manage, and refer persons with reciprocity where necessary. This study sought to describe the knowledge, attitudes, and practices of Zimbabwean mental health professionals concerning the oral care of persons living with mental health conditions. It evaluated the standard of oral health care provision by mental health professionals in Zimbabwe and assessed attitudes mental health professionals possess regarding the management of patients presenting with oral health conditions.
Methods
Study Area and Period
A cross-sectional study was conducted at the national level. Mental health professionals from all ten provinces of Zimbabwe were targeted through an online google forms survey. Data was collected over two weeks.
Sampling Technique
The convenience sampling technique was employed, and the invitation to participate in the study was sent to mental health professionals through contacts from a database of mental health workers obtained from the Ministry of Health and Childcare Mental Health Directorate. The targeted population was assumed to have all the required expertise and knowledge to participate in the study.
Study Population
All health professionals that are primarily associated with handling and offering services to Mental Health patients in Zimbabwe were targeted. The study sought to assess their knowledge, attitudes and practices concerning the oral health care of Mental Health patients.
Inclusion and Exclusion Criteria
The study only included health professionals that have a direct service to Mental Health patients and all that have a service that influences the well-being of the patients. The survey excluded those professionals in the Health industry who do not have a direct or indirect influence on the well-being of Mental Health patients.
Sample size determination
According to information obtained from the Ministry of Health and Childcare, there were 553 Mental Health Professionals (13 Psychiatrists, 48 Medical Doctors, 486 psychiatric nurses and 6 psychologists) working in public mental health institutions in Zimbabwe at the time of the study. Based on Slovin’s formula with a confidence level of 95% and a 10% margin of error, the target sample size was 82 mental health professionals. However, the actual size reached saturation when the study was conducted and 71 mental health professionals participated.
Data Collection Tools, Methods and Data Quality Assurance
A questionnaire was designed based on an extensive review of the literature. It was divided into four sections. The first section focused on sociodemographic details, while the following two focused on the knowledge and attitudes regarding the oral care of mental health patients. Questions on these two sections were on a five-point Likert scale. The final section of the questionnaire focused on the practices regarding oral care of mental health patients. This section consisted of open-ended questions. To ensure validity, the constructed questionnaire was reviewed by research members from both the dental and mental health professions. To ensure reliability, a pilot study among 25 mental health professionals was carried out and Cronbach’s Analysis was conducted. Two questions that were inconsistent one from the knowledge section and another from attitudes were excluded from the final research instrument used to carry out the national survey.
Data Analysis
Questions from the two sections Knowledge and Attitudes were given marking scores for each response ranging from 3,2,1,0 as per the level of correctness of the response. The most correct response was given a level of three (3) point score and the next level scores were two (2) points and one (1). Zero (0) points were awarded for an extreme wrong and also for the “I don’t know” response e.g. cleaning the oral cavity of patients is a disgusting task?
Response
Score Attributed
I don’t know
0
Agree
1
Strongly Agree
0
Disagree
2
Strongly Disagree
3
The Attitude section had 4 questions which were considered so a maximum score that a participant would score was 12 and the Knowledge section had 9 questions considered with a total of 27 points that a participant could gain. Scores for each participant on Knowledge and Attitudes were then gathered and descriptive statistics were performed using SPSS 23. The open-ended answers were assessed and themes were drawn from the responses of the respondents. The findings from this section were used to supplement the findings from the close-ended section in the discussion of findings.
Ethics
Ethical Clearance was obtained from the Medical Research Council of Zimbabwe (MRCZ/A/2723). Informed consent was obtained from study participants and the identity of respondents was kept anonymous. Participation in the survey was entirely voluntary and the right to withdraw or chose not to participate without any consequences was spelt out to participants.
Results
Demographics
The distribution of professionals who participated in the study is shown in Figure 1 below. Psychiatric Nurses and Psychiatrists are the participants which showed much dominance with an average of 21 respondents and 17 respondents, respectively.
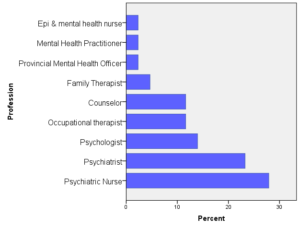
Figure 1: Distribution of Professions of Respondents.
In terms of the gender distribution, there were 28 (39.4%) Male and 43 (60.6%) Female respondents. Figure 2 shows the age distribution of respondents. The age range of 35-40 had more professionals than the other age range groups.
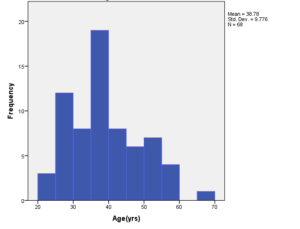 Figure 2: Age Distribution of Respondents.
Figure 2: Age Distribution of Respondents.
The work experience of the mental health professionals who participated in the study is presented in Figure 3. Zero years of experience implies that the mental health professionals had less than a year in the field. The highest reported working experience was a one-year working experience (18%).
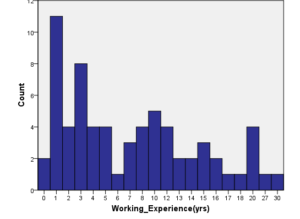
Figure 3: Years of Work Experience in Mental Health amongst respondents.
Knowledge Regarding Oral Care of Mental Health Patients
Responses were graded based on the scoring system shown in Table 1 (see methods section), in which the highest attainable score for each question is three and the lowest possible mark is zero. The mean scores of responses to each question are presented below:
Question
Mean score
Std
Dental care rendered by oral health professionals is associated with raised anxiety
1.403
1.009
Individuals with mental health conditions are at increased risk for negative oral health outcomes
1.821
0.976
Periodontitis is a common dental condition amongst mentally ill patients that affects the gums and tooth-supporting soft tissue
1.398
1.113
Xerostomia, drying of the mouth, is common predisposing to rampant caries
1.485
1.036
Poor nutrition may result from problems in the oral region
1.794
0.9
Maxillofacial injuries are injuries to the jaws and facial region that are to be referred for management by professional dental staff.
2.132
0.999
There is only one correct technique for toothbrushing
1.691
0.879
Pregnant women require extra oral health
1.529
0.931
Different patients require different types of toothbrushes
1.821
0.88
To measure the overall knowledge regarding oral and maxillofacial care, responses to each of the questions were summed up. The maximum achievable score for knowledge regarding oral and maxillofacial care of mental health patients was 27 points. The overall knowledge score is presented in Table 3. This score translates to 53.2% knowledge regarding oral and maxillofacial care.
N
Minimum
Maximum
Mean
Std. Deviation
Knowledge
71
0
27
14.37
5.642
Attitudes Regarding Oral Care of Mental Health Patients
Responses were graded based on the scoring system shown in Table 1 (see Methods section), the highest score on each item was three and the lowest possible score was zero. The mean score of responses to individual items in the attitudes section of the questionnaire is presented in Table 4.
Question (Attitudes)
Mean score
Std
Cleaning the oral cavity of patients is a disgusting task
1.824
1.070
Cleaning the oral cavity of hospitalized patients is essential
2.397
0.926
Cleaning the oral cavity of patients is a time-consuming task
1.627
0.99
There are more important tasks than cleaning the oral cavity of patients
2.176
0.785
To measure the overall attitudes regarding oral and maxillofacial care, responses to each of the questions were summed up. The maximum achievable score for attitudes regarding oral and maxillofacial care of mental health patients was 12 points. The findings are presented in Table 5. This translates to a 63.3% score in terms of attitudes regarding Oral and Maxillofacial Care.
N
Minimum
Maximum
Mean
Std. Deviation
Attitudes
71
0
12
7.66
2.787
Practices Regarding Oral Care of Mental Health Patients
The responses from the open-ended section of the questionnaire which probed into the practices of mental health professionals regarding oral care of their patients revealed that almost all the professionals would refer a patient with a toothache or related oral health problem to the dentist. Only one out of 71 professionals who answered the questionnaire reported to have received dental-related training for about six months, the rest had a no answer to this question. In terms of handling oral health problems which are common to mental health patients, 10% of the professionals had some idea of handling a drooling tooth, 35% did not know what to do with such patients and the other 55% responded that they would refer to a dentist. Among respondents who said they would the patient to a dentist, some indicated they would first need to determine the cause of the drooling before referral. When asked for suggestions, professionals’ brought out ideas that push for more training and workshops for them that would increase knowledge and confidence in handling oral conditions. Some suggested that a dental unit be placed near their facilities to improve ease of access to dental care.
Discussion
The study revealed that mental health professionals possess average (53.2%) knowledge regarding oral and maxillofacial care. This is better than expected, considering that only 1.4% of the respondents indicated that they had received training related to the provision of oral health. This is in contrast to the findings of a cross-sectional study carried out in Australia where it was found that 39% of mental health support workers had received training in oral health in the previous twelve months [17]. However, this finding is in harmony with the findings of Ashour [18] who examined the knowledge, attitudes, and practices of oral health care among Nursing staff in Saudi Arabia and concluded that there is a need for formal training of mental health professionals with regards to oral health provision. While the overall knowledge is average, an analysis of the findings reveals that there was great variance in the degrees of knowledge regarding different areas of oral health. Knowledge regarding the incidence of maxillofacial fractures and the need for referral was high. However, knowledge related to the occurrence of periodontitis amongst mental health patients, the association between dental care and anxiety, and the association between xerostomia and caries was below average. The lack of knowledge in these areas may make it difficult for mental health professionals to prioritize the provision of oral care amongst their patients [19].
The study revealed that mental health professionals possess average (63.3%) attitudes regarding oral care of mental health patients. A notable number of respondents viewed cleaning the oral cavity as a time-consuming and disgusting task. This is supported by the findings of Scrine, Durey, and Slack-Smith [20] who reported a reluctance amongst mental health professionals when it came to raising oral health issues. This may be due to limited training regarding oral care which has been demonstrated to create negative perceptions of oral care amongst healthcare workers, thus hindering collaboration between healthcare workers and dental professionals [21]. The same study also found that there were generally less positive perceptions amongst health care workers, other than dental professionals, regarding performing a thorough cleaning of the oral cavity using dental care products such as floss and interdental brushes. The general perception was that these are specialized tools designated for use by dental professionals and not healthcare workers from other fields. Attitudes and perceptions regarding oral healthcare have been demonstrated to improve with increased dental education [22]. The researchers hypothesize that the average attitudes regarding oral care found amongst mental health professionals can be improved by oral healthcare education programs targeted at mental health professionals.
In terms of practices regarding oral health, the findings indicate that most mental health professionals do not have the requisite training when it comes to the provision of oral care. Furthermore, most of them do not have an idea of how to handle basic oral health problems. Almost half of them (45%) do not know the proper referral pathway for referring a patient with oral and maxillofacial problems. Given the average knowledge and attitudes regarding oral care of patients, the researchers hypothesize that the less than ideal practices with regards to oral healthcare of patients may due to limited knowledge. This is supported by findings from Göstemeye, Baker, and Schwendicke who found that the barriers to adequate oral healthcare provision by healthcare professionals include lack of knowledge, lack of oral health training, and patients refusing oral care [23]. The absence of structured guidelines regarding the oral care to be provided to mental health patients may also contribute to the practices that fall below ideal. In a study that assessed the oral healthcare provision by prenatal care professionals, it has been concluded that while knowledge regarding oral health may be adequate, in the absence of best practice guidelines and frameworks to ensure that they are implemented, the practice of oral care of patients may remain below ideal [24].
Conclusions
The findings of this study suggest that there is a need for collaboration between oral health and mental health professionals. Meaningful interdisciplinary training programs need to be coordinated where mental health professionals are trained in the provision of oral and maxillofacial care, this will increase confidence in handling patients presenting with basic oral health needs and also ensure that all are aware of when to refer, how to refer, and to whom to refer a patient requiring specialized oral health care. There is a need for the formulation of a manual including best practice guidelines to ensure that the oral care of mental health patients is carried out in harmony with international best practices.
Funding: The project has been made possible thanks to a grant from the FDI World Dental Development Fund.
Conflict of Interest: The authors declare that they have no undisclosed competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements: The authors thank all mental health professionals who participated in the survey.
The authors would like to thank the following partners for making this research possible: Zimbabwe Dental Association, Zimbabwe College of Psychiatrists, Ministry of Health and Child Care – Oral health and Mental health Directorates, University of Zimbabwe Dentistry and Psychiatry Departments, Zimbabwe Dental Therapists Association (ZIDETHA), Zimbabwe Dental Students Association (ZIDSA), Zimbabwe Academy of Dental Nurses (ZADENU), Dental Surgery Assistants Association, Zimbabwe Mental Health Nurses Network, Zimbabwe Life Project.
References
- Soares F, Souto G, Lofrano M, Colares V (2015). Anxiety related to dental care in children and adolescents in a low-income Brazilian community. European Archives of Paediatric Dentistry. 16:149-152.
- Tellez M, Kinner D, Heimberg R, Lim S, Ismail A (2014). Prevalence and correlates of dental anxiety in patients seeking dental care. Community Dentistry and Oral Epidemiology. 43:135-142.
- Seligman L, Hovey J, Chacon K, Ollendick T (2017). Dental anxiety: An understudied problem in youth. Clinical Psychology Review. 55:25-40.
- Kisely S (2016). No Mental Health without Oral Health. The Canadian Journal of Psychiatry. 61:277-282.
- Kisely S, Sawyer E, Siskind D, Lalloo R (2016). The oral health of people with anxiety and depressive disorders – a systematic review and meta-analysis. Journal of Affective Disorders. 200:119-132.
- Kisely S, Baghaie H, Lalloo R, Siskind D, Johnson N (2015). A Systematic Review and Meta-Analysis of the Association Between Poor Oral Health and Severe Mental Illness. Psychosomatic Medicine. 77:83-92.
- Gupta S, PK P, Gupta R (2016). Necessity of oral health intervention in schizophrenic patients – A review. Nepal Journal of Epidemiology. 6:605-612.
- Qiao Y, Shi H, Wang H, Wang M, Chen F (2020). Oral Health Status of Chinese Children with Autism Spectrum Disorders. Frontiers in Psychiatry. 11.
- Nochaiwong S, Ruengorn C, Thavorn K, Hutton B, Awiphan R, Phosuya C, et al. (2021). The global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Scientific Reports. 11(1).
- World Health Organization (2021). Mental Health Atlas. Geneva: World Health Organization.
- World Health Organization (2019). Suicide in the world: Global Health Estimates. Geneva: World Health Organization.
- Mangezi W (2020). A Letter from Zimbabwe. The Lancet Psychiatry. 7(5):394.
- Ministry of Health and Childcare. National Strategic Plan for Mental Health Services 2019 – 2023: Towards Quality of Care in Mental Health Services. Harare: Ministry of Health and Childcare; 2020.
- United Nations. Transforming our World: The 2030 Agenda for Sustainable Development. New York: United Nations; 2015.
- Baiju R (2017). Oral Health and Quality of Life: Current Concepts. Journal of Clinical and Diagnostic Research.
- Choo C, Chew P, Ho C, Ho R (2019). Quality of Life in Patients with a Major Mental Disorder in Singapore. Frontiers in Psychiatry. 9.
- McGrath R, Marino R, Satur J (2021). Oral health promotion practices of Australian community mental health professionals: a cross-sectional web-based survey. BMC Oral Health. 21(1).
- Ashour A (2020). Knowledge, Attitudes and Practices Regarding Oral Health and Oral Care Among Nursing Staff at a Mental Health Hospital in Taif, Saudi Arabia: A Questionnaire-based Study. Journal of Advanced Oral Research. 11:34-44.
- Edward K, Felstead B, Mahoney A (2011). Hospitalized mental health patients and oral health. Journal of Psychiatric and Mental Health Nursing. 19:419-425.
- Scrine C, Durey A, Slack-Smith L (2017). Enhancing oral health for better mental health: Exploring the views of mental health professionals. International Journal of Mental Health Nursing. 27:178-186.
- Haresaku S, Aoki H, Kubota K, Monji M, Miyoshi M, Machishima K, et al. (2020). Comparison of perceptions, attitudes and performance regarding collaborative oral health care among healthcare workers. International Dental Journal. 70:462-468.
- Haresaku S, Umezaki Y, Egashira R, Naito T, Kubota K, Iino H, et al. (2021). Comparison of attitudes, awareness, and perceptions regarding oral healthcare between dental and nursing students before and after oral healthcare education. BMC Oral Health. 21(1).
- Göstemeyer G, Baker S, Schwendicke F (2019). Barriers and facilitators for provision of oral health care in dependent older people: a systematic review. Clinical Oral Investigations. 23:979-993.
- Hoerler S, Jenkins S, Assad D (2019). Evaluating Oral Health in Pregnant Women: Knowledge, attitudes and practices of health professionals. Journal of Dental Hygiene. 93:16-22.