Publication Information
ISSN: 2641-6859
Frequency: Continuous
Format: PDF and HTML
Versions: Online (Open Access)
Year first Published: 2018
Language: English
| Journal Menu |
| Editorial Board |
| Reviewer Board |
| Articles |
| Open Access |
| Special Issue Proposals |
| Guidelines for Authors |
| Guidelines for Editors |
| Guidelines for Reviewers |
| Membership |
| Fee and Guidelines |
 |
25-OH-VitaminD3 Level in Elite Sports: Is high-Dose Vitamin D Supplementation Effective In Preventing Muscle Damage and Infections?
Klaus Erpenbach1*, Max C. Erpenbach1, Wolfgang Mayer2, Uwe Hoffmann3, Stefan Mücke1
1Institut für medizinische Leistungsoptimierung und Trainingssteuerung, Marienstraße 1, 50374 Erftstadt, Germany
2Lab4more GmbH Bavariahaus, Augustenstraße 10, 80333 München, Germany
3Deutsche Sporthochschule Köln, Am Sportpark Müngersdorf 6, 50933 Köln, Germany
Received Date: February 26, 2021; Accepted Date: March 09, 2021; Published Date: March 22, 2021
*Corresponding author: Klaus Erpenbach, Institut für medizinische Leistungsoptimierung und Trainingssteuerung, Marienstraße 1, 50374 Erftstadt, Germany. Email: info@im-lot.org
Citation: Erpenbach K, Erpenbach MC, Mayer W, Hoffmann U, Mücke S (2021) 25-OH-VitaminD3 Level in Elite Sports: Is high-Dose Vitamin D Supplementation Effective In Preventing Muscle Damage and Infections?Adv Ortho and Sprts Med: AOASM-137.
Summary
Muscle damage as well as recurrent and serious infections especially to the end of the playing period in team sport or to the end of preparation for competition in endurance or single sport is the most common symptom in elite sport demolishing optimal training results. Is a vitamin D deficiency responsible for these symptoms in elite sports and a high-dose vitamin D supplementation able to prevent these symptoms by reaching the upper standard blood level of vitamin D?
Methods:
In 111 elite athletes [male: 50 – female: 61 / soccer: 21 – field hockey: 62 – Olympics: 19 – tennis: 5 – motorsports (DTM-Formula1): 4] blood vitamin D were determined. In all elite athletes the symptoms muscle damage and infections were correlated. 25 athletes were substituted with daily dose of 20000 IU 25(OH) vitaminD3 for 3 months. The vitamin D blood level was determined before and after supplementation and correlated with the symptoms of recurrent infections and muscle injury. A Spearman-ranking coefficient of correlation, a chi-quadrat-test (²-Test) by Pearson and an independent t-test were used. p < 0,05 was supposed to be significant, p < 0,01 highly significant.
Results:
In 51.3% of all elite athletes (N=57/111) a vitamin D-deficiency (< 30 ng/ml) was established. In cases of young player (< 18) compared to national A player vitamin D significantly were poorly supplied [vitamin D: 25,71 ± 9,58 ng/ml vs. 35,87 ± 12,35 ng/ml (p=0,007)]. Muscle damages (in 73% of all cases) significantly occurred in vitamin D deficiency [29,13 ± 9,38 ng/dl vs. 36,27 ± 12,09 ng/dl, p=0,005] more frequently. Comparing the settings of vitamin D < 40 ng/ml vs. > 40ng/ml [27,50 ± 7,85 ng/ml vs. 46,31 ± 6,71 ng/ml, OR=4,53, p=0,007] muscle damage were observed 4,53 times more frequent in the lower group. No significances were observed in infection. By the daily substitution of 20000 IU 25(OH) vitaminD3 the vitamin D blood level was significantly increased (20,68 ± 12,29 ng/ml before vs. 76,41 ± 25,36 ng/ml after therapy, p=0,0001). Regarding recurrent infections an absolute risk reduction of 48% (13/25 before vs. 2/25 after therapy, p=n.s) and muscular injuries of 68% (18/25 before vs 1/25 after therapy, p=0,066) was achieved. No toxicities have been observed.
Conclusion:
Independently to the type of sports deficiency of vitamin D in elite sports was observed. Vitamin D plays an important and significant role in preventing muscle damages. Further RCT studies reaching a 25(OH)-vitaminD3 level of 70-80 ng/ml for a whole season are necessary to demonstrate efficacy in preventing muscle damages and recurrent infections in elite athletes.
Introduction
Micronutrients - vitamins and trace elements – interact with each other, are essential and needed daily to maintain all physiological body functions optimally [1-2]. High training effort, a tight schedule, unbalanced or incorrect nutrition, frequent travel and high psychological stress lead to a high consumption of these micronutrients during preparation, which ends in injuries in 12.9% of cases and in acute infections in 9.2% of cases, leading to training interruptions and competition cancellations [3-6]. At major events such as the Olympics, the FIFA World Cup or the IAAF, 9.6-14% of participants are absent due to injury [5-13]. Twice as often in winter as in summer, 5.4-8.9% of participants suffer from an acute infectious disease [5-13]. The most common acute infections occur in the upper respiratory tract (46%), 25% in the urogenital system, followed by 21% with gastrointestinal infections and 8% skin infections [5-13]. These losses could not be reduced by the "General guidelines for illness prevention in athletes" of the Olympic Committee [14].
Vitamin D is an essential, fat-soluble vitamin and acts as a precursor hormone for many metabolic and biological processes and regulates the expression of over 900 different genes [18]. These genes have a wide range of effects on health and performance in sport: such as exercise-induced inflammation, carbohydrate metabolism, cardiovascular health, bone and skeletal muscle metabolism [15-17, 19-22]. Athletes with vitamin D deficiency have an increased risk of bone/joint wear or fractures [23-25] as well as catabolic effects on the muscle that result in muscle fatigue or tear [26, 27].
The aim of this study is to evaluate the 25-OH vitamin D3 status of top athletes in various sports and to identify possible correlations with the complaints of susceptibility to infections and muscle injuries of the athletes as well as the efficacy of high-dose 25(OH) VitaminD3 substitution in preventing these symptoms. Are there clear differences between vitamin D deficiency and the athletes' complaints?
Methods
Participants
111 top athletes from various sports (team sports: field hockey and soccer - individual sports: athletics, tennis, motorsports) included in the study for performance optimization. All participants gave their written consent and were evaluated using a questionnaire for medically confirmed muscle injuries and susceptibility to infections. Muscle injuries included all muscle fibre tears, muscle bundle tears and tendon-muscle tears. Susceptibility to infection was defined as at least 2 viral and/or bacterial infections (upper respiratory tract infections, gastrointestinal infections, urinary tract infections) or more per year. In all athletes, 25-OH vitamin D3 in the blood was examined and correlated with the symptoms. In addition, 25 elite athletes were substituted with a daily dose of 20000 IU 25(OH) vitaminD3 for 3 month, blood vitaminD was determined before and after therapy and correlated with symptoms of recurrent infection and muscle injury.
Vitamin D 25-OH (serum)
The quantitative determination of total 25-OH vitamin D in serum was carried out according to the manufacturer's instructions by using a direct competitive chemiluminescence immunoassay (CLIA) on the Liasion-XL laboratory machine from Diasorin, Dietzenbach, Germany (Order No. 310600).
Statistical Analysis
The data was statistically analyzed using IBM®SPSS® software 25. Spearman Rho was used to calculate the correlation between the different parameters. A Chi-square (²- ) 4-field test according to Pearson was used for the frequency comparison between symptoms and age groups and the odds ratio (OR) was calculated. The 95% confidence interval (CI) was calculated according to.
For 2-group mean comparisons, a level test was performed to check variance homogeneity, followed by an independent T-test for homogeneous (P > 0.1) or in homogeneous variances with two-sided questioning. For k > 2 groups or for combined influences of the different patient groups and the respective symptoms, a one - or two - factorial analysis of variance (ANOVA) was applied. Post-hoc mean value equivalence was performed with the two-sided Sidak test.
For p ≤ 0.05 the results were considered significant, for p ≤ 0.01 highly significant.
Results
(Table 1) shows the characteristics of the study population. 73% of all top athletes complained about muscle injuries and 40% about infections. Young national players U16-U18 suffered significantly more frequent muscle injuries than the A-national players [86% (18/21) vs. 67% (18/27) - OR = 3.00; 95%CI: 1.50 - 4.50, p=0.022]. No differences were found for infections. The vitamin D value of 51.3% (57/111) of the athletes was < 30 ng/ml, with 13.5% (15/111) showing a vitamin D deficiency (< 20 ng/ml) and 37.8% (42/111) an in-adequate vitamin D supply (> 20-30 ng/ml).
(Table 2) shows the comparison of youth vs. adults. Compared to adults, adolescents are significantly worse supplied with vitamin D. For vitamin D (25.71 ± 9.58 ng/ml vs. 35.78 ± 12.35 ng/ml - p=0.007) (Table 2) the youth players are significantly worse supplied compared to the A-national players. The proportion of youth players with a deficiency or inadequate vitamin D supply was 64.4% (29/45), with 22.2% (10/45) youth players showing a vitamin D deficiency (< 20 ng/ml) and 42.4% (19/45) an inadequate vitamin D supply (20-30 ng/ml). Compared to the adults, youth players thus have a 2.46 times higher risk of developing a vitamin D deficiency (29/45 vs. 28/66, OR = 2.46, 95%CI: 1.67 - 3.24, p < 0.023).
(Table 3) shows the values of the athletes in the group comparison divided into groups below and above international recommendations of 40 ng/ml (15, 28-31) with reference to the symptoms. A muscle injury seems more likely to occur with a deficiency of 25-OH vitamin D3 (p = 0.007). No effects on infections are apparent.
The daily administration of 20000 IU 25(OH)VitaminD3 (each 10000 IU in the morning and evening) significantly increased the blood vitaminD (20,68 ± 12,29 ng/ml before vs. 76,41 ± 25,36 ng/ml after therapy, p=0.0001) (Figure 1) and with regard recurrent infections, an absolute risk reduction of 48% (13/25 before vs. 2/25 after therapy, p=n.s) and muscular injuries of 68% (18/25 before vs 1/25 after therapy, p=0.066) was achieved (Tabble 4). No toxicities (hypercalcaemia) have been observed. The athlete, who still suffered from muscular injury after 3 months daily substitution of 25(OH) Vitamin D3, tore the anterior cruciate ligament without any external influence. VitD 30-80 ng/ml (n=111) (n=61) (n=50) Football (n=21) (n=62) Participants (n=19) (n=5) (n=4) (n=27) (n=6) (n=15) (n=6) (30-80 ng/ml) (n=111) Adults (n=24) U16 + U18 (n=21) (n=21) Adults (n=45) ± SD ± SD ± SD ± SD ± SD
Age
Infect
Muscle Injury
Total
22,34
44/111
81/111
31,1
± 7,43
(40%)
(73%)
± 10,61
Female
20,13
24/61
44/61
31,9
± 6,16
(39%)
(72%)
± 9,92
Male
25,04
20/50
37/50
30,0
± 8
(40%)
(74%)
± 11,42
22,9
5/21
17/21
32,2
± 4,05
(24%)
(81%)
± 13,29
Field hockey
19,37
22/62
45/62
31,6
± 4,62
(36%)
(73%)
± 9,99
Olympia-
29
11/19
13/19
29,6
± 10,86
(58%)
(68%)
± 10,58
Tennis
21,6
3/5
4/5
27,1
± 6,5
(60%)
(80%)
± 10,84
Motor
34,75
3/4
2/4
29,0
± 6,85
(75%)
(50%)
± 6,05
National
23,59
8/27
18/27
34,4
± 5,35
(30%)
(67%)
± 12,94
U16
13,67
1/6
5/6
29,9
± 0,82
(17%)
(83%)
± 8,04
U18
16,47
4/15
13/15
28,9
±0,64
(27%)
(87%)
± 8,32
U21
18,78
1/6
3/6
31,0
± 0,9
(17%)
(50%)
± 7,8
Vit D
Total
31,06
± 10,61
National Player
35,78*
± 12,35
National Player
28,53
± 8,2
other U18
25,71*
± 9,58
*p=0,007
Others
32,47
± 9,67
Vitamin D
Group ≤ 40 ng/ml
n
Group > 40 ng/ml
n
Odds-Ratio
Total
27,96
95
49,43
16
± 7,53
± 7,04
Infects
27,11
39
46,92
5
1,53 p=0,325
± 5,91
± 5,19
Infects (negative)
28,56
56
50,57
11
± 8,48
± 7,68
Muscle injury (positive)
27,5
74
46,31
7
4,53 p=0,007
± 7,85
± 6,71
Muscle injury (negative)
29,59
21
51,86
9
± 6,17
± 6,64
25 (OH) Vitamin D3
Therapy
Before
After
Total (N=25)
30,68
76,41
± 12,29
± 26,36
Correlation*
P=0,062
Test*
P=0,0001
Infection
30,54
59,55
± 9,70
± 2,33
N = 13
N = 2
Time*
P=0,0001
ARR
48%
Symptom*
P=0,828
No infection
30,82
77,87
± 15,06
± 27,01
(N=12)
(N=23)
Muscle injury
27,27
71,60
± 10,07
(N=18)
(N=1)
Time*
P=0,0001
ARR
68%
Symptom*
P=0,066
No muscle injury
39,43
76,60
± 13,87
± 26,90
(N=7)
(N=24)
Discussion
The prevalence rate of inadequate vitamin D supply in our study (51.4%) correlates closely with the meta-analysis published recently by Farrokhyar, et al. [37], in which 56% of the athletes examined worldwide showed inadequate supply ( < 30 ng/ml). The prevalence of inadequate vitamin D supply in other studies [30-32, 35] ranged from 51% - 91.3% of the athletes, with the average vitamin D value of the athletes (N=20969) in these studies ranging from 11.62 ± 9.24 ng/ml - 38.45 ± 16.65 ng/ml [28-36]. The average vitamin D value of the study with the most participants (N=18883): 29 ± 8 ng/ml [36] and the value of the Swiss Olympians (N=651): 30.32 ± 9.24 ng/ml [30] correlates closely with the mean value in our study (N=111): 31.06 ± 10.61 ng/ml. Adolescents with an average of 25.71 ± 9.58 ng/ml have a significantly worse vitamin D supply than A-national players (35.78 ± 12.35 ng/ml - p=0.007). The percentage of adolescent athletes in our study who are inadequately supplied with vitamin D (< 30 ng/ml) is, at 64.4%, significantly worse than that of adults (42.4% - OR = 2.46 - p < 0.023). This is confirmed by the results of Quadri, et al. [30]: 65% (234/360) of the Swiss athletes < 18 years had a vitamin D supply < 30ng/ml compared to 34% (99/192) of the athletes > 18 years (OR = 3.6), whereas the risk of suffering a vitamin D deficiency (< 20 ng/ml) is 5.18 times higher in adolescents < 18 years compared to adults in this study (95%CI 3.00 - 8.95, p < 0.0001). The reason for the significantly poorer vitamin D supply in adolescents may be the higher demand in the growth age on the one hand, and on the other hand the better average supply in A-national players may because by a more conscious diet (e.g. more fish) but also by a targeted, organisation-controlled vitamin D substitution.
A striking feature of our study is the high number of muscular injuries among top athletes (73% of all athletes), while U16 and U18 national players also experiencing muscular injuries significantly more frequently (83% of U16 and 87% of U18 athletes). The vitamin D value was significantly lower in athletes with muscular injuries (29.13 ± 9.38 ng/ml) than in athletes without muscular injuries (36.27 ± 12.09 ng/ml). There are currently no comparable studies on muscle injuries and vitamin D levels. Only Quadri et al (30) report in their study that 62.2% of Swiss Olympic athletes complained of muscular pain.
When comparing the prevalence of muscular injury in athletes with vitamin D values > 40 ng/ml against athletes with vitamin D values < 40 ng/ml, the probability of muscular injury is significantly higher for vitamin D values < 40 ng/ml than for athletes with vitamin D values > 40 ng/ml (OR=4.53, KI95% = [3.43; 5.63], p < 0.007). The influence of adequate vitamin D concentrations (>v40 ng/ml) on the TNFα concentration seems to play a decisive role. Willis, et al. [19] were able to demonstrate a significant inverse correlation of vitamin D to TNF-α concentration in 19 healthy competitive athletes, whereby according to their results vitamin D values > 40 ng/ml should be aimed for. TNF-α leads in the acute phase to an increased cellular calcium release and thus to muscle stiffness and tears and in the intermediate phase to an increase in the cellular inflammation parameter NfκB and thus to an increased macrophage reaction and thus to muscular inflammation and injury [19]. Can vitamin D value > 70 ng/ml prevent muscular injuries by lowering the TNF-α concentration in competitive sports (Figure 2)? In a placebo-controlled randomized therapy study in athletes with vitamin D deficiency (N=40: 18 ± 10 ng/ml), Owens, et al [29] achieved a significant increase in vitamin D levels in the therapy group (N=20: 46 ± 12.4 ng/ml - p < 0.005) by daily substitution of 4000 IU OH-vitaminD3 over 6 weeks and observed a significantly faster recovery from muscular injuries in the therapy group compared to the placebo group. Close, et al. [28] were able to confirm in their therapy study the improvement of muscle strength through vitamin D substitution. In this placebo-controlled randomized therapy study, a significant increase in vitamin D levels > 40 ng/ml was achieved in the verum group by daily administration of 5000 IU OH-VitaminD3 over 8 weeks. A significant increase in vitamin D values > 40 ng/ml of the 10 and 30m sprint power and the bounce power was demonstrated in the verum group compared to the placebo group [28].
Correlations between vitamin D levels and sleep disorders, fatigue or infections showed no significance, although athletes with vitamin D levels < 40 ng/ml showed a 1.53-fold higher risk of developing infections than athletes with vitamin D levels > 40 ng/ml. The Third National Health and Nutrition Examination Survey [36] seems to confirm this observation, because in this study (N=18883) a significant-inverse correlation between vitamin D concentration and upper respiratory tract infections (URTI) was found (participants with vitamin D values < 10 ng/ml developed URTI in up to 30% of cases). Internationally, a target value for vitamin D > 40 ng/ml is achieved by daily administration of 4000 - 5000 IU OH-VitaminD3.
In our 3-month treatment study (N = 25) we achieved the upper normal vitamin D-levels (76,41 ± 26,36 ng/ml) by daily
substitution of 20000 IU 25(OH)VitaminD3, thus avoiding muscle injury in 68% and a recurrent infection in 48%. Whether this can actually be achieved by lowering the TNF level or whether other biochemical processes (vitamin D-induced optimization of the intracellular influx of calcium and magnesium into the muscle) are responsible for preventing muscle injury and recurrent infections, further studies are needed to clarify. Comparable studies are not available in the current literature. Long-term studies with the preservation of blood vitamin D3 between 70-80 ng/ml have to show whether recurrent infections and muscle damages can be prevented during this time. Further studies must also show whether other micronutrient deficiencies or gene changes are responsible for the severe injury (rupture of the anterior cruciate ligament) of the athlete despite optimal vitamin D levels.

Figure 1: blood Vitamin D concentrations and standard errors before and after therapy with 20000 IU 25(OH) VitaminD3 daily for 3 months (n=25). ** = p=0.0001.
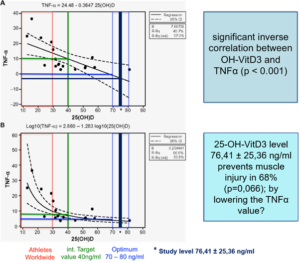
Figure 2: inverse correlation TNFα and OH-VitD3 according to Willis et al. (19) modified according to Erpenbach et al. (39) (unpublished data).
References
- Rodriguez NR, DiMarco NM, Langley S (2009) American College of Sports Medicine position stand. Nutrition and athletic p Med Sci Sports Exerc 41: 709-731.
- Kreider RB, Wilborn CD, Taylor L, Campbell B, Almada AL, et al. (2010) ISSN exercise & sport nutrition review: research & recommendations. J Int Soc Sports Nutr 7:1-43
- Walsh NP, Gleeson M, Shephard RJ, Gleeson M, Woods JA, et al. (2011) Position Part one: immune function and exercise. Exerc Immunol Rev 17: 6-63.
- Gleeson M, Pyne DB (2016) Respiratory inflammation and infections in high-performance Immunol Cell Biol 94: 124-31.
- Junge A, Engebretsen L, Mountjoy ML, Alonso JM, Renström PASH, et al. (2009) Sports injuries during the Summer Olympic Games 2008. Am J Sports Med 37: 2165-2172.
- Engebretsen L, Steffen K, Alonso JM, Aubry M, Dvorak J, et al. (2010) Sports injuries and illnesses during the Winter Olympic Games 2010. Br J Sports Med 44: 772-780.
- Engebretsen L, Soligard T, Steffen K, Alonso JM, Aubry M, et al. (2013) Sports injuries and illnesses during the London Summer Olympic Games 2012. Br J Sports Med 47: 407-414.
- Soligard T, Steffen K, Palmer-Green D, Aubry M, Grant ME, et al. (2015) Sports injuries and illnesses in the Sochi2014 Olympic Winter Games. Br J Sports Med 49: 441-447.
- Junge A, Dvorak J, Graf-Baumann T (2004) Football injuries during the World Cup 2002. Am J Sports Med 32: 23S-27S.
- Dvorak J, Junge A, Grimm K (2007) Medical report from the 2006 FIFA World CupGermany. Br J Sports Med 41: 578-581.
- Alonso JM, Tscholl PM, Engebretsen L, Mountjoy M, Dvorak J, et al. (2010) Occurrence of injuries and illnesses during the 2009 IAAF World Athletics Championships. Br J Sports Med 44: 1100-1105.
- Alonso JM, Edouard P, Fischetto G, Adams B, Depiesse F, et al. (2012) Determination of future prevention strategies in elite track and field: analysis of Daegu 2011 IAAF championships injuries and illnesses surveillance. Br J Sports Med 46: 505-514.
- Alonso JM, Jacobsson J, Timpka T, Ronsen O, Kajenienne A, et al. (2015) Pre participation injury complaint is a risk factor for injury: a prospective study of the Moscow 2013 IAAF championships. Br JSports Med 49: 1118-1124.
- Schwellnus M, Soligard T, Alonso JM, Bahr R, ClarsenB , Dijkstra HP, et al. (2016) How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness. Br J Sports Med 50: 1043-1052.
- Deakin V, Stear SJ, Shirreffs SM, Collins AL, eds: Sport and Exercise Nutrition. 1st Oxford, UK: Wiley-Blackwell; 2011: 66-88.
- Hakkiday TM, Peterson NJ, Thomas JJ, Kleppinger K, Hollis BW, et al. (2011) Vitamin D status relative to diet, lifestyle, injury and illness in college athletes. Med Sci Sports Exerc 43: 335-343.
- Ruohola JP, Laaksi I, Ylikomi T, Haataja R, Mattila VM, et al. (2006) Association between serum 25 (OH) D concentrations and bone stress fractures in Finnish young men. J Bone Miner Res 21: 1483-1488.
- Wang TT, Tavera-Menodza LE, Laperriere D, Libby E, MacLeod NB, et al. (2005) Large-scalein silico and microassay-based identification of direct 1,25-dihydroxyvitaminD3 target genes. Mol Endocrinol 19: 2685-2695.
- Willis KS, Smith DT, Broughton KS, Larson-Meyer DE (2012) Vitamin D status and biomarkers of inflammation in runners. J Sports Med 3: 35-42
- Reddy Vanga S, Good M, Howard PA, Vacek JL (2010) Role of vitamin D in cardiovascular health. Am J Cardiol 106: 798-805.
- Sukumar D, Shapes SA, Schneider SH (2015) Vitamin D supplementation during short-term caloric restriction in healthy overweight/obese older women: effect on glycemic indices and serum osteocalcin levels. Mol Cell Endocrinol 410: 1-5.
- Close GL, Leckey J, Patterson M, Bradley W, Owens DJ, et al. (2013) The effects of vitamin D(3) supplementation on serum total 25[OH]D concentration and physical performance: a randomized dose-response study. Brit J Sports Med 47: 692-696.
- Guillot X, Prati C, Wendling D (2014) Vitamin D and spondyloarthritis. Expert Rev Clin Immunol 10: 1581-1589.
- Bikle DD (2014) VItaminD metabolism, mechanism of action and clinical applications. Chem Biol 21: 319-329.
- Ogan D, Pritchett K (2013) Vitamin D and the athlete risks, recommendations and benefits. Nutrients 5: 1856-1868.
- Glerup H, Mikkelsen K, Poulsen L, Hass E, Overbeck S, et al. (2000) Hypovitaminosis D myopathy without biochemical signs of osteomalcic bone involvement. Calcif Tissue Int 66: 419-424.
- Pfeifer M, Begerow B, Minne H (2002) Vitamin D and muscle function. Osteoporos Int 3: 187-194.
- Close GL, Russell J, Cobley JN, Owens DJ, Wilson G, et al. (2012) Assessment of vitamin D concentration in non-supplemented professional athletes and healthy adults during winter months in the UK: implications for skeletal muscle function. J Sports Sciences 31: 344-353.
- Owens DJ, Sharples AP, Polydorou I, Alwan N, Donovan T, et al. (2015) A systems-based investigation into vitamin D and skeletal muscle repair, regeneration and hypertrophy. Am J Physiol Endocrinol Metab 309: 1019-1031.
- Quadri A, Gojanovic B, Noack P, Fuhrer C, Steuer C, et al. (2016) Seasonal variation og vitamin D levels in Swiss athletes. Swiss Sports & Exercise Medicine 64: 19-25.
- Sghaier-Ayadi A, Feki M, Bezrati-Ben Ayed I, Abene O, et al. (2015) Vitamin D status and determinants of deficiency in non-supplemented athletes during the winter months in Tunisia. Biol Sport 32: 281-287.
- Fishman MP, Lombardo SJ, Kharrazi FD (2016) Vitamin D Deficiency among Professional Basketball Players. Orthopedic J Sport Med 4: 1-5.
- Varamenti E, Cherif A, Nikolovski Z, Tabben M, Jamurtas AZT, et al. (2019) Exploring possible relationships between 25(OH)D deficiency and variables related to inflammation, endothelial function, and enzymatic antioxidants in adolescent athletes: a prospective study. Biol Sport 36: 113-118.
- Kryzwanski J, Mikulski T, Krysztofiak H, Mlynczak M, Gaczynska E, et al. (2016) Seasonal Vitamin D Status in Polish Elite Athletes in Relation to Sun Exposure and Oral Supplementation. PLoS ONE 11: 1-12.
- Backx EMP, Tieland M, Maase K, Kies AK, Mensink M, et al. (2016) The impact of 1-year vitamin D supplementation on vitamin D status in athletes: a dose–response study. European J Clin Nutr 70: 1009-1014.
- Ginde AA, Mansbach MPH, Camargo CA Jr (2009) Association between Serum 25-Hydroxyvitamin D Level and Upper Respiratory Tract Infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med 169: 384-390.
- Farrokhyar F, Tabasinejad R, Dao D, Peterson D, Ayeni OR, et al. (2015) Prevalence of Vitamin D inadequacy in athletes: a systemic review and meta analysis. Sports Med 45: 365-373.
- Pereira Panza VS, Diefenthaeler F, da Silva EL (2015) Benefits of dietary phytochemical supplementation on eccentric exercise-induced muscle damage: Is including antioxidants enough? Nutrition 31: 1072-1082.
- Erpenbach K, Mücke S (2017) Mitochondriale Ernährung. Sportärztezeitung 4: 88-91.